Abstract
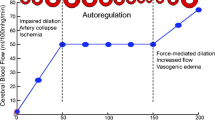
The exact etiology of cardiopulmonary bypass (CPB)-associated morbidity and mortality remains unclear and is probably multifactorial resulting from the interactions of a variety of mechanisms: alterations in blood flow, activation of inflammatory processes, temperature manipulations, and emboli. Brain injury, regardless of etiology, can lead to brain edema, further exacerbating the injury.1
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Harris DN, Bailey SM, Smith PL, Taylor KM, Oatridge A, Bydder GM. Brain swelling in first hour after coronary artery bypass surgery [see comments]. Lancet. 1993;342(8871):586-587.
Padayachee TS, Parsons S, Theobold R, Linley J, Gosling RG, Deverall PB. The detection of microemboli in the middle cerebral artery during cardiopulmonary bypass: a transcranial Doppler ultrasound investigation using membrane and bubble oxygenators. Ann Thorac Surg. 1987;44(3):298-302.
Blauth C, Smith P, Newman S, et al. Retinal microembolism and neuropsychological deficit following clinical cardiopulmonary bypass: comparison of a membrane and a bubble oxygenator. A preliminary communication. Eur J Cardio-Thorac Surg. 1989;3(2):135-138. discussion 139.
Kurusz M. Gaseous microemboli: sources, causes, and clinical considerations. Med Instrument. 1985;19:73-75.
Clark RE, Brillman J, Davis DA, Lovell MR, Price TR, Magovern GJ. Microemboli during coronary artery bypass grafting. Genesis and effect on outcome [see comments]. J Thorac Cardiovasc Sur. 1995;109(2):249-257. discussion 257-248.
Pugsley W, Klinger L, Paschalis C, Treasure T, Harrison M, Newman S. The impact of microemboli during cardiopulmonary bypass on neuropsychological functioning. Stroke. 1994;25(7):1393-1399.
Hammon JW Jr, Stump DA, Kon ND, et al. Risk factors and solutions for the development of neurobehavioral changes after coronary artery bypass grafting. Ann Thorac Surg. 1997;63(6):1613-1618.
Butler BD, Kurusz M. Embolic Events. In: Gravlee GP, Davis RF, Kurusz M, Utley J, eds. Cardiopulmonary Bypass: Principles and Practice. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:320-341.
Williams IM. Intravascular changes in the retina during open-heart surgery. Lancet. 1971;2(7726):688-691.
Williams IM. Retinal vascular occlusions in open heart surgery. Brit J Ophthalmol. 1975;59(2):81-91.
Blauth C, Arnold J, Kohner EM, Taylor KM. Retinal microembolism during cardiopulmonary bypass demonstrated by fluorescein angiography. Lancet. 1986;2(8511):837-839.
Blauth CI, Smith PL, Arnold JV, Jagoe JR, Wootton R, Taylor KM. Influence of oxygenator type on the prevalence and extent of microembolic retinal ischemia during cardiopulmonary bypass Assessment by digital image analysis. J Thorac Cardiovasc Sur. 1990;99(1):61-69.
Blauth CI, Arnold JV, Schulenberg WE, McCartney AC, Taylor KM. Cerebral microembolism during cardiopulmonary bypass Retinal microvascular studies in vivo with fluorescein angiography. J Thorac Cardiovasc Surg. 1988;95(4):668-676.
Pugsley W. The use of Doppler ultrasound in the assessment of microemboli during cardiac surgery. Perfusion. 1989;4:115-122.
Stump DA, Stein CS, Tegeler CH, et al. Validity and reliability of a device for detecting carotid emboli. J Neuroimag. 1991;1:18-22.
Deal DD, Stump DA, Brooker MD. Ultrasonic monitoring for emboli in the operating room: errors of detection. J Neuroimag. 1997;7:254 (Abstract).
Trivedi UH, Patel RL, Turtle MR, Venn GE, Chambers DJ. Relative changes in cerebral blood flow during cardiac operations using xenon-133 clearance versus transcranial Doppler sonography [see comments] [published erratum appears in Ann Thorac Surg 1997 Oct;64(4):1228]. Ann Thorac Surg. 1997;63(1):167-174.
van der Linden J, Casimir-Ahn H. When do cerebral emboli appear during open heart operations? A transcranial Doppler study [see comments]. Ann Thorac Surg. 1991;51(2):237-241.
