Abstract
Salicylic acid (SA) has therapeutic potential based on its anti-inflammatory and antimicrobial properties. A limitation of SA treatment is its short half-life in vivo that can be overcome by the sustained release by incorporation into a polymer backbone resulting in biodegradable salicylic acid-based poly(anhydride-esters) (SAPAE). In addition to slow release for up to 1 month, SAPAE is simple to produce and is an effective low-cost alternative to biologic factors. These properties are useful in promoting bone regeneration, particularly under situations where inflammation is enhanced by systemic conditions such as diabetes. In a rat critical size defect model, SAPAE application with bone grafting material significantly increased bone fill as assessed by micro-computed tomography (CT) and histomorphometry. While there was accelerated bone formation in the normoglycemic group, there was both accelerated and increased bone formation in diabetic rats. The increased bone formation in the diabetic group was tied to a decrease in inflammation during the period of bone formation, an increase in the number of osteoblasts, and a reduction of osteoclasts. The results suggest that SAPAE polymer can be used to accelerate and enhance bone formation in the treatment of periodontal and other craniofacial osseous defects and may be useful for the treatment of peri-implantitis, particularly in diabetic conditions.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Mahdi JG, Mahdi AJ, Mahdi AJ, Bowen ID. The historical analysis of aspirin discovery, its relation to the willow tree and antiproliferative and anticancer potential. Cell Prolif. 2006;39:147–55.
Madan RK, Levitt J. A review of toxicity from topical salicylic acid preparations. J Am Acad Dermatol. 2014;70:788–92.
Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol. 1971;231:232.
Amann R, Peskar BA. Anti-inflammatory effects of aspirin and sodium salicylate. Eur J Pharmacol. 2002;447:1–9.
Cottrell J, O’Connor JP. Effect of non-steroidal anti-inflammatory drugs on bone healing. Pharmaceuticals. 2010;3:1668–93.
Higgs GA, Salmon JA, Henderson B, Vane JR. Pharmacokinetics of aspirin and salicylate in relation to inhibition of arachidonate cyclooxygenase and antiinflammatory activity. Proc Natl Acad Sci U S A. 1987;84:1417–20.
Mitchell JA, Saunders M, Barnes PJ, Newton R, Belvisi MG. Sodium salicylate inhibits Cyclo-Oxygenase-2 activity independently of transcription factor (nuclear factor κB) activation: role of arachidonic acid. Mol Pharmacol. 1997;51:907.
Ping M, Zizhen L, Meng X, Rui J, Weirui L, Xiaohong W, Shen M, Gaimei S. Naturally occurring methyl salicylate glycosides. Mini-Rev Med Chem. 2014;14:56–63.
Rowland M, Riegelman S. Pharmacokinetics of acetylsalicylic acid and salicylic acid after intravenous administration in man. J Pharm Sci. 1968;57:1313–9.
Prudencio A, Schmeltzer RC, Uhrich KE. Effect of linker structure on salicylic acid-derived poly(anhydride−esters). Macromolecules. 2005;38:6895–901.
Faig Jonathan J, Smith K, Moretti A, Yu W, Uhrich Kathryn E. One-pot polymerization syntheses: incorporating bioactives into poly(anhydride-esters). Macromol Chem Phys. 2016;217:1842–50.
Carbone Ashley L, Uhrich Kathryn E. Design and synthesis of fast-degrading poly(anhydride-esters). Macromol Rapid Commun. 2009;30:1021–6.
Whitaker-Brothers K, Uhrich K. Poly(anhydride-ester) fibers: role of copolymer composition on hydrolytic degradation and mechanical properties. J Biomed Mater Res A. 2004;70A:309–18.
Griffin J, Delgado-Rivera R, Meiners S, Uhrich KE. Salicylic acid-derived poly(anhydride-ester) electrospun fibers designed for regenerating the peripheral nervous system. J Biomed Mat Res A. 2011;97:230–42.
Subramanian S, Mitchell A, Yu W, Snyder S, Uhrich K, O'Connor JP. Salicylic acid-based polymers for guided bone regeneration using bone morphogenetic Protein-2. Tissue Eng Part A. 2015;21:2013–24.
Demirdirek B, Uhrich KE. Physically crosslinked salicylate-based poly (N-isopropylacrylamide-co-acrylic acid) hydrogels for protein delivery. J Bioact Compat Polym. 2018;33:224–36.
