Abstract
Abnormal protein folding and self-assembly causes over 30 cureless human diseases for which no disease-modifying therapies are available. The common side to all these diseases is formation of aberrant toxic protein oligomers and amyloid fibrils. Both types of assemblies are drug targets, yet each presents major challenges to drug design, discovery, and development. In this review, we focus on two small molecules that inhibit formation of toxic amyloid protein assemblies — the green-tea derivative (−)-epigallocatechin-3-gallate (EGCG), which was identified through a combination of epidemiologic data and a compound library screen, and the molecular tweezer CLR01, whose inhibitory activity was discovered in our group based on rational reasoning, and subsequently confirmed experimentally. Both compounds act in a manner that is not specific to one particular protein and thus are useful against a multitude of amyloidogenic proteins, yet they act via distinct putative mechanisms. CLR01 disrupts protein aggregation through specific binding to lysine residues, whereas the mechanisms underlying the activity of EGCG are only recently beginning to unveil. We discuss current in vitro and, where available, in vivo literature related to EGCG and CLR01’s effects on amyloid β-protein, α-synuclein, transthyretin, islet amyloid polypeptide, and calcitonin. We also describe the toxicity, pharmacokinetics, and mechanism of action of each compound.
Similar content being viewed by others
Abbreviations
- ADAD:
-
Alzheimer’s disease
- AFM:
-
Atomic force microscopy
- Aβ:
-
Amyloid beta
- APP:
-
Amyloid β-protein precursor
- COMT:
-
Catechol-O-methyltransferase
- CYP 450:
-
Cytochrome P450
- EC:
-
Epicatechin
- ECG:
-
Epicatechin-3-gallate
- EGC:
-
Epigallocatechin
- EGCG:
-
Epigallocatechin-3-gallate
- EM:
-
Electron microscopy
- FAP:
-
Familial amyloidotic polyneuropathy
- IAPP:
-
Islet amyloid polypeptide
- IC50:
-
Half maximal inhibitory concentration
- IP:
-
Intraperitoneal
- MPTP:
-
1 - Methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine
- MT:
-
Molecular tweezer
- MTT:
-
3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide
- NBT:
-
Nitroblue-tetrazolium
- NMR:
-
Nuclear magnetic resonance
- PD:
-
Parkinson’s disease
- SDS-PAGE:
-
Sodium dodecyl sulfate polyacrylamide gel electrophoresis
- SPRi:
-
Surface plasmon resonance imaging
- ThT:
-
Thioflavin T
- TTR:
-
Transthyretin
- UPS:
-
Ubiquitin-proteasome system
References
Rahimi F., Shanmugam A., Bitan G., Structure-function relationships of pre-fibrillar protein assemblies in Alzheimer’s disease and related disorders, Curr. Alzheimer Res., 2008, 5, 319–341
Fändrich M., Oligomeric intermediates in amyloid formation: structure determination and mechanisms of toxicity, J. Mol. Biol., 2012, 421, 427–440
Serpell L.C., Alzheimer’s amyloid fibrils: structure and assembly, Biochim. Biophys. Acta, 2000, 1502, 16–30
Vinters H.V., Tung S., Solis O.E., Pathologic Lesions in Alzheimer disease and Other Neurodegenerative Diseases—Cellular and Molecular Components, In: Rahimi F., Bitan G. (Eds.), Non-fibrillar Amyloidogenic Protein Assemblies—Common Cytotoxins Underlying Degenerative Diseases, Springer, 2012
Hardy J.A., Higgins G.A., Alzheimer’s disease: the amyloid cascade hypothesis, Science, 1992, 256, 184–185
Soto C., Estrada L., Amyloid inhibitors and β-sheet breakers, Subcell. Biochem., 2005, 38, 351–364
Necula M., Kayed R., Milton S., Glabe C.G., Small molecule inhibitors of aggregation indicate that amyloid β oligomerization and fibrillization pathways are independent and distinct, J. Biol. Chem., 2007, 282, 10311–10324
Ladiwala A.R., Dordick J.S., Tessier P.M., Aromatic small molecules remodel toxic soluble oligomers of amyloid β through three independent pathways, J. Biol. Chem., 2011, 286, 3209–3218
Liu T., Bitan G., Modulating self-assembly of amyloidogenic proteins as a therapeutic approach for neurodegenerative diseases: strategies and mechanisms, ChemMedChem, 2012, 7, 359–374
Jan A., Adolfsson O., Allaman I., Buccarello A.L., Magistretti P.J., Pfeifer A., et al., Aβ42 neurotoxicity is mediated by ongoing nucleated polymerization process rather than by discrete Aβ42 species, J. Biol. Chem., 2011, 286, 8585–8596
Eikelenboom P., Veerhuis R., Familian A., Hoozemans J.J., van Gool W.A., Rozemuller A.J., Neuroinflammation in plaque and vascular β-amyloid disorders: clinical and therapeutic implications, Neurodegener. Dis., 2008, 5, 190–193
Esteras-Chopo A., Pastor M.T., Serrano L., Lopez de la Paz M., New strategy for the generation of specific D-peptide amyloid inhibitors, J. Mol. Biol., 2008, 377, 1372–1381
Fradinger E.A., Monien B.H., Urbanc B., Lomakin A., Tan M., Li H., et al., C-terminal peptides coassemble into Aβ42 oligomers and protect neurons against Aβ42-induced neurotoxicity, Proc. Natl. Acad. Sci. USA, 2008, 105, 14175–14180
Doig A.J., Peptide inhibitors of β-amyloid aggregation, Curr. Opin. Drug Discov. Devel., 2007, 10, 533–539
Cheng P.N., Liu C., Zhao M., Eisenberg D., Nowick J.S., Amyloid β-sheet mimics that antagonize protein aggregation and reduce amyloid toxicity, Nat. Chem., 2012, 4, 927–933
van Groen T., Wiesehan K., Funke S.A., Kadish I., Nagel-Steger L., Willbold D., Reduction of Alzheimer’s disease amyloid plaque load in transgenic mice by D3, A D-enantiomeric peptide identified by mirror image phage display, ChemMedChem, 2008, 3, 1848–1852
Belluti F., Rampa A., Gobbi S., Bisi A., Small-molecule inhibitors/modulators of amyloid-β peptide aggregation and toxicity for the treatment of Alzheimer’s disease—A patent review (2010–2012), Expert Opin. Ther. Pat., 2013