Stump DA, Rogers AT, Hammon JW, Newman SP. Cerebral emboli and cognitive outcome after cardiac surgery. J Cardiothorac Vasc Anesth. 1996;10(1):113-118. quiz 118-119.
Yao FS, Barbut D, Hager DN, Trifiletti RR, Gold JP. Detection of aortic emboli by transesophageal echocardiography during coronary artery bypass surgery. J Cardiothorac Vasc Anest. 1996;10(3):314-317.
Mitchell SJ, Willcox T, McDougal C, Gorman DF. Emboli generation by the Medtronic Maxima hard-shell adult venous reservoir in cardiopulmonary bypass circuits: a preliminary report. Perfusion. 1996;11(2):145-155.
Taylor RL, Borger MA, Weisel RD, Fedorko L, Feindel CM. Cerebral microemboli during cardiopulmonary bypass: increased emboli during perfusionist interventions. Ann Thorac Surg. 1999;68(1):89-93.
Duff HJ, Buda AJ, Kramer R, Strauss HD, David TE, Berman ND. Detection of entrapped intracardiac air with intraoperative echocardiography. Am J Cardiol. 1980;46(2):255-260.
Oka Y, Moriwaki KM, Hong Y, et al. Detection of air emboli in the left heart by M-Mode transesophageal echocardiography following cardiopulmonary bypass. Anesthesiology. 1985;63:109-113.
Oka Y, Inoue T, Hong Y, Sisto DA, Strom JA, Frater RW. Retained intracardiac air. Transesophageal echocardiography for definition of incidence and monitoring removal by improved techniques. J Thorac Cardiovasc Surg. 1986;91(3):329-338.
Moody DM, Bell MA, Challa VR, Johnston WE, Prough DS. Brain microemboli during cardiac surgery or aortography [see comments]. Ann Neurol. 1990;28(4):477-486.
Brown WR, Moody DM, Challa VR, Stump DA. Histologic studies of brain microemboli in humans and dogs after cardiopulmonary bypass. Echocard J Cardiovasc Ultra Allied Technol. 1996;13(5):559-565.
Challa VR, Moody DM, Troost BT. Brain embolic phenomena associated with cardiopulmonary bypass. J Neurol Sci. 1993;117(1-2):224-231.
Moody DM, Brown WR, Challa VR, Stump DA, Reboussin DM, Legault C. Brain microemboli associated with cardiopulmonary bypass: a histologic and magnetic resonance imaging study. Ann Thorac Surg. 1995;59(5):1304-1307.
Libman RB, Wirkowski E, Neystat M, Barr W, Gelb S, Graver M. Stroke associated with cardiac surgery. Determinants, timing, and stroke subtypes. Arch Neurol. 1997;54(1):83-8.
Aberg T, Ronquist G, Tyden H, et al. Adverse effects on the brain in cardiac operations as assessed by biochemical, psychometric, and radiologic methods. J Thorac Cardiovasc Surg. 1984;87(1):99-105.
Muraoka R, Yokota M, Aoshima M, et al. Subclinical changes in brain morphology following cardiac operations as reflected by computed tomographic scans of the brain. J Thorac Cardiovasc Surg. 1981;81(3):364-369.
Steinberg GK, De La Paz R, Mitchell RS, Bell TE, Albers GW. MR and cerebrospinal fluid enzymes as sensitive indicators of subclinical cerebral injury after open-heart valve replacement surgery. Am J Neuroradiol. 1996;17(2):205-212. discussion 213-205.
Simonson TM, Yuh WT, Hindman BJ, Embrey RP, Halloran JI, Behrendt DM. Contrast MR of the brain after high-perfusion cardiopulmonary bypass. Am J Neuroradiol. 1994;15(1):3-7.
Vik A, Brubakk AO, Rinck PA, Sande E, Levang OW, Sellevold O. MRI: a method to detect minor brain damage following coronary bypass surgery? Neuroradiology. 1991; 33(5):396-398.
Sellman M, Hindmarsh T, Ivert T, Semb BK. Magnetic resonance imaging of the brain before and after open heart operations [see comments]. Ann Thorac Surg. 1992;53(5):807-812.
Marochnik S, Alexandrov AV, Anthone D, Lewin C, Caldwell CB, Pullicino PM. Feasibility of SPECT for studies of brain perfusion during cardiopulmonary bypass. J Neuroimag. 1996;6(4):243-245.