Demirdirek B, Uhrich KE. Novel salicylic acid-based chemically crosslinked pH-sensitive hydrogels as potential drug delivery systems. Int J Pharm. 2017;528:406–15.
Demirdirek B, Uhrich KE. Salicylic acid-based pH-sensitive hydrogels as potential oral insulin delivery systems. J Drug Target. 2015;23:716–24.
Ouimet MA, Fogaca R, Snyder SS, Sathaye S, Catalani LH, Pochan DJ, Uhrich KE. Poly(anhydride-ester) and poly(N-vinyl-2-pyrrolidone) blends: salicylic acid-releasing blends with hydrogel-like properties that reduce inflammation. Macromol Biosci. 2015;15:342–50.
Yu W, Bien-Aime S, Li J, Zhang L, McCormack ES, Goldberg ID, Narayan P, Uhrich KE. Injectable microspheres for extended delivery of bioactive insulin and salicylic acid. J Bioact Compat Polym. 2015;30:340–6.
Delgado-Rivera R, Rosario-Melendez R, Yu W, Uhrich KE. Biodegradable salicylate-based poly(anhydride-ester) microspheres for controlled insulin delivery. J Biomed Mat Res A. 2014;102:2736–42.
Rosario-Meléndez R, Ouimet M, Uhrich K. Formulation of salicylate-based poly(anhydride-ester) microspheres for short- and long-term salicylic acid delivery. Polym Bull. 2013;70:343–51.
Díez S, Tros de Ilarduya C. Versatility of biodegradable poly(d,l-lactic-co-glycolic acid) microspheres for plasmid DNA delivery. Eur J Pharm Biopharm. 2006;63:188–97.
Stebbins ND, Faig JJ, Yu W, Guliyev R, Uhrich KE. Polyactives: controlled and sustained bioactive release via hydrolytic degradation. Biomater Sci. 2015;3:1171–87.
Elgali I, Omar O, Dahlin C, Thomsen P. Guided bone regeneration: materials and biological mechanisms revisited. Eur J Oral Sci. 2017;125:315–37.
Simon AM, Manigrasso MB, O'Connor JP. Cyclo-oxygenase 2 function is essential for bone fracture healing. J Bone Miner Res. 2002;17:963–76.
Sri B, Vadithya A, Chatterjee A. As a review on hydrogels as drug delivery in the pharmaceutical field. Int J Pharm Chem Sci. 2012;1:642–61.
Peppas NA, Huang Y, Torres-Lugo M, Ward JH, Zhang J. Physicochemical foundations and structural design of hydrogels in medicine and biology. Annu Rev Biomed Eng. 2000;2:9–29.
Lopérgolo LC, Lugão AB, Catalani LH. Direct UV photocrosslinking of poly(N-vinyl-2-pyrrolidone) (PVP) to produce hydrogels. Polymer. 2003;44:6217–22.
Lin C-C, Metters AT. Hydrogels in controlled release formulations: network design and mathematical modeling. Adv Drug Deliv Rev. 2006;58:1379–408.
Park H, Park K. Hydrogels in bioapplications. In: Hydrogels and Biodegradable Polymers for Bioapplications. Washington, DC: American Chemical Society; 1996. p. 2–10.
Kipper MJ, Shen E, Determan A, Narasimhan B. Design of an injectable system based on bioerodible polyanhydride microspheres for sustained drug delivery. Biomaterials. 2002;23:4405–12.
Whitaker-Brothers K, Uhrich K. Investigation into the erosion mechanism of salicylate-based poly(anhydride-esters). J Biomed Mat Res A. 2006;76:470–9.
Keith CT, Borisy AA, Stockwell BR. Multicomponent therapeutics for networked systems. Nat Rev Drug Discov. 2005;4:71.
Kumar CG, Anand SK. Significance of microbial biofilms in food industry: a review. Int J Food Microbiol. 1998;42:9–27.
Perilli R, Marziano ML, Formisano G, Caiazza S, Scorcia G, Baldassarri L. Alteration of organized structure of biofilm formed by Staphylococcus epidermidis on soft contact lenses. J Biomed Mater Res. 2000;49:53–7.
Phan TN, Reidmiller JS, Marquis RE. Sensitization of actinomyces naeslundii and streptococcus sanguis biofilms and suspensons to acid damage by fluoride and other weak acids. Arch Microbiol. 2000;174(4):248–55.