Re F., Airoldi C., Zona C., Masserini M., La Ferla B., Quattrocchi N., et al., β amyloid aggregation inhibitors: small molecules as candidate drugs for therapy of Alzheimer’s disease, Curr. Med. Chem., 2010, 17, 2990–3006
Roberts B.E., Shorter J., Escaping amyloid fate, Nat. Struct. Mol. Biol., 2008, 15, 544–546
Wang W., Protein aggregation and its inhibition in biopharmaceutics, Int. J. Pharm., 2005, 289, 1–30
Bartolini M., Andrisano V., Strategies for the inhibition of protein aggregation in human diseases, ChemBioChem., 2010, 11, 1018–1035
Bose M., Gestwicki J.E., Devasthali V., Crabtree G.R., Graef I.A., ‘Natureinspired’ drug-protein complexes as inhibitors of Aβ aggregation, Biochem. Soc. Trans., 2005, 33, 543–547
Cole G.M., Teter B., Frautschy S.A., Neuroprotective effects of curcumin, Adv. Exp. Med. Biol., 2007, 595, 197–212
Bastianetto S., Krantic S., Quirion R., Polyphenols as potential inhibitors of amyloid aggregation and toxicity: possible significance to Alzheimer’s disease, Mini Rev. Med. Chem., 2008, 8, 429–435
Porat Y., Abramowitz A., Gazit E., Inhibition of amyloid fibril formation by polyphenols: structural similarity and aromatic interactions as a common inhibition mechanism, Chem. Biol. Drug Des., 2006, 67, 27–37
Mandel S.A., Amit T., Weinreb O., Reznichenko L., Youdim M.B., Simultaneous manipulation of multiple brain targets by green tea catechins: a potential neuroprotective strategy for Alzheimer and Parkinson diseases, CNS Neurosci. Ther., 2008, 14, 352–365
Albani D., Polito L., Signorini A., Forloni G., Neuroprotective properties of resveratrol in different neurodegenerative disorders, BioFactors, 2010, 36, 370–376
Cheng B., Liu X., Gong H., Huang L., Chen H., Zhang X., et al., Coffee components inhibit amyloid formation of human islet amyloid polypeptide in vitro: possible link between coffee consumption and diabetes mellitus, J. Agric. Food Chem., 2011, 59, 13147–13155
Huang Y., Jin M., Pi R., Zhang J., Chen M., Ouyang Y., et al., Protective effects of caffeic acid and caffeic acid phenethyl ester against acrolein-induced neurotoxicity in HT22 mouse hippocampal cells, Neurosci. Lett., 2013, 535, 146–151
Mohamed T., Yeung J.C., Vasefi M.S., Beazely M.A., Rao P.P., Development and evaluation of multifunctional agents for potential treatment of Alzheimer’s disease: application to a pyrimidine-2,4-diamine template, Bioorg. Med. Chem. Lett., 2012, 22, 4707–4712
Mao F., Huang L., Luo Z., Liu A., Lu C., Xie Z., et al., O-Hydroxyl-or o-amino benzylamine-tacrine hybrids: multifunctional biometals chelators, antioxidants, and inhibitors of cholinesterase activity and amyloid-β aggregation, Bioorg. Med. Chem., 2012, 20, 5884–5892
Pi R., Mao X., Chao X., Cheng Z., Liu M., Duan X., et al., Tacrine-6-ferulic acid, a novel multifunctional dimer, inhibits amyloid-β-mediated Alzheimer’s disease-associated pathogenesis in vitro and in vivo, PLoS One, 2012, 7, e31921
Bag S., Ghosh S., Tulsan R., Sood A., Zhou W., Schifone C., et al., Design, synthesis and biological activity of multifunctional α,β-unsaturated carbonyl scaffolds for Alzheimer’s disease, Bioorg. Med. Chem. Lett., 2013
Nunes A., Marques S.M., Quintanova C., Silva D.F., Cardoso S.M., Chaves S., et al., Multifunctional iron-chelators with protective roles against neurodegenerative diseases, Dalton Trans., 2013
Telpoukhovskaia M.A., Patrick B.O., Rodriguez-Rodriguez C., Orvig C., Exploring the multifunctionality of thioflavin- and deferiprone-based molecules as acetylcholinesterase inhibitors for potential application in Alzheimer’s disease, Mol. Biosyst., 2013, 9, 792–805
Török B., Sood A., Bag S., Tulsan R., Ghosh S., Borkin D., et al., Diaryl hydrazones as multifunctional inhibitors of amyloid self-assembly, Biochemistry, 2013, 52, 1137–1148
Granzotto A., Zatta P., Resveratrol acts not through anti-aggregative pathways but mainly via its scavenging properties against Aβ and Aβ-metal complexes toxicity, PLoS One, 2011, 6, e21565
Stratton S.P., Bangert J.L., Alberts D.S., Dorr R.T., Dermal toxicity of topical (−)epigallocatechin-3-gallate in BALB/c and SKH1 mice, Cancer Lett., 2000, 158, 47–52
Miyamoto Y., Haylor J.L., El Nahas A.M., Cellular toxicity of catechin analogues containing gallate in opossum kidney proximal tubular (OK) cells, J. Toxicol. Sci., 2004, 29, 47–52
Mak J.C., Potential role of green tea catechins in various disease therapies: progress and promise, Clin. Exp. Pharmacol. Physiol., 2012, 39, 265–273
Balentine D.A., Wiseman S.A., Bouwens L.C., The chemistry of tea flavonoids, Crit. Rev. Food Sci. Nutr., 1997, 37, 693–704
Khan N., Afaq F., Saleem M., Ahmad N., Mukhtar H., Targeting multiple signaling pathways by green tea polyphenol (−)-epigallocatechin-3-gallate, Cancer Res., 2006, 66, 2500–2505
Ehrnhoefer D.E., Duennwald M., Markovic P., Wacker J.L., Engemann S., Roark M., et al., Green tea (−)-epigallocatechin-gallate modulates early events in huntingtin misfolding and reduces toxicity in Huntington’s disease models, Hum. Mol. Genet., 2006, 15, 2743–2751
Barranco Quintana J.L., Allam M.F., Del Castillo A.S., Navajas R.F., Parkinson’s disease and tea: a quantitative review, J. Am. Coll. Nutr., 2009, 28, 1–6
Hellenbrand W., Seidler A., Boeing H., Robra B.P., Vieregge P., Nischan P., et al., Diet and Parkinson’s disease. I: A possible role for the past intake of specific foods and food groups. Results from a selfadministered food-frequency questionnaire in a case-control study, Neurology, 1996, 47, 636–643
Ng T.P., Feng L., Niti M., Kua E.H., Yap K.B., Tea consumption and cognitive impairment and decline in older Chinese adults, Am. J. Clin. Nutr., 2008, 88, 224–231
Dragicevic N., Smith A., Lin X., Yuan F., Copes N., Delic V., et al., Green tea epigallocatechin-3-gallate (EGCG) and other flavonoids reduce Alzheimer’s amyloid-induced mitochondrial dysfunction, J. Alzheimers Dis., 2011, 26, 507–521