Krull F, Latta K, Hoyer PF, Ziemer G, Kallfelz HC. Cerebral ultrasonography before and after cardiac surgery in infants. Pediatr Cardiol. Jul-Aug 1994;15(4):159-162.
Stump DA, Kon NA, Rogers AT, Hammon JW. Emboli and neuropsychological outcome following cardiopulmonary bypass. Echocardiography. 1996;13:1.
Schmidt R, Fazekas F, Offenbacher H, et al. Brain magnetic resonance imaging in coronary artery bypass grafts: a pre- and postoperative assessment. Neurology. Apr 1993; 43(4):775-778.
Toner I, Hamid SK, Peden CJ, Taylor KM, Smith PL. Magnetic resonance imaging and P300 (event-related auditory evoked potentials) in the assessment of postoperative cerebral injury following coronary artery bypass graft surgery. Perfusion. 1993;8(4):321-329.
McConnell JR, Fleming WH, Chu WK, et al. Magnetic resonance imaging of the brain in infants and children before and after cardiac surgery. A prospective study [see comments]. Am J Dis Child. 1990;144(3):374-378.
Mintorovitch J, Moseley ME, Chileuitt L, Shimizu H, Cohen Y, Weinstein PR. Comparison of diffusion- and T2-weighted MRI for the early detection of cerebral ischemia and reperfusion in rats. Magn Reson Med. 1991;18(1):39-50.
Moseley ME, Cohen Y, Mintorovitch J, et al. Early detection of regional cerebral ischemia in cats: comparison of diffusion- and T2-weighted MRI and spectroscopy. Magn Reson Med. May 1990;14(2):330-346.
Marks MP, de Crespigny A, Lentz D, Enzmann DR, Albers GW, Moseley ME. Acute and chronic stroke: navigated spin-echo diffusion-weighted MR imaging [published erratum appears in Radiology 1996 Jul;200(1):289]. Radiology. 1996;199(2):403-408.
Lutsep HL, Albers GW, DeCrespigny A, Kamat GN, Marks MP, Moseley ME. Clinical utility of diffusion-weighted magnetic resonance imaging in the assessment of ischemic stroke [see comments]. Ann Neurol. 1997;41(5):574-580.
Warach S, Dashe JF, Edelman RR. Clinical outcome in ischemic stroke predicted by early diffusion-weighted and perfusion magnetic resonance imaging: a preliminary analysis. J Cereb Blood Flow Metab. Jan 1996;16(1):53-59.
Baird DL, Murkin JM, Lee DL. Neurologic findings in coronary artery bypass patients: perioperative or preexisting? J Cardiothorac Vasc Anesth. 1997;11(6):694-698.
Siewert B, Schlaug G, Edelman RR, Warach S. Comparison of EPISTAR and T2*-weighted gadolinium-enhanced perfusion imaging in patients with acute cerebral ischemia. Neurology. Mar 1997;48(3):673-679.
Brant-Zawadzki M, Weinstein P, Bartkowski H, Moseley M. MR imaging and spectroscopy in clinical and experimental cerebral ischemia: a review. Am J Roentgenol. Mar 1987; 148(3):579-588.
Frahm J, Bruhn H, Gyngell ML, Merboldt KD, Hanicke W, Sauter R. Localized high-resolution proton NMR spectroscopy using stimulated echoes: initial applications to human brain in vivo. Magn Reson Med. Jan 1989;9(1):79-93.
Graham GD, Blamire AM, Howseman AM, et al. Proton magnetic resonance spectroscopy of cerebral lactate and other metabolites in stroke patients. Stroke. Mar 1992;23(3):333-340.
Gillard JH, Barker PB, van Zijl PC, Bryan RN, Oppenheimer SM. Proton MR spectroscopy in acute middle cerebral artery stroke. Am J Neuroradiol. May 1996;17(5):873-886.
Bruhn H, Frahm J, Gyngell ML, Merboldt KD, Hanicke W, Sauter R. Cerebral metabolism in man after acute stroke: new observations using localized proton NMR spectroscopy. Magn Reson Med. Jan 1989;9(1):126-131.
Ehrenhaft JL, Claman MA, Layton JM, Zimmerman GR. Cerebral complications of open-heart surgery. J Thorac Cardiovasc Surg. 1961;41:503-508.
Lindberg DA, Lucas FV, Sheagren J, Malm JR. Silicone embolization during clinical and experimental heart surgery employing a bubble oxygenator. Am J Pathol. 1961;39:129-144.