Muller E, Al-Attar J, Wolff AG, Farber BF. Mechanism of salicylate-mediated inhibition of biofilm in Staphylococcus epidermidis. J Infect Dis. 1998;177:501–3.
Brown MRW, Allison DG, Gilbert P. Resistance of bacterial biofilms to antibiotics a growth-rate related effect? J Antimicrob Chemother. 1988;22:777–80.
Dunne WM Jr, Mason EO Jr, Kaplan SL. Diffusion of rifampin and vancomycin through a Staphylococcus epidermidis biofilm. Antimicrob Agents Chemother. 1993;37:2522–6.
Arciola C, Montanaro L, Caramazza R, Sassoli V, Cavedagna D. Inhibition of bacterial adherence to a high-water-content polymer by a water-soluble, nonsteroidal, anti-inflammatory drug. J Biomed Mater Res. 1998;42(1):1–5.
Bryers JD, Jarvis RA, Lebo J, Prudencio A, Kyriakides TR, Uhrich K. Biodegradation of poly(anhydride-esters) into non-steroidal anti-inflammatory drugs and their effect on Pseudomonas aeruginosa biofilms in vitro and on the foreign-body response in vivo. Biomaterials. 2006;27:5039–48.
Rosenberg L, Carbone A, Römling U, Uhrich K, Chikindas M. Salicylic acid-based poly (anhydride esters) for control of biofilm formation in Salmonella enterica serovar typhimurium. Lett Appl Microbiol. 2008;46:593–9.
Vane J, Botting R. Inflammation and the mechanism of action of anti-inflammatory drugs. FASEB J. 1987;1:89–96.
Erdmann L, Macedo B, Uhrich K. Degradable poly (anhydride ester) implants: effects of localized salicylic acid release on bone. Biomaterials. 2000;21:2507–12.
Mitchell A, Kim B, Cottrell J, Snyder S, Witek L, Ricci J, Uhrich KE, O’Connor JP. Development of a guided bone regeneration device using salicylic acid-poly(anhydride-ester) polymers and osteoconductive scaffolds. J Biomed Mat Res A. 2014;102:655–64.
Mitchell A, Kim B, Snyder S, Subramanian S, Uhrich K, O’Connor JP. Use of salicylic acid polymers and bone morphogenetic protein-2 to promote bone regeneration in rabbit parietal bone defects. J Bioact Compat Polym. 2015;31:140–51.
Yunus Basha R, Sampath Kumar TS, Doble M. Design of biocomposite materials for bone tissue regeneration. Mater Sci Eng C. 2015;57:452–63.
Dorj B, Won J-E, Purevdorj O, Patel KD, Kim J-H, Lee E-J, Kim H-W. A novel therapeutic design of microporous-structured biopolymer scaffolds for drug loading and delivery. Acta Biomater. 2014;10:1238–50.
Quinlan E, Thompson EM, Matsiko A, O’Brien FJ, López-Noriega A. Functionalization of a collagen–hydroxyapatite scaffold with osteostatin to facilitate enhanced bone regeneration. Adv Healthc Mater. 2015;4:2649–56.
Sutherland AJ, Detamore MS. Bioactive microsphere-based scaffolds containing decellularized cartilage. Macromol Biosci. 2015;15:979–89.
Kim B-S, Kim J-S, Yang S-S, Kim H-W, Lim HJ, Lee J. Angiogenin-loaded fibrin/bone powder composite scaffold for vascularized bone regeneration. Biomat Res. 2015;19:18.
Retzepi M, Lewis MP, Donos N. Effect of diabetes and metabolic control on de novo bone formation following guided bone regeneration. Clin Oral Implants Res. 2010;21:71–9.
Ramanujam CL, Facaros Z, Zgonis T. An overview of bone grafting techniques for the diabetic charcot foot and ankle. Clin Podiatr Med Surg. 2012;29:589.
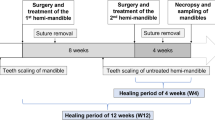
Wada K, Yu W, Elazizi M, Barakat S, Ouimet MA, Rosario-Meléndez R, Fiorellini JP, Graves DT, Uhrich KE. Locally delivered salicylic acid from a poly(anhydride-ester) impact on diabetic bone regeneration. J Control Release. 2013;171:33–7.
