Summary
Synopsis
When used to treat patients with Parkinson’s disease pergolide acts at dopamine receptors in the corpus striatum to improve locomotor activity, reducing the tremor, gait disturbances, bradykinesia or akinesia and rigidity experienced by such patients. Treatment with pergolide often allows substantial reductions in concomitant levodopa dosage, and occasionally levodopa can be completely replaced by pergolide therapy in short term use. Pergolide has a long duration of action, thus reducing the wearing-off and end-of-dose phenomena frequently seen with long term levodopa therapy, suppressing fluctuations in levodopa response, and increasing total ‘on’ time. Despite a lack of well controlled studies comparing this drug with other dopamine agonist agents, pergolide appears to result in adverse effects and anti-Parkinson responses similar to those of bromocriptine and lisuride.
Thus, pergolide would appear to be at least as useful as other dopamine agonists such as bromocriptine or lisuride for the management of patients with Parkinson’s disease when administered in combination with levodopa. Future research should be directed towards establishing which patients are most likely to benefit from pergolide therapy, and clarifying the relative efficacy and safety of the anti-Parkinsonian drugs available to the clinician. If pergolide does provide clinical benefit when substituted for levodopa-adjunct drugs that are producing less than optimal control, this will be an advantage in a disease area which at present has few therapeutic options.
Pharmacological and Pharmacokinetic Properties
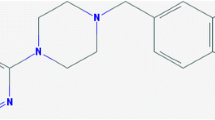
Pergolide is a dopamine receptor agonist which acts at both D1 and D2 receptors in the nigrostriatal regions of the brain where it affects locomotor activity, exemplified by circling behaviour in lesioned rats. It stimulates adenylate cyclase activity via D1 receptors in the corpus striatum in a manner similar to dopamine and has minor α2-stimulating activity which may cause a vasopressor response at high doses.
Pergolide initially increases serum corticosterone levels in rats, possibly via central dopamine receptors, but tolerance to this effect develops after as little as 5 days of continuous administration. Pergolide 0.0075 mg/kg reduces blood pressure in normotensive dogs by 17% although 0.03 mg/kg caused an initial 25% increase in pressure; larger reductions of blood pressure occur in hypertensive animals. Similarly, heart rate, blood pressure and plasma dopamine, norepinephrine (noradrenaline) and lactic acid levels are reduced at rest and/or during exercise when pergolide 0.05 mg/day is administered to healthy volunteers. The hypotensive effects of the drug are dose proportionate and tend to diminish with continued treatment of patients. Pergolide appears devoid of effects on glucose metabolism in either animals or patients with Parkinson’s disease. Furthermore, pergolide reduces intraocular pressure in healthy volunteers and causes significant reductions in prolactin levels at rest and during exercise. In animal models of Parkinson’s disease, pergolide has induced Stereotypic behaviour in rats and guinea-pigs by direct stimulation of striatal dopamine receptors. In rats, pre- and postsynaptic dopamine receptors may play a part in decreases and increases in locomotor activity, respectively. Increased locomotion is accompanied by stereotypy and could be sustained for long periods. Effects of the drug on prolactin levels appear to last 24 hours or more and although its duration of activity in Parkinson’s disease is shorter, it still exceeds that of levodopa. The onset of action against Parkinson’s disease symptoms in 8 patients occurred in 80 minutes and effects lasted a mean of 5.5 hours.
Pergolide is rapidly absorbed from the gastrointestinal tract, reaching peak plasma concentrations within 1 to 2 hours. Complete elimination of a single radiolabelled dose from the body is achieved within 4 to 5 days, with a mean elimination half-life of 27 hours. Pergolide is 90% bound to plasma proteins. 55% of a radioactive dose is eliminated via the kidneys, 5% via the lungs and the remainder by the liver. Pergolide appears to concentrate in dopamine-rich areas of the brain such as the corpus striatum.
Therapeutic Trials
In short term noncomparative studies (less than 3 months) in Parkinson’s disease, administration of pergolide frequently results in reduced levodopa requirements (complete withdrawal has occasionally been possible), reduced disability and decreased ‘off’ time in patients who no longer respond reliably to bromocriptine and/or levodopa. Placebo-controlled studies demonstrate that mean daily dosages of pergolide 2.5 to 4.6mg result in a 33 to 78% reduction in the requirement for levodopa while improving the duration and extent of response to the latter and reducing the total duration of ‘off’ time by 1.4 to 2.8 hours per day. However, switching from pergolide to placebo results in deterioration of symptoms in all patients. Sleep disturbances tend to be suppressed by pergolide in some patients with Parkinson’s disease.
Long term (6 months to 7 years) studies of pergolide show that both disability and levodopa dosage tend to be reduced and mobility improved, with the most persistent responses seen in patients who achieved the greatest initial benefit. Peak clinical improvement appears to occur after 2 to 12 months and results may diminish slowly thereafter, although some patients continue to respond for up to 7 years without increasing pergolide or levodopa dosages. Previous response to bromocriptine is not predictive of likely outcome with pergolide since, in a small study involving 25 patients, 50% of individuals who did not improve on bromocriptine gained significant benefit when switched to pergolide.
When compared with bromocriptine in a double-blind crossover study, pergolide induced similar improvements in gait, tremor, rigidity and dyskinesia, with slightly more patients preferring to continue pergolide at the end of 14 to 20 weeks of study. If efficacy with bromocriptine or pergolide decreases, the substitution of pergolide for bromocriptine appears more likely to be clinically beneficial than the switch to bromocriptine after pergolide therapy. Comparisons of pergolide with lergotrile, lisuride, and mesulergine have usually been of one-way crossover design, and while similar responses have been seen in a small number of patients, some studies show marginally more favourable responses to pergolide. However, given the limited nature of these clinical trials any conclusions regarding relative efficacy must remain tentative. De novo monotherapy with pergolide has shown limited promise. However, use of pergolide combined with levodopa in the early therapy of Parkinson’s disease may yet prove to delay the onset of levodopa related adverse effects.
Adverse Effects
Overall, pergolide appears to be relatively well-tolerated in patients with Parkinson’s disease, although adverse effects have resulted in discontinuation of therapy in 27% of patients in clinical trials. The most frequently reported adverse effects during pergolide treatment have been dyskinesias, nausea, dizziness, hallucinations, rhinitis and other CNS or gastrointestinal symptoms.
ECG changes and other cardiac effects have been noted infrequently, but close observation may be required in patients with prior heart disease. Occasional first-dose postural hypotension makes gradual introduction and increments of pergolide dosage advisable. Rarely, abrupt withdrawal of the drug has resulted in confusion or hallucinations, so if pergolide therapy needs to be stopped it is prudent to discontinue the drug gradually if at all possible. In general, long term use of the drug does not adversely alter neuro-psychological parameters.
Dosage and Administration
When used to treat Parkinson’s disease, slow incremental increases in oral dosage of pergolide are recommended, beginning with 0.05 mg/day and increasing by 0.05 to 0.15 mg/day every third day for 2 weeks, then by 0.25 mg/day every third day until an optimum dosage is reached. Reductions in concomitant levodopa dosages may be required. Dosages of 2 to 4 mg/day are most common, administered in 3 to 4 divided oral doses. The effects of dosages above 5 mg/day have not been fully examined