Fernandez J.W., Rezai-Zadeh K., Obregon D., Tan J., EGCG functions through estrogen receptor-mediated activation of ADAM10 in the promotion of non-amyloidogenic processing of APP, FEBS Lett., 2010, 584, 4259–4267
Lin C.L., Chen T.F., Chiu M.J., Way T.D., Lin J.K., Epigallocatechin gallate (EGCG) suppresses β-amyloid-induced neurotoxicity through inhibiting c-Abl/FE65 nuclear translocation and GSK3 β activation, Neurobiol. Aging, 2009, 30, 81–92
Mandel S.A., Amit T., Kalfon L., Reznichenko L., Weinreb O., Youdim M.B., Cell signaling pathways and iron chelation in the neurorestorative activity of green tea polyphenols: special reference to epigallocatechin gallate (EGCG), J. Alzheimers Dis., 2008, 15, 211–222
Singh B.N., Shankar S., Srivastava R.K., Green tea catechin, epigallocatechin-3-gallate (EGCG): mechanisms, perspectives and clinical applications, Biochem. Pharmacol., 2011, 82, 1807–1821
Smith A., Giunta B., Bickford P.C., Fountain M., Tan J., Shytle R.D., Nanolipidic particles improve the bioavailability and α-secretase inducing ability of epigallocatechin-3-gallate (EGCG) for the treatment of Alzheimer’s disease, Int. J. Pharm., 2010, 389, 207–212
Ruidavets J., Teissedre P., Ferrieres J., Carando S., Bougard G., Cabanis J., Catechin in the Mediterranean diet: vegetable, fruit or wine?, Atherosclerosis, 2000, 153, 107–117
Chyu K.Y., Babbidge S.M., Zhao X., Dandillaya R., Rietveld A.G., Yano J., et al., Differential effects of green tea-derived catechin on developing versus established atherosclerosis in apolipoprotein E-null mice, Circulation, 2004, 109, 2448–2453
Katiyar S., Elmets C.A., Katiyar S.K., Green tea and skin cancer: photoimmunology, angiogenesis and DNA repair, J. Nutr. Biochem., 2007, 18, 287–296
Meng F., Abedini A., Plesner A., Verchere C.B., Raleigh D.P., The flavanol (−)-epigallocatechin 3-gallate inhibits amyloid formation by islet amyloid polypeptide, disaggregates amyloid fibrils, and protects cultured cells against IAPP-induced toxicity, Biochemistry, 2010, 49, 8127–8133
Ehrnhoefer D.E., Bieschke J., Boeddrich A., Herbst M., Masino L., Lurz R., et al., EGCG redirects amyloidogenic polypeptides into unstructured, off-pathway oligomers, Nat. Struct. Mol. Biol., 2008, 15, 558–566
Bieschke J., Russ J., Friedrich R.P., Ehrnhoefer D.E., Wobst H., Neugebauer K., et al., EGCG remodels mature α-synuclein and amyloid-β fibrils and reduces cellular toxicity, Proc. Natl. Acad. Sci. USA, 2010, 107, 7710–7715
Masuda M., Suzuki N., Taniguchi S., Oikawa T., Nonaka T., Iwatsubo T., et al., Small molecule inhibitors of α-synuclein filament assembly, Biochemistry, 2006, 45, 6085–6094
Hauber I., Hohenberg H., Holstermann B., Hunstein W., Hauber J., The main green tea polyphenol epigallocatechin-3-gallate counteracts semen-mediated enhancement of HIV infection, Proc. Natl. Acad. Sci. USA, 2009, 106, 9033–9038
Popovych N., Brender J.R., Soong R., Vivekanandan S., Hartman K., Basrur V., et al., Site specific interaction of the polyphenol EGCG with the SEVI amyloid precursor peptide PAP(248–286), J. Phys. Chem. B, 2012, 116, 3650–3658
Chandrashekaran I.R., Adda C.G., MacRaild C.A., Anders R.F., Norton R.S., Inhibition by flavonoids of amyloid-like fibril formation by Plasmodium falciparum merozoite surface protein 2, Biochemistry, 2010, 49, 5899–5908
Chandrashekaran I.R., Adda C.G., Macraild C.A., Anders R.F., Norton R.S., EGCG disaggregates amyloid-like fibrils formed by Plasmodium falciparum merozoite surface protein 2, Arch. Biochem. Biophys., 2011, 513, 153–157
Rambold A.S., Miesbauer M., Olschewski D., Seidel R., Riemer C., Smale L., et al., Green tea extracts interfere with the stress-protective activity of PrP and the formation of PrP, J. Neurochem., 2008, 107, 218–229
Attar A., Bitan G., Disrupting Self-Assembly and Toxicity of Amyloidogenic Protein Oligomers by “Molecular Tweezers”-from the Test Tube to Animal Models, Curr. Pharm. Des., 2013, In press
Klärner F.G., Schrader T., Aromatic interactions by molecular tweezers and clips in chemical and biological systems, Acc. Chem. Res., 2013, 46, 967–978
Fokkens M., Schrader T., Klärner F.G., A molecular tweezer for lysine and arginine, J. Am. Chem. Soc., 2005, 127, 14415–14421
Talbiersky P., Bastkowski F., Klärner F.G., Schrader T., Molecular clip and tweezer introduce new mechanisms of enzyme inhibition, J. Am. Chem. Soc., 2008, 130, 9824–9828
Sinha S., Lopes D.H., Du Z., Pang E.S., Shanmugam A., Lomakin A., et al., Lysine-specific molecular tweezers are broad-spectrum inhibitors of assembly and toxicity of amyloid proteins, J. Am. Chem. Soc., 2011, 133, 16958–16969
Bier D., Rose R., Bravo-Rodriguez K., Bartel M., Ramirez-Anguita J.M., Dutt S., et al., Molecular tweezers modulate 14-3-3 protein-protein interactions, Nat. Chem., 2013, 5, 234–239
Attar A., Ripoli C., Riccardi E., Maiti P., Li Puma D.D., Liu T., et al., Protection of primary neurons and mouse brain from Alzheimer’s pathology by molecular tweezers, Brain, 2012, 135, 3735–3748
Prabhudesai S., Sinha S., Attar A., Kotagiri A., Fitzmaurice A.G., Lakshmanan R., et al., A novel “molecular tweezer” inhibitor of α-synuclein neurotoxicity in vitro and in vivo, Neurotherapeutics, 2012, 9, 464–476
Glenner G.G., Wong C.W., Alzheimer’s disease: Initial report of the purification and characterization of a novel cerebrovascular amyloid protein, Biochem. Biophys. Res. Commun., 1984, 120, 885–890
Masters C.L., Simms G., Weinman N.A., Multhaup G., McDonald B.L., Beyreuther K., Amyloid plaque core protein in Alzheimer disease and Down syndrome, Proc. Natl. Acad. Sci. U.S.A., 1985, 82, 4245–4249
Hardy J., Selkoe D.J., The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics, Science, 2002, 297, 353–356.