Miller JA, Fonkalsrud EW, Harrison LL, Maloney JV. Fat embolism associated with extracorporeal circulation and blood transfusion. Surgery. 1962;51:448-451.
Osborn JJ, Swank RL, Hill JD, Aguilar MJ, Gerbode F. Clinical use of a Dacron wool filter during perfusion for open-heart surgery. J Thorac Cardiovasc Surg. 1970;60:575-581.
Loop FD, Szabo J, Rowlinson RD, Urbanek K. Events related to microembolism during extracorporeal perfusion in man: effectiveness of in-line filtration recorded by ultrasound. Ann Thorac Surg. 1976;21:412-420.
Padayachee TS, Parsons S, Theobold R, Gosling RG, Deverall PB. The effect of arterial filtration on reduction of gaseous microemboli in the middle cerebral artery during cardiopulmonary bypass. Ann Thorac Surg. 1988;45(6):647-649.
Whitaker DC, Newman SP, Stygall J, Hope-Wynne C, Harrison MJG, Walesby RK. The effect of leucocyte-depleting arterial line filters on cerebral microemboli and neuropsychological outcome following coronary artery bypass surgery. Eur J Cardio-Thorac Surg. Feb 2004;25(2):267-274.
Perthel M, Kseibi S, Bendisch A, Laas J. Use of a dynamic bubble trap in the arterial line reduces microbubbles during cardiopulmonary bypass and microembolic signals in the middle cerebral artery. Perfusion. May 2005;20(3):151-156.
Mitchell SJ, Willcox T, Gorman DF. Bubble generation and venous air filtration by hard-shell venous reservoirs: a comparative study. Perfusion. 1997;12(5):325-333.
Jones TJ, Deal DD, Vernon JC, Blackburn N, Stump DA. How effective are cardiopulmonary bypass circuits at removing gaseous microemboli?[see comment]. J Extra-Corporeal Technol. 2002;34(1):34-39.
Rodriguez RA, Williams KA, Babaev A, Rubens F, Nathan HJ. Effect of perfusionist technique on cerebral embolization during cardiopulmonary bypass. Perfusion. Jan 2005; 20(1):3-10.
Borger MA, Peniston CM, Weisel RD, Vasiliou M, Green RE, Feindel CM. Neuropsychologic impairment after coronary bypass surgery: effect of gaseous microemboli during perfusionist interventions. J Thorac Cardiovasc Surg. Apr 2001;121(4):743-749.
Willcox TW, Mitchell SJ, Gorman DF. Venous air in the bypass circuit: a source of arterial line emboli exacerbated by vacuum-assisted drainage. Ann Thorac Surg. 1999; 68(4):1285-1289.
Jones TJ, Deal DD, Vernon JC, Blackburn N, Stump DA. Does vacuum-assisted venous drainage increase gaseous microemboli during cardiopulmonary bypass? Ann Thorac Surg. 2002;74(6):2132-2137.
Norman MJ, Sistino JJ, Acsell JR. The effectiveness of low-prime cardiopulmonary bypass circuits at removing gaseous emboli. J Extra-Corp Technol. Dec 2004;36(4):336-342.
Young JA, Kisker CT, Doty DB. Adequate anticoagulation during cardiopulmonary bypass determined by activated clotting time and the appearance of fibrin monomer. Ann Thorac Surg. 1978;26(3):231-240.
Esposito RA, Culliford AT, Colvin SB, Thomas SJ, Lackner H, Spencer FC. The role of the activated clotting time in heparin administration and neutralization for cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1983;85(2):174-185.
Radegran K, Aren C, Teger-Nilsson A. Prostacyclin infusion during extracorporeal circulation for coronary bypass. J Thorac Cardiovasc Surg. 1982;83:205-211.
Longmore DB, Bennett G, Gueirrara D, et al. Prostacyclin: a solution to some problems of extracorporeal circulation. Lancet. 1979;1:1002-1005.
Slogoff S, Girgis KZ, Keats AS. Etiologic factors in neuropsychiatric complications associated with cardiopulmonary bypass. Anesth Analgesia. 1982;61:903-911.
Nussmeier NA, Arlund C, Slogoff S. Neuropsychiatric complications after cardiopulmonary bypass: cerebral protection by a barbiturate. Anesthesiology. 1986;64(2):165-170.
Newberg LA, Michenfelder JD. Cerebral protection by isoflurane during hypoxemia or ischemia. Anesthesiology. 1983;59:29-35.