Yu W, Bien-Aime S, Mattos M, Alsadun S, Wada K, Rogado S, Fiorellini J, Graves D, Uhrich K. Sustained, localized salicylic acid delivery enhances diabetic bone regeneration via prolonged mitigation of inflammation. J Biomed Mat Res A. 2016;104:2595–603.
Liu R, Bal HS, Desta T, Behl Y, Graves DT. Tumor necrosis factor-alpha mediates diabetes-enhanced apoptosis of matrix-producing cells and impairs diabetic healing. Am J Pathol. 2006;168:757–64.
Pacios S, Andriankaja O, Kang J, Alnammary M, Bae J, de Brito Bezerra B, Schreiner H, Fine DH, Graves DT. Bacterial infection increases periodontal bone loss in diabetic rats through enhanced apoptosis. Am J Pathol. 2013;183:1928–35.
Xiao W, Li S, Pacios S, Wang Y, Graves DT. Bone remodeling under pathological conditions. Front Oral Biol. 2016;18:17–27.
Pacios S, Kang J, Galicia J, Gluck K, Patel H, Ovaydi-Mandel A, Petrov S, Alawi F, Graves DT. Diabetes aggravates periodontitis by limiting repair through enhanced inflammation. FASEB J. 2012;26:1423–30.
Liu R, Bal HS, Desta T, Krothapalli N, Alyassi M, Luan Q, Graves DT. Diabetes enhances periodontal bone loss through enhanced resorption and diminished bone formation. J Dent Res. 2006;85:510–4.
Kang J, de Brito Bezerra B, Pacios S, Andriankaja O, Li Y, Tsiagbe V, Schreiner H, Fine DH, Graves DT. Aggregatibacter actinomycetemcomitans infection enhances apoptosis in vivo through a caspase-3-dependent mechanism in experimental periodontitis. Infect Immun. 2012;80:2247–56.
Simmons DJ. Fracture healing perspectives. Clin Orthop Relat Res. 1985;200:100–13.
Zhang X, Kohli M, Zhou Q, Graves DT, Amar S. Short- and long-term effects of IL-1 and TNF antagonists on periodontal wound healing. J Immunol. 2004;173:3514–23.
Panda H. Handbook on drugs from natrual sources. New Delhi: Asia Pacific Business Press Inc.; 2010.
Mountziaris PM, Mikos AG. Modulation of the inflammatory response for enhanced bone tissue regeneration. Tissue Eng Part B Rev. 2008;14:179–86.
Mountziaris PM, Spicer PP, Kasper FK, Mikos AG. Harnessing and modulating inflammation in strategies for bone regeneration. Tissue Eng Part B Rev. 2011;17:393–402.
Brugger OE, Bornstein MM, Kuchler U, Janner SF, Chappuis V, Buser D. Implant therapy in a surgical specialty clinic: an analysis of patients, indications, surgical procedures, risk factors, and early failures. Int J Oral Maxillofac Implants. 2015;30:151–60.
Claffey N, Clarke E, Polyzois I, Renvert S. Surgical treatment of peri-implantitis. J Clin Periodontol. 2008;35:316–32.
Schwarz F, Jepsen S, Herten M, Sager M, Rothamel D, Becker J. Influence of different treatment approaches on non-submerged and submerged healing of ligature induced peri-implantitis lesions: an experimental study in dogs. J Clin Periodontol. 2006;33:584–95.
Derks J, Schaller D, Hakansson J, Wennstrom JL, Tomasi C, Berglundh T. Effectiveness of implant therapy analyzed in a Swedish population: prevalence of peri-implantitis. J Dent Res. 2016;95:43–9.
Tarnow DP. Increasing prevalence of peri-implantitis: how will we manage? J Dent Res. 2016;95:7–8.
Sanz M, Chapple IL, V. E. W. o. P. Working Group 4 of the. Clinical research on peri-implant diseases: consensus report of working group 4. J Clin Periodontol. 2012;39(Suppl 12):202–6.
Mellado Valero A, Ferrer García JC, Herrera Ballester A, Labaig Rueda C. Effects of diabetes on the osseointegration of dental implants. Med Oral Patol Oral Cir Bucal (Internet). 2007;12:38–43.
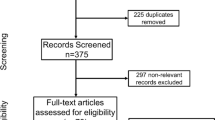
Camargo WA, de Vries R, van Luijk J, Hoekstra JW, Bronkhorst EM, Jansen JA, van den Beucken JJ. Diabetes mellitus and bone regeneration: a systematic review and meta-analysis of animal studies. Tissue Eng Part B Rev. 2017;23:471–9.