Bastianetto S., Yao Z.X., Papadopoulos V., Quirion R., Neuroprotective effects of green and black teas and their catechin gallate esters against β-amyloid-induced toxicity, Eur. J. Neurosci., 2006, 23, 55–64
LeVine H., 3rd, Quantification of β-sheet amyloid fibril structures with thioflavin T., Methods Enzymol., 1999, 309, 274–284
Palhano F.L., Lee J., Grimster N.P., Kelly J.W., Toward the molecular mechanism(s) by which EGCG treatment remodels mature amyloid fibrils, J. Am. Chem. Soc., 2013, 135, 7503–7510
Walsh D.M., Klyubin I., Fadeeva J.V., Cullen W.K., Anwyl R., Wolfe M.S., et al., Naturally secreted oligomers of amyloid β protein potently inhibit hippocampal long-term potentiation in vivo, Nature, 2002, 416, 535–539
Reed M.N., Hofmeister J.J., Jungbauer L., Welzel A.T., Yu C., Sherman M.A., et al., Cognitive effects of cell-derived and synthetically derived Aβ oligomers, Neurobiol. Aging, 2011, 32, 1784–1794
O’Nuallain B., Freir D.B., Nicoll A.J., Risse E., Ferguson N., Herron C.E., et al., Amyloid β-protein dimers rapidly form stable synaptotoxic protofibrils, J. Neurosci., 2010, 30, 14411–14419
Kayed R., Head E., Thompson J.L., McIntire T.M., Milton S.C., Cotman C.W., et al., Common structure of soluble amyloid oligomers implies common mechanism of pathogenesis, Science, 2003, 300, 486–489
Paz M.A., Flückiger R., Boak A., Kagan H.M., Gallop P.M., Specific detection of quinoproteins by redox-cycling staining, J. Biol. Chem., 1991, 266, 689–692
Lopez del Amo J.M., Fink U., Dasari M., Grelle G., Wanker E.E., Bieschke J., et al., Structural properties of EGCG-induced, nontoxic Alzheimer’s disease Aβ oligomers, J. Mol. Biol., 2012, 421, 517–524
Bitan G., Kirkitadze M.D., Lomakin A., Vollers S.S., Benedek G.B., Teplow D.B., Amyloid β-protein (Aβ) assembly: Aβ40 and Aβ42 oligomerize through distinct pathways, Proc. Natl. Acad. Sci. USA, 2003, 100, 330–335
Hoshi M., Sato M., Matsumoto S., Noguchi A., Yasutake K., Yoshida N., et al., Spherical aggregates of β-amyloid (amylospheroid) show high neurotoxicity and activate tau protein kinase I/glycogen synthase kinase-3β, Proc. Natl. Acad. Sci. USA, 2003, 100, 6370–6375
Dahlgren K.N., Manelli A.M., Stine W.B., Jr., Baker L.K., Krafft G.A., LaDu M.J., Oligomeric and fibrillar species of amyloid-β peptides differentially affect neuronal viability, J. Biol. Chem., 2002, 277, 32046–32053
Harper J.D., Lansbury P.T., Jr., Models of amyloid seeding in Alzheimer’s disease and scrapie: mechanistic truths and physiological consequences of the time-dependent solubility of amyloid proteins, Annu. Rev. Biochem, 1997, 66, 385–407
Petkova A.T., Ishii Y., Balbach J.J., Antzutkin O.N., Leapman R.D., Delaglio F., et al., A structural model for Alzheimer’s β-amyloid fibrils based on experimental constraints from solid state NMR, Proc. Natl. Acad. Sci. USA, 2002, 99, 16742–16747
Petkova A.T., Yau W.M., Tycko R., Experimental constraints on quaternary structure in Alzheimer’s β-amyloid fibrils, Biochemistry, 2006, 45, 498–512
Lazo N.D., Grant M.A., Condron M.C., Rigby A.C., Teplow D.B., On the nucleation of amyloid β-protein monomer folding, Protein Sci., 2005, 14, 1581–1596
Yu L., Edalji R., Harlan J.E., Holzman T.F., Lopez A.P., Labkovsky B., et al., Structural characterization of a soluble amyloid β-peptide oligomer, Biochemistry, 2009, 48, 1870–1877
Wang S.H., Liu F.F., Dong X.Y., Sun Y., Thermodynamic analysis of the molecular interactions between amyloid β-peptide 42 and (−)-epigallocatechin-3-gallate, J. Phys. Chem. B, 2010, 114, 11576–11583
Wang S.H., Dong X.Y., Sun Y., Thermodynamic analysis of the molecular interactions between amyloid β-protein fragments and (−)-epigallocatechin-3-gallate, J. Phys. Chem. B, 2012, 116, 5803–5809
Hane F., Tran G., Attwood S.J., Leonenko Z., Cu2+ affects amyloid-β (1–42) aggregation by increasing peptide-peptide binding forces, PLoS One, 2013, 8, e59005
Solomonov I., Korkotian E., Born B., Feldman Y., Bitler A., Rahimi F., et al., Zn2+-Aβ40 complexes form metastable quasi-spherical oligomers that are cytotoxic to cultured hippocampal neurons, J. Biol. Chem., 2012, 287, 20555–20564
Mancino A.M., Hindo S.S., Kochi A., Lim M.H., Effects of clioquinol on metal-triggered amyloid-β aggregation revisited, Inorg. Chem., 2009, 48, 9596–9598
Bush A.I., Masters C.L., Tanzi R.E., Copper, β-amyloid, and Alzheimer’s disease: Tapping a sensitive connection, Proc. Natl. Acad. Sci. USA, 2003, 100, 11193–11194
Huang X., Moir R.D., Tanzi R.E., Bush A.I., Rogers J.T., Redox-active metals, oxidative stress, and Alzheimer’s disease pathology, Ann. N. Y. Acad. Sci., 2004, 1012, 153–163
Pirker K.F., Baratto M.C., Basosi R., Goodman B.A., Influence of pH on the speciation of copper(II) in reactions with the green tea polyphenols, epigallocatechin gallate and gallic acid, J. Inorg. Biochem., 2012, 112, 10–16
Sun S.L., He G.Q., Yu H.N., Yang J.G., Borthakur D., Zhang L.C., et al., Free Zn2+ enhances inhibitory effects of EGCG on the growth of PC-3 cells, Mol. Nutr. Food Res., 2008, 52, 465–471
Weinreb O., Amit T., Mandel S., Youdim M.B., Neuroprotective molecular mechanisms of (−)-epigallocatechin-3-gallate: a reflective outcome of its antioxidant, iron chelating and neuritogenic properties, Genes Nutr. 2009, 4, 283–296
Seeram N.P., Henning S.M., Niu Y., Lee R., Scheuller H.S., Heber D., Catechin and caffeine content of green tea dietary supplements and correlation with antioxidant capacity, J. Agric. Food Chem., 2006, 54, 1599–1603
Zhang Y., Jiang T., Zheng Y., Zhou P., Interference of EGCG on the Zn(II)-induced conformational transition of silk fibroin as a model protein related to neurodegenerative diseases, Soft Matter, 2012, 8, 5543–5549
Cheng X.R., Hau B.Y., Veloso A.J., Martic S., Kraatz H.B., Kerman K., Surface plasmon resonance imaging of amyloid-β aggregation kinetics in the presence of epigallocatechin gallate and metals, Anal. Chem., 2013, 85, 2049–2055
Hyung S.J., DeToma A.S., Brender J.R., Lee S., Vivekanandan S., Kochi A., et al., Insights into antiamyloidogenic properties of the green tea extract (−)-epigallocatechin-3-gallate toward metal-associated amyloid-β species, Proc. Natl. Acad. Sci. USA, 2013, 110, 3743–3748
Sinha S., Du Z., Maiti P., Klärner F.G., Schrader T., Wang C., et al., Comparison of three amyloid assembly inhibitors: the sugar scylloinositol, the polyphenol epigallocatechin gallate, and the molecular tweezer CLR01, ACS Chem. Neurosci., 2012, 3, 451–458
Miyai S., Yamaguchi A., Iwasaki T., Shamsa F., Ohtsuki K., Biochemical characterization of epigallocatechin-3-gallate as an effective stimulator for the phosphorylation of its binding proteins by glycogen synthase kinase-3β in vitro, Biol. Pharm. Bull., 2010, 33, 1932–1937
Takashima A., The Mechanism of tau aggregation and its relation to neuronal dysfunction, Alzheimer’s Association Interantional Conference on Alzheimer’s disease, 2010, S144, Abstract No. PL-104-103.