Bashein G, Townes BD, Nessly ML, Bledsoe SW, Hornbein TF. Carbon dioxide management during hypothermic cardiopulmonary bypass. Anesthesiology. 1989;71(Suppl 3A):A35.
Patel RL, Turtle MR, Chambers DJ, James DN, Newman S, Venn GE. Alpha-stat acid-base regulation during cardiopulmonary bypass improves neuropsychologic outcome in patients undergoing coronary artery bypass grafting [see comments]. J Thorac Cardiovasc Surg. 1996;111(6):1267-1279.
Henriksen L, Hjelms E, Lindeburgh T. Brain hyperperfusion during cardiac operations. J Thorac Cardiovasc Surg. 1983;86:202-208.
Davila-Roman VG, Barzilai B, Wareing TH, Murphy SF, Schechtman KB, Kouchoukos NT. Atherosclerosis of the ascending aorta. Prevalence and role as an independent predictor of cerebrovascular events in cardiac patients. Stroke. 1994;25(10):2010-2016.
Wareing TH, Davila-Roman VG, Barzilai B, Murphy SF, Kouchoukos NT. Management of the severely atherosclerotic ascending aorta during cardiac operations. A strategy for detection and treatment. J Thorac Cardiovasc Surg. 1992;103(3):453-462.
Davila-Roman VG, Phillips KJ, Daily BB, Davila RM, Kouchoukos NT, Barzilai B. Intraoperative transesophageal echocardiography and epiaortic ultrasound for assessment of atherosclerosis of the thoracic aorta. J Am Coll Cardiol. 1996;28(4):942-947.
Culliford AT, Colvin SB, Rohrer K, Baumann FG, Spencer FC. The atherosclerotic ascending aorta and transverse arch: a new technique to prevent cerebral injury during bypass: experience with 13 patients. Ann Thorac Surg. 1986;41(1):27-35.
Borger MA, Taylor RL, Weisel RD, et al. Decreased cerebral emboli during distal aortic arch cannulation: a randomized clinical trial. J Thorac Cardiovasc Surg. 1999;118(4):740-745.
Hammon JW, Stump DA, Butterworth JF, et al. Coronary artery bypass grafting with single cross-clamp results in fewer persistent neuropsychological deficits than multiple clamp or off-pump coronary artery bypass grafting. Ann Thorac Surg. Oct 2007;84(4):1174-1178. discussion 1178-1179.
Brooker RF, Brown WR, Moody DM, et al. Cardiotomy suction: a major source of brain lipid emboli during cardiopulmonary bypass. Ann Thorac Surg. 1998;65(6):1651-1655.
Kincaid EH, Jones TJ, Stump DA, et al. Processing scavenged blood with a cell saver reduces cerebral lipid microembolization. Ann Thorac Surg. 2000;70(4):1296-1300.
Djaiani G, Fedorko L, Borger MA, et al. Continuous-flow cell saver reduces cognitive decline in elderly patients after coronary bypass surgery [see comment]. Circulation. Oct 23 2007;116(17):1888-1895.
Rubens FD, Boodhwani M, Mesana T, et al. The cardiotomy trial: a randomized, double-blind study to assess the effect of processing of shed blood during cardiopulmonary bypass on transfusion and neurocognitive function. Circulation. Sep 11 2007;116(11):I89-97.
Walpoth BH, Eggensperger N, Hauser SP, et al. Effects of unprocessed and processed cardiopulmonary bypass blood retransfused into patients after cardiac surgery. Int J Art Organs. 1999;22(4):210-216.
Boodhwani M, Nathan HJ, Mesana TG, Rubens FD, Cardiotomy I. Effects of shed mediastinal blood on cardiovascular and pulmonary function: a randomized, double-blind study. Ann Thorac Surg. October 1, 2008;86(4):1167-1173.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer London
About this chapter
Cite this chapter
Bhudia, S.K., Stump, D.A., Jones, T.J. (2011). Current Techniques of Emboli Detection and Their Utility in Brain Protection Studies. In: Bonser, R., Pagano, D., Haverich, A. (eds) Brain Protection in Cardiac Surgery. Springer, London. https://doi.org/10.1007/978-1-84996-293-3_9
Download citation
DOI: https://doi.org/10.1007/978-1-84996-293-3_9
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-84996-292-6
Online ISBN: 978-1-84996-293-3
eBook Packages: MedicineMedicine (R0)