Genuth S, Alberti K, Bennett P, Buse J, DeFronzo R, Kahn R, Kitzmiller J, Knowler WC, Lebovitz H, Lernmark A. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care. 2003;26:3160–8.
Chrcanovic BR, Albrektsson T, Wennerberg A. Diabetes and oral implant failure: a systematic review. J Dent Res. 2014;93:859–67.
Oates TW, Dowell S, Robinson M, McMahan CA. Glycemic control and implant stabilization in type 2 diabetes mellitus. J Dent Res. 2009;88:367–71.
von Wilmowsky C, Stockmann P, Harsch I, Amann K, Metzler P, Lutz R, Moest T, Neukam FW, Schlegel KA. Diabetes mellitus negatively affects peri-implant bone formation in the diabetic domestic pig. J Clin Periodontol. 2011;38:771–9.
Coelho PG, Pippenger B, Tovar N, Koopmans SJ, Plana NM, Graves DT, Engebretson S, van Beusekom HMM, Oliveira P, Dard M. Effect of obesity or metabolic syndrome and diabetes on osseointegration of dental implants in a miniature swine model: a pilot study. J Oral Maxillofac Surg. 2018;76:1677–87.
Abduljabbar T, Al-Sahaly F, Kellesarian SV, Kellesarian TV, Al-Anazi M, Al-Khathami M, Javed F, Vohra F. Comparison of peri-implant clinical and radiographic inflammatory parameters and whole salivary destructive inflammatory cytokine profile among obese and non-obese men. Cytokine. 2016;88:51–6.
Daubert DM, Weinstein BF, Bordin S, Leroux BG, Flemming TF. Prevalence and predictive factors for peri-implant disease and implant failure: a cross-sectional analysis. J Periodontol. 2015;86:337–47.
Elangovan S, Brogden KA, Dawson DV, Blanchette D, Pagan-Rivera K, Stanford CM, Johnson GK, Recker E, Bowers R, Haynes WG, Avila-Ortiz G. Body fat indices and biomarkers of inflammation: a cross-sectional study with implications for obesity and peri-implant oral health. Int J Oral Maxillofac Implants. 2014;29:1429–34.
Vohra F, Alkhudhairy F, Al-Kheraif AA, Akram Z, Javed F. Peri-implant parameters and C-reactive protein levels among patients with different obesity levels. Clin Implant Dent Relat Res. 2018;20:130–6.
Li Y, Lu Z, Zhang X, Yu H, Kirkwood KL, Lopes-Virella MF, Huang Y. Metabolic syndrome exacerbates inflammation and bone loss in periodontitis. J Dent Res. 2015;94:362–70.
Wu YY, Xiao E, Graves DT. Diabetes mellitus related bone metabolism and periodontal disease. Int J Oral Sci. 2015;7:63–72.
Napoli N, Chandran M, Pierroz DD, Abrahamsen B, Schwartz AV, Ferrari SL, Bone IOF, Diabetes Working G. Mechanisms of diabetes mellitus-induced bone fragility. Nat Rev Endocrinol. 2017;13:208–19.
Graves DT, Alshabab A, Albiero ML, Mattos M, Correa JD, Chen S, Yang Y. Osteocytes play an important role in experimental periodontitis in healthy and diabetic mice through expression of RANKL. J Clin Periodontol. 2018;45:285–92.
Alharbi MA, Zhang C, Lu C, Milovanova TN, Yi L, Ryu JD, Jiao H, Dong G, O'Connor JP, Graves DT. FOXO1 deletion reverses the effect of diabetic-induced impaired fracture healing. Diabetes. 2018;67:2682–94.
Xiao E, Mattos M, Vieira GHA, Chen S, Correa JD, Wu Y, Albiero ML, Bittinger K, Graves DT. Diabetes enhances IL-17 expression and alters the oral microbiome to increase its pathogenicity. Cell Host Microbe. 2017;22:120–128.e124.
Zhou M, Rong R, Munro D, Zhu C, Gao X, Zhang Q, Dong Q. Investigation of the effect of type 2 diabetes mellitus on subgingival plaque microbiota by high-throughput 16S rDNA pyrosequencing. PLoS One. 2013;8:e61516.