Frost B., Ollesch J., Wille H., Diamond M.I., Conformational diversity of wild-type Tau fibrils specified by templated conformation change, J. Biol. Chem., 2009, 284, 3546–3551
Hsiao K., Chapman P., Nilsen S., Eckman C., Harigaya Y., Younkin S., et al., Correlative memory deficits, Aβ elevation, and amyloid plaques in transgenic mice, Science, 1996, 274, 99–102
Rezai-Zadeh K., Shytle D., Sun N., Mori T., Hou H., Jeanniton D., et al., Green tea epigallocatechin-3-gallate (EGCG) modulates amyloid precursor protein cleavage and reduces cerebral amyloidosis in Alzheimer transgenic mice, J. Neurosci., 2005, 25, 8807–8814
Rezai-Zadeh K., Arendash G.W., Hou H., Fernandez F., Jensen M., Runfeldt M., et al., Green tea epigallocatechin-3-gallate (EGCG) reduces β-amyloid mediated cognitive impairment and modulates tau pathology in Alzheimer transgenic mice, Brain Res., 2008, 1214, 177–187
Hwang D.Y., Chae K.R., Kang T.S., Hwang J.H., Lim C.H., Kang H.K., et al., Alterations in behavior, amyloid β-42, caspase-3, and Cox-2 in mutant PS2 transgenic mouse model of Alzheimer’s disease, FASEB J., 2002, 16, 805–813
Lee J.W., Lee Y.K., Ban J.O., Ha T.Y., Yun Y.P., Han S.B., et al., Green tea (−)-epigallocatechin-3-gallate inhibits β-amyloid-induced cognitive dysfunction through modification of secretase activity via inhibition of ERK and NF-κB pathways in mice, J. Nutr., 2009, 139, 1987–1993
Lee S.Y., Lee J.W., Lee H., Yoo H.S., Yun Y.P., Oh K.W., et al., Inhibitory effect of green tea extract on β-amyloid-induced PC12 cell death by inhibition of the activation of NF-κB and ERK/p38 MAP kinase pathway through antioxidant mechanisms, Brain Res. Mol. Brain Res., 2005, 140, 45–54
Rasoolijazi H., Joghataie M.T., Roghani M., Nobakht M., The beneficial effect of (−)-epigallocatechin-3-gallate in an experimental model of Alzheimer’s disease in rat: a behavioral analysis, Iran Biomed. J., 2007, 11, 237–243
Lee Y.K., Yuk D.Y., Lee J.W., Lee S.Y., Ha T.Y., Oh K.W., et al., (−)-Epigallocatechin-3-gallate prevents lipopolysaccharide-induced elevation of β-amyloid generation and memory deficiency, Brain Res., 2009, 1250, 164–174
Lee Y.J., Choi D.Y., Yun Y.P., Han S.B., Oh K.W., Hong J.T., Epigallocatechin-3-gallate prevents systemic inflammationinduced memory deficiency and amyloidogenesis via its antineuroinflammatory properties, J. Nutr. Biochem., 2013, 24, 298–310
Miklossy J., Kis A., Radenovic A., Miller L., Forro L., Martins R., et al., β-amyloid deposition and Alzheimer’s type changes induced by Borrelia spirochetes, Neurobiol. Aging, 2006, 27, 228–236
Link C.D., Expression of human β-amyloid peptide in transgenic Caenorhabditis elegans, Proc. Natl. Acad. Sci. USA, 1995, 92, 9368–9372
Abbas S., Wink M., Epigallocatechin gallate inhibits β amyloid oligomerization in Caenorhabditis elegans and affects the daf-2/ insulin-like signaling pathway, Phytomedicine, 2010, 17, 902–909
Bitan G., Fradinger E.A., Spring S.M., Teplow D.B., Neurotoxic protein oligomers—what you see is not always what you get, Amyloid, 2005, 12, 88–95
Hepler R.W., Grimm K.M., Nahas D.D., Breese R., Dodson E.C., Acton P., et al., Solution state characterization of amyloid β-derived diffusible ligands, Biochemistry, 2006, 45, 15157–15167
Khan J.M., Qadeer A., Chaturvedi S.K., Ahmad E., Rehman S.A., Gourinath S., et al., SDS can be utilized as an amyloid inducer: a case study on diverse proteins, PLoS One, 2012, 7, e29694
Watt A.D., Perez K.A., Rembach A., Sherrat N.A., Hung L.W., Johanssen T., et al., Oligomers, fact or artefact? SDS-PAGE induces dimerization of β-amyloid in human brain samples, Acta Neuropathol. (Berl). 2013
Jankowsky J.L., Fadale D.J., Anderson J., Xu G.M., Gonzales V., Jenkins N.A., et al., Mutant presenilins specifically elevate the levels of the 42 residue β-amyloid peptide in vivo: evidence for augmentation of a 42-specific γ secretase, Hum. Mol. Genet., 2004, 13, 159–170
Oddo S., Caccamo A., Shepherd J.D., Murphy M.P., Golde T.E., Kayed R., et al., Triple-transgenic model of Alzheimer’s disease with plaques and tangles: intracellular Aβ and synaptic dysfunction, Neuron, 2003, 39, 409–421
George J.M., Jin H., Woods W.S., Clayton D.F., Characterization of a novel protein regulated during the critical period for song learning in the zebra finch, Neuron, 1995, 15, 361–372
Maroteaux L., Scheller R.H., The rat brain synucleins; family of proteins transiently associated with neuronal membrane, Brain Res. Mol. Brain Res., 1991, 11, 335–343
Maroteaux L., Campanelli J.T., Scheller R.H., Synuclein: a neuronspecific protein localized to the nucleus and presynaptic nerve terminal, J. Neurosci., 1988, 8, 2804–2815
Bendor J.T., Logan T.P., Edwards R.H., The function of α-synuclein, Neuron, 2013, 79, 1044–1066
El-Agnaf O.M.A., Jakes R., Curran M.D., Middleton D., Ingenito R., Bianchi E., et al., Aggregates from mutant and wild-type α-synuclein proteins and NAC peptide induce apoptotic cell death in human neuroblastoma cells by formation of β-sheet and amyloid-like filaments, FEBS Lett., 1998, 440, 71–75
Acharya S., Safaie B., Wongkongkathep P., Ivanova M.I., Attar A., Klärner F.-G., et al., Molecular basis for preventing α-synuclein aggregation by a molecular tweezer, 2013, Submitted for publication
Ng C.H., Mok S.Z., Koh C., Ouyang X., Fivaz M.L., Tan E.K., et al., Parkin protects against LRRK2 G2019S mutant-induced dopaminergic neurodegeneration in Drosophila, J. Neurosci., 2009, 29, 11257–11262
Wang C., Lu R., Ouyang X., Ho M.W., Chia W., Yu F., et al., Drosophila overexpressing parkin R275W mutant exhibits dopaminergic neuron degeneration and mitochondrial abnormalities, J. Neurosci., 2007, 27, 8563–8570
Ng C.H., Guan M.S., Koh C., Ouyang X., Yu F., Tan E.K., et al., AMP kinase activation mitigates dopaminergic dysfunction and mitochondrial abnormalities in Drosophila models of Parkinson’s disease, J. Neurosci., 2012, 32, 14311–14317
