Abstract
Background: Opioid rotation is currently the subject of considerable debate for two reasons: firstly as a strategy for pain treatment, and secondly because of the difficulty in determining equianalgesic doses. Switching from one slow-release (SR) opioid analgesic to another raises a number of critical issues, and there are no widespread studies that support a standard protocol. Initiation of opioid therapy must consider gradual dose titration of the drug until the minimum effective and maximum tolerated dosage for each patient is found.
Objective: This study aimed to evaluate the effects of SR opioid rotation after a stabilization period with normal-release (NR) morphine (‘start therapy’) in patients with cancer or non-cancer pain not controlled with their current SR opioid.
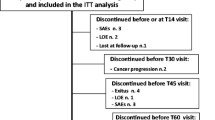
Methods: This is a multicentre, open-label, prospective study. A total of 326 consecutive patients were enrolled who were affected by chronic cancer or non-cancer pain that was not controlled by an SR opioid administered as either monotherapy or in combination with other analgesic drugs. Following start therapy with oral NR morphine at a dosage of 5 mg or 10 mg every 4 hours, rotation to an SR opioid of a different type from that previously administered was carried out.
Results: After about 3 days of start therapy with NR morphine, rotation to an SR opioid allowed a significant decrease of both baseline pain and daily episodes of breakthrough pain. No significant difference was detected between dosages and type of opioid administered, both prior to and after the start therapy period with NR morphine.
Conclusions: Rotation to another opioid preceded by a brief period of opioid receptor resetting by start therapy with NR morphine allows a good level of pain control and avoids rotation to inappropriate opioid dosages or combinations analgesics.












Similar content being viewed by others
References
Hanks GW, Conno F, Cherny N, et al. Morphine and alternative opioids in cancer pain: the EAPC recommendations. Br J Cancer 2001 Mar 2; 84(5): 587–93
Ripamonti CI, Campa T, Fagnoni E, et al. Normal-release oral morphine starting dose in cancer patients with pain. Clin J Pain 2009 Jun; 25(5): 386–90
Gatti A, Reale C, Occhioni R, et al. Standard therapy with opioids in chronic pain management: ORTIBER study. Clin Drug Investig 2009; 29Suppl. 1: 17–23
Geppetti P, Benemei S. Pain treatment with opioids: achieving the minimal effective and the minimal interacting dose. Clin Drug Investig 2009; 29Suppl. 1: 3–16
Mercadante S, Porzio G, Ferrera P, et al. Sustained-release oral morphine versus transdermal fentanyl and oral methadone in cancer pain management. Eur J Pain 2008 Nov; 12(8): 1040–6
Klepstad P, Kaasa S, Jystad A, et al. Immediate- or sustained-release morphine for dose finding during start of morphine to cancer patients: a randomized, double-blind trial. Pain 2003 Jan; 101(1-2): 193–8
Fine PG, Portenoy RK. Establishing “best practices” for opioid rotation: conclusions of an expert panel. J Pain Symptom Manage 2009 Sep; 38(3): 418–25
Knotkova H, Fine PG, Portenoy RK. Opioid rotation: the science and the limitations of the equianalgesic dose table. J Pain Symptom Manage 2009 Sep; 38(3): 426–39
Shaheen PE, Walsh D, Lasheen W, et al. Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manage 2009 Sep; 38(3): 409–17
De Conno F, Ripamonti C, Fagnoni E, et al. The MERITO Study: a multicentre trial of the analgesic effect and toler-ability of normal-release oral morphine during ‘titration phase’ in patients with cancer pain. Palliat Med 2008 Apr; 22(3): 214–21
Gordon DB, Dahl JL, Miaskowski C, et al. American pain society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch Intern Med 2005 Jul 25; 165(14): 1574–80
Ambrosio F, Finco G, Mattia C, et al. SIAARTI recommendations for chronic noncancer pain. Minerva Anestesiol 2006 Nov; 72(11): 859–80
Mercadante S. Opioid rotation for cancer pain: rationale and clinical aspects. Cancer 1999 Nov 1; 86(9): 1856–66
Duttaroy A, Yoburn BC. The effect of intrinsic efficacy on opioid tolerance. Anesthesiology 1995 May; 82(5): 1226–36
Adams JU, Paronis CA, Holtzman SG. Assessment of relative intrinsic activity of mu-opioid analgesics in vivo by using beta-funaltrexamine. J Pharmacol Exp Ther 1990 Dec; 255(3): 1027–32
Nickerson M. Receptor occupancy and tissue response. Nature 1956 Sep 29; 178(4535): 697–8
Stephenson RP. A modification of receptor theory. Br J Pharmacol Chemother 1956 Dec; 11(4): 379–93
Acknowledgements
The authors thank Nila Bhana of inScience Communications, a Wolters Kluwer business, who provided English-language and editorial assistance in the preparation of this article. This assistance was funded by Molteni Farmaceutici, Inc., Italy. The authors also thank Ennio Sarli (Centro Consulenze, Florence, Italy) for data analysis and statistical support. No external funding was received to conduct the study. The authors have no potential conflicts of interest that are directly relevant to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gatti, A., Reale, C., Luzi, M. et al. Effects of Opioid Rotation in Chronic Pain Patients. Clin. Drug Investig. 30 (Suppl 2), 39–47 (2010). https://doi.org/10.2165/1158413-S0-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/1158413-S0-000000000-00000