Saeb ATM, Al-Rubeaan KA, Aldosary K, Udaya Raja GK, Mani B, Abouelhoda M, Tayeb HT. Relative reduction of biological and phylogenetic diversity of the oral microbiota of diabetes and pre-diabetes patients. Microb Pathog. 2019;128:215–29.
Sabharwal A, Ganley K, Miecznikowski JC, Haase EM, Barnes V, Scannapieco FA. The salivary microbiome of diabetic and non-diabetic adults with periodontal disease. J Periodontol. 2019;90:26–34.
Ussar S, Fujisaka S, Kahn CR. Interactions between host genetics and gut microbiome in diabetes and metabolic syndrome. Mol Metab. 2016;5:795–803.
Griffen AL, Beall CJ, Campbell JH, Firestone ND, Kumar PS, Yang ZK, Podar M, Leys EJ. Distinct and complex bacterial profiles in human periodontitis and health revealed by 16S pyrosequencing. ISME J. 2012;6:1176–85.
Mahato N, Wu X, Wang L. Management of peri-implantitis: a systematic review, 2010-2015. Springerplus. 2016;5:105.
Persson LG, Berglundh T, Lindhe J, Sennerby L. Re-osseointegration after treatment of peri-implantitis at different implant surfaces. An experimental study in the dog. Clin Oral Implants Res. 2001;12:595–603.
Renvert S, Quirynen M. Risk indicators for peri-implantitis. A narrative review. Clin Oral Implants Res. 2015;26(Suppl 11):15–44.
Venza I, Visalli M, Cucinotta M, De Grazia G, Teti D, Venza M. Proinflammatory gene expression at chronic periodontitis and peri-implantitis sites in patients with or without type 2 diabetes. J Periodontol. 2010;81:99–108.
Erdmann L, Uhrich K. Synthesis and degradation characteristics of salicylic acid-derived poly (anhydride-esters). Biomaterials. 2000;21:1941–6.
Housby JN, Cahill CM, Chu B, Prevelige R, Bickford K, Stevenson MA, Calderwood SK. Non-steroidal anti-inflammatory drugs inhibit the expression of cytokines and induce HSP70 in human monocytes. Cytokine. 1999;11:347–58.
Fujita D, Yamashita N, Iita S, Amano H, Yamada S, Sakamoto K. Prostaglandin E2 induced the differentiation of osteoclasts in mouse osteoblast-depleted bone marrow cells. Prostaglandins Leukot Essent Fat Acids. 2003;68:351–8.
Gruber R, Karreth F, Fischer M, Watzek G. Platelet-released supernatants stimulate formation of osteoclast-like cells through a prostaglandin/RANKL-dependent mechanism. Bone. 2002;30:726–32.
Lader C, Flanagan A. Prostaglandin E2, interleukin 1α, and tumor necrosis factor-α increase human osteoclast formation and bone resorption in vitro 1. Endocrinology. 1998;139:3157–64.
Okada Y, Lorenzo JA, Freeman AM, Tomita M, Morham SG, Raisz LG, Pilbeam CC. Prostaglandin G/H synthase-2 is required for maximal formation of osteoclast-like cells in culture. J Clin Investig. 2000;105:823.
Carbone-Howell AL, Stebbins ND, Uhrich KE. Poly(anhydride-esters) comprised exclusively of naturally occurring antimicrobials and EDTA: antioxidant and antibacterial activities. Biomacromolecules. 2014;15:1889–95.
Rosenberg LE, Carbone AL, Romling U, Uhrich KE, Chikindas ML. Salicylic acid-based poly(anhydride esters) for control of biofilm formation in Salmonella enterica serovar typhimurium. Lett Appl Microbiol. 2008;46:593–9.
Sanz-Martin I, Doolittle-Hall J, Teles RP, Patel M, Belibasakis GN, Hammerle CHF, Jung RE, Teles FRF. Exploring the microbiome of healthy and diseased peri-implant sites using Illumina sequencing. J Clin Periodontol. 2017;44:1274–84.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Graves, D., Cao, Y., Coelho, P., Witek, L., Uhrich, K. (2020). Salicylic Acid Polymers in Periodontal Tissue Healing. In: Sahingur, S. (eds) Emerging Therapies in Periodontics. Springer, Cham. https://doi.org/10.1007/978-3-030-42990-4_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-42990-4_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-42989-8
Online ISBN: 978-3-030-42990-4
eBook Packages: MedicineMedicine (R0)