Bonilla-Ramirez L., Jimenez-Del-Rio M., Velez-Pardo C., Low doses of paraquat and polyphenols prolong life span and locomotor activity in knock-down parkin Drosophila melanogaster exposed to oxidative stress stimuli: implication in autosomal recessive juvenile Parkinsonism, Gene, 2013, 512, 355–363
Choi J.Y., Park C.S., Kim D.J., Cho M.H., Jin B.K., Pie J.E., et al., Prevention of nitric oxide-mediated 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridineinduced Parkinson’s disease in mice by tea phenolic epigallocatechin 3-gallate, Neurotoxicology, 2002, 23, 367–374
Kim J.S., Kim J.M., O J.J., Jeon B.S., Inhibition of inducible nitric oxide synthase expression and cell death by (−)-epigallocatechin-3-gallate, a green tea catechin, in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine mouse model of Parkinson’s disease, J. Clin. Neurosci., 2010, 17, 1165–1168
Reznichenko L., Kalfon L., Amit T., Youdim M.B., Mandel S.A., Low dosage of rasagiline and epigallocatechin gallate synergistically restored the nigrostriatal axis in MPTP-induced parkinsonism, Neurodegener. Dis., 2010, 7, 219–231
Youdim M.B., Grunblatt E., Levites Y., Maor G., Mandel S., Early and late molecular events in neurodegeneration and neuroprotection in Parkinson’s disease MPTP model as assessed by cDNA microarray; the role of iron, Neurotox. Res., 2002, 4, 679–689
Leaver K.R., Allbutt H.N., Creber N.J., Kassiou M., Henderson J.M., Oral pre-treatment with epigallocatechin gallate in 6-OHDA lesioned rats produces subtle symptomatic relief but not neuroprotection, Brain Res. Bull., 2009, 80, 397–402
Kang K.S., Wen Y., Yamabe N., Fukui M., Bishop S.C., Zhu B.T., Dual beneficial effects of (−)-epigallocatechin-3-gallate on levodopa methylation and hippocampal neurodegeneration: in vitro and in vivo studies, PLoS One, 2010, 5, e11951
Emmanouilidou E., Stefanis L., Vekrellis K., Cell-produced α-synuclein oligomers are targeted to, and impair, the 26S proteasome, Neurobiol. Aging, 2010, 31, 953–968
Zhang N.Y., Tang Z., Liu C.W., α-Synuclein protofibrils inhibit 26 S proteasome-mediated protein degradation: understanding the cytotoxicity of protein protofibrils in neurodegenerative disease pathogenesis, J. Biol. Chem., 2008, 283, 20288–20298
Lulla A., Barnhill L., Stahl M., Fitzmaurice A.G., Li S., Bronstein J.M., Neurotoxicity of the dithiocarbamate fungicide ziram is dependent on synuclein in zebrafish: Implications for Parkinson’s disease, Society of Toxicology Annual Meeting, 2013, Abstract #1407.
Wang X.F., Li S., Chou A.P., Bronstein J.M., Inhibitory effects of pesticides on proteasome activity: implication in Parkinson’s disease, Neurobiol. Dis., 2006, 23, 198–205
Zhou Y., Shie F.S., Piccardo P., Montine T.J., Zhang J., Proteasomal inhibition induced by manganese ethylene-bis-dithiocarbamate: relevance to Parkinson’s disease, Neuroscience, 2004, 128, 281–291
Chou A.P., Maidment N., Klintenberg R., Casida J.E., Li S., Fitzmaurice A.G., et al., Ziram causes dopaminergic cell damage by inhibiting E1 ligase of the proteasome, J. Biol. Chem., 2008, 283, 34696–34703
Wang A., Costello S., Cockburn M., Zhang X., Bronstein J., Ritz B., Parkinson’s disease risk from ambient exposure to pesticides, Eur. J. Epidemiol., 2011, 26, 547–555
Rinetti G.V., Schweizer F.E., Ubiquitination acutely regulates presynaptic neurotransmitter release in mammalian neurons, J. Neurosci., 2010, 30, 3157–3166
Saraiva M., Cardoso I., Transthyretin Aggregation and Toxicity, In: Rahimi F., Bitan G. (Eds.), Non-fibrillar Amyloidogenic Protein Assemblies—Common Cytotoxins Underlying Degenerative Diseases, Springer Netherlands, 2012
Westermark P., Senile systemic amyloidosis — An overview, Amyloid, 2001, 8, 121
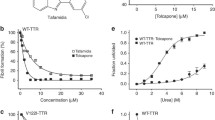
Ferreira N., Cardoso I., Domingues M.R., Vitorino R., Bastos M., Bai G., et al., Binding of epigallocatechin-3-gallate to transthyretin modulates its amyloidogenicity, FEBS Lett., 2009, 583, 3569–3576
Miyata M., Sato T., Kugimiya M., Sho M., Nakamura T., Ikemizu S., et al., The crystal structure of the green tea polyphenol (−)-epigallocatechin gallate-transthyretin complex reveals a novel binding site distinct from the thyroxine binding site, Biochemistry, 2010, 49, 6104–6114
Kristen A.V., Lehrke S., Buss S., Mereles D., Steen H., Ehlermann P., et al., Green tea halts progression of cardiac transthyretin amyloidosis: an observational report, Clin. Res. Cardiol., 2012, 101, 805–813
Kristen A.V., Perz J.B., Schonland S.O., Hegenbart U., Schnabel P.A., Kristen J.H., et al., Non-invasive predictors of survival in cardiac amyloidosis, Eur. J. Heart Fail., 2007, 9, 617–624
Mörner S., Hellman U., Suhr O.B., Kazzam E., Waldenstrom A., Amyloid heart disease mimicking hypertrophic cardiomyopathy, J. Intern. Med., 2005, 258, 225–230
Ferreira N., Saraiva M.J., Almeida M.R., Epigallocatechin-3-gallate as a potential therapeutic drug for TTR-related amyloidosis: “in vivo” evidence from FAP mice models, PLoS One, 2012, 7, e29933
Santos S.D., Fernandes R., Saraiva M.J., The heat shock response modulates transthyretin deposition in the peripheral and autonomic nervous systems, Neurobiol. Aging, 2010, 31, 280–289
Ferreira N., Pereira-Henriques A., Attar A., Klärner F.-G., Schrader T., Bitan G., et al., Molecular Tweezers Targeting Transthyretin Amyloidosis, 2013, Submitted for publication
Westermark P., Wernstedt C., Wilander E., Hayden D.W., O’Brien T.D., Johnson K.H., Amyloid fibrils in human insulinoma and islets of Langerhans of the diabetic cat are derived from a neuropeptide-like protein also present in normal islet cells, Proc. Natl. Acad. Sci. USA, 1987, 84, 3881–3885
Cooper G.J., Willis A.C., Clark A., Turner R.C., Sim R.B., Reid K.B., Purification and characterization of a peptide from amyloid-rich pancreases of type 2 diabetic patients, Proc. Natl. Acad. Sci. USA, 1987, 84, 8628–8632
Kahn S.E., Andrikopoulos S., Verchere C.B., Islet amyloid: a longrecognized but underappreciated pathological feature of type 2 diabetes, Diabetes, 1999, 48, 241–253
Clark A., Cooper G.J., Lewis C.E., Morris J.F., Willis A.C., Reid K.B., et al., Islet amyloid formed from diabetes-associated peptide may be pathogenic in type-2 diabetes, Lancet, 1987, 2, 231–234
Hull R.L., Westermark G.T., Westermark P., Kahn S.E., Islet amyloid: a critical entity in the pathogenesis of type 2 diabetes, J. Clin. Endocrinol. Metab., 2004, 89, 3629–3643
Lorenzo A., Razzaboni B., Weir G.C., Yankner B.A., Pancreatic islet cell toxicity of amylin associated with type-2 diabetes mellitus, Nature, 1994, 368, 756–760
Clark A., Wells C.A., Buley I.D., Cruickshank J.K., Vanhegan R.I., Matthews D.R., et al., Islet amyloid, increased a-cells, reduced b-cells and exocrine fibrosis: quantitative changes in the pancreas in type 2 diabetes, Diabetes Res., 1988, 9, 151–159
Butler A.E., Janson J., Bonner-Weir S., Ritzel R., Rizza R.A., Butler P.C., β-Cell deficit and increased β-cell apoptosis in humans with type 2 diabetes, Diabetes, 2003, 52, 102–110
Bahramikia S., Yazdanparast R., Inhibition of human islet amyloid polypeptide or amylin aggregation by two manganese-salen derivatives, Eur. J. Pharmacol., 2013, 707, 17–25
Cheng B., Gong H., Li X., Sun Y., Chen H., Zhang X., et al., Salvianolic acid B inhibits the amyloid formation of human islet amyloid polypeptideand protects pancreatic β-cells against cytotoxicity, Proteins, 2013, 81, 613–621
Cheng B., Gong H., Li X., Sun Y., Zhang X., Chen H., et al., Silibinin inhibits the toxic aggregation of human islet amyloid polypeptide, Biochem. Biophys. Res. Commun., 2012, 419, 495–499
Hagihara M., Takei A., Ishii T., Hayashi F., Kubota K., Wakamatsu K., et al., Inhibitory effects of choline-O-sulfate on amyloid formation of human islet amyloid polypeptide, FEBS open bio, 2012, 2, 20–25
Seeliger J., Winter R., Islet amyloid polypeptide: Aggregation and fibrillogenesis in vitro and its inhibition, Subcell. Biochem., 2012, 65, 185–209
Engel M.F., vandenAkker C.C., Schleeger M., Velikov K.P., Koenderink G.H., Bonn M., The polyphenol EGCG inhibits amyloid formation less efficiently at phospholipid interfaces than in bulk solution, J. Am. Chem. Soc., 2012, 134, 14781–14788
Fu L., Ma G., Yan E.C., In situ misfolding of human islet amyloid polypeptide at interfaces probed by vibrational sum frequency generation, J. Am. Chem. Soc., 2010, 132, 5405–5412
Fu L., Liu J., Yan E.C., Chiral sum frequency generation spectroscopy for characterizing protein secondary structures at interfaces, J. Am. Chem. Soc., 2011, 133, 8094–8097
Suzuki Y., Brender J.R., Hartman K., Ramamoorthy A., Marsh E.N., Alternative pathways of human islet amyloid polypeptide aggregation distinguished by 19F nuclear magnetic resonancedetected kinetics of monomer consumption, Biochemistry, 2012, 51, 8154–8162
Lopes D.H.J., Attar A., Du Z., McDaniel K., Dutt S., Bravo-Rodriguez K., et al., The molecular tweezer CLR01 inhibits islet amyloid polypeptide assembly and toxicity via an unexpected mechanism, 2013, Submitted for publication
Sexton P.M., Findlay D.M., Martin T.J., Calcitonin, Curr. Med. Chem., 1999, 6, 1067–1093
Copp D.H., Calcitonin: discovery, development, and clinical application, Clin. Invest. Med., 1994, 17, 268–277
Huang C.L., Sun L., Moonga B.S., Zaidi M., Molecular physiology and pharmacology of calcitonin, Cellular and molecular biology (Noisyle-Grand, France), 2006, 52, 33–43
Foster G.V., Calcitonin (thyrocalcitonin), N. Engl. J. Med., 1968, 279, 349–360
Haymovits A., Rosen J.F., Calcitonin in metabolic disorders, Adv. Metab. Disord., 1972, 60, 177–212
Huang R., Vivekanandan S., Brender J.R., Abe Y., Naito A., Ramamoorthy A., NMR characterization of monomeric and oligomeric conformations of human calcitonin and its interaction with EGCG, J. Mol. Biol., 2012, 416, 108–120
Molinari M., Watt K.D., Kruszyna T., Nelson R., Walsh M., Huang W.Y., et al., Acute liver failure induced by green tea extracts: case report and review of the literature, Liver Transpl., 2006, 12, 1892–1895
Isbrucker R.A., Bausch J., Edwards J.A., Wolz E., Safety studies on epigallocatechin gallate (EGCG) preparations. Part 1: genotoxicity, Food Chem. Toxicol., 2006, 44, 626–635
Isbrucker R.A., Edwards J.A., Wolz E., Davidovich A., Bausch J., Safety studies on epigallocatechin gallate (EGCG) preparations. Part 3: teratogenicity and reproductive toxicity studies in rats, Food Chem. Toxicol., 2006, 44, 651–661
Isbrucker R.A., Edwards J.A., Wolz E., Davidovich A., Bausch J., Safety studies on epigallocatechin gallate (EGCG) preparations. Part 2: dermal, acute and short-term toxicity studies, Food Chem. Toxicol., 2006, 44, 636–650
Lambert J.D., Kennett M.J., Sang S., Reuhl K.R., Ju J., Yang C.S., Hepatotoxicity of high oral dose (−)-epigallocatechin-3-gallate in mice, Food Chem. Toxicol., 2010, 48, 409–416
Goodin M.G., Rosengren R.J., Epigallocatechin gallate modulates CYP450 isoforms in the female Swiss-Webster mouse, Toxicol. Sci., 2003, 76, 262–270
Kapetanovic I.M., Crowell J.A., Krishnaraj R., Zakharov A., Lindeblad M., Lyubimov A., Exposure and toxicity of green tea polyphenols in fasted and non-fasted dogs, Toxicology, 2009, 260, 28–36
Guengerich F.P., Cytochrome p450 and chemical toxicology, Chem. Res. Toxicol., 2008, 21, 70–83
Huynh H.T., Teel R.W., Effects of plant-derived phenols on rat liver cytochrome P450 2B1 activity, Anticancer Res., 2002, 22, 1699–1703
Ullmann U., Haller J., Decourt J.P., Girault N., Girault J., Richard-Caudron A.S., et al., A single ascending dose study of epigallocatechin gallate in healthy volunteers, J. Int. Med. Res., 2003, 31, 88–101
Chow H.H., Hakim I.A., Vining D.R., Crowell J.A., Ranger-Moore J., Chew W.M., et al., Effects of dosing condition on the oral bioavailability of green tea catechins after single-dose administration of Polyphenon E in healthy individuals, Clin. Cancer Res., 2005, 11, 4627–4633
Ullmann U., Haller J., Decourt J.D., Girault J., Spitzer V., Weber P., Plasma-kinetic characteristics of purified and isolated green tea catechin epigallocatechin gallate (EGCG) after 10 days repeated dosing in healthy volunteers, International journal for vitamin and nutrition research. Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. Int. J. Vitam. Nutr. Res., 2004, 74, 269–278
Chow H.H., Cai Y., Hakim I.A., Crowell J.A., Shahi F., Brooks C.A., et al., Pharmacokinetics and safety of green tea polyphenols after multipledose administration of epigallocatechin gallate and polyphenon E in healthy individuals, Clin. Cancer Res., 2003, 9, 3312–3319
Hsu C.H., Liao Y.L., Lin S.C., Tsai T.H., Huang C.J., Chou P., Does supplementation with green tea extract improve insulin resistance in obese type 2 diabetics? A randomized, double-blind, and placebocontrolled clinical trial, Altern. Med. Rev., 2011, 16, 157–163
Jimenez-Saenz M., Martinez-Sanchez Mdel C., Acute hepatitis associated with the use of green tea infusions, J. Hepatol., 2006, 44, 616–617
Crew K.D., Brown P., Greenlee H., Bevers T.B., Arun B., Hudis C., et al., Phase IB randomized, double-blinded, placebo-controlled, dose escalation study of polyphenon E in women with hormone receptor-negative breast cancer, Cancer Prev. Res., 2012, 5, 1144–1154
Bonkovsky H.L., Hepatotoxicity associated with supplements containing Chinese green tea (Camellia sinensis), Ann. Intern. Med., 2006, 144, 68–71
Mazzanti G., Menniti-Ippolito F., Moro P.A., Cassetti F., Raschetti R., Santuccio C., et al., Hepatotoxicity from green tea: a review of the literature and two unpublished cases, Eur. J. Clin. Pharmacol., 2009, 65, 331–341
Attar A., Chan W.-T.C., Klärner F.-G., Schrader T., Bitan G., Safety and pharmacokinetic characterization of the molecular tweezer CLR01 in vivo, 2013, Manuscript in preparation
Obach R.S., Walsky R.L., Venkatakrishnan K., Gaman E.A., Houston J.B., Tremaine L.M., The utility of in vitro cytochrome P450 inhibition data in the prediction of drug-drug interactions, J. Pharmacol. Exp. Ther., 2006, 316, 336–348
Williamson G., Dionisi F., Renouf M., Flavanols from green tea and phenolic acids from coffee: critical quantitative evaluation of the pharmacokinetic data in humans after consumption of single doses of beverages, Mol. Nutr. Food Res., 2011, 55, 864–873
Yang C.S., Chen L., Lee M.J., Balentine D., Kuo M.C., Schantz S.P., Blood and urine levels of tea catechins after ingestion of different amounts of green tea by human volunteers, Cancer Epidemiol. Biomarkers Prev., 1998, 7, 351–354
Chow H.H., Cai Y., Alberts D.S., Hakim I., Dorr R., Shahi F., et al., Phase I pharmacokinetic study of tea polyphenols following single-dose administration of epigallocatechin gallate and polyphenon E, Cancer Epidemiol. Biomarkers Prev., 2001, 10, 53–58
Renouf M., Guy P., Marmet C., Longet K., Fraering A.L., Moulin J., et al., Plasma appearance and correlation between coffee and green tea metabolites in human subjects, Br. J. Nutr., 2010, 104, 1635–1640
Van Amelsvoort J.M., Van Hof K.H., Mathot J.N., Mulder T.P., Wiersma A., Tijburg L.B., Plasma concentrations of individual tea catechins after a single oral dose in humans, Xenobiotica, 2001, 31, 891–901
Lee M.J., Wang Z.Y., Li H., Chen L., Sun Y., Gobbo S., et al., Analysis of plasma and urinary tea polyphenols in human subjects, Cancer Epidemiol. Biomarkers Prev., 1995, 4, 393–399
Mateos R., Goya L., Bravo L., Uptake and metabolism of hydroxycinnamic acids (chlorogenic, caffeic, and ferulic acids) by HepG2 cells as a model of the human liver, J. Agric. Food Chem., 2006, 54, 8724–8732
Meng X., Sang S., Zhu N., Lu H., Sheng S., Lee M.J., et al., Identification and characterization of methylated and ring-fission metabolites of tea catechins formed in humans, mice, and rats, Chem. Res. Toxicol., 2002, 15, 1042–1050
Walle T., Methylation of dietary flavones greatly improves their hepatic metabolic stability and intestinal absorption, Mol. Pharm., 2007, 4, 826–832
Maeda-Yamamoto M., Ema K., Monobe M., Tokuda Y., Tachibana H., Epicatechin-3-O-(3″-O-methyl)-gallate content in various tea cultivars (Camellia sinensis L.) and its in vitro inhibitory effect on histamine release, J. Agric. Food Chem., 2012, 60, 2165–2170
Harada M., Kan Y., Naoki H., Fukui Y., Kageyama N., Nakai M., et al., Identification of the major antioxidative metabolites in biological fluids of the rat with ingested (+)-catechin and (−)-epicatechin, Biosci. Biotechnol. Biochem., 1999, 63, 973–977
Giunta B., Hou H., Zhu Y., Salemi J., Ruscin A., Shytle R.D., et al., Fish oil enhances anti-amyloidogenic properties of green tea EGCG in Tg2576 mice, Neurosci. Lett., 2010, 471, 134–138
Sang S., Lee M.J., Hou Z., Ho C.T., Yang C.S., Stability of tea polyphenol (−)-epigallocatechin-3-gallate and formation of dimers and epimers under common experimental conditions, J. Agric. Food Chem., 2005, 53, 9478–9484
Ishii T., Mori T., Tanaka T., Mizuno D., Yamaji R., Kumazawa S., et al., Covalent modification of proteins by green tea polyphenol (−)-epigallocatechin-3-gallate through autoxidation, Free Radic. Biol. Med., 2008, 45, 1384–1394
Sato M., Murakami K., Uno M., Nakagawa Y., Katayama S., Akagi K.I., et al., Site-specific inhibitory mechanism for amyloid-β42 aggregation by catechol-type flavonoids targeting the Lys residues, J. Biol. Chem., 2013
Okada K., Wangpoengtrakul C., Osawa T., Toyokuni S., Tanaka K., Uchida K., 4-hydroxy-2-nonenal-mediated impairment of intracellular proteolysis during oxidative stress — Identification of proteasomes as target molecules, J. Biol. Chem., 1999, 274, 23787–23793
Qin Z., Hu D., Han S., Reaney S.H., Di Monte D.A., Fink A.L., Effect of 4-hydroxy-2-nonenal modification on α-synuclein aggregation, J. Biol. Chem., 2007, 282, 5862–5870
Perez M., Cuadros R., Smith M.A., Perry G., Avila J., Phosphorylated, but not native, tau protein assembles following reaction with the lipid peroxidation product, 4-hydroxy-2-nonenal, FEBS Lett., 2000, 486, 270–274
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Attar, A., Rahimi, F. & Bitan, G. Modulators of amyloid protein aggregation and toxicity: EGCG and CLR01. Translat.Neurosci. 4, 385–409 (2013). https://doi.org/10.2478/s13380-013-0137-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2478/s13380-013-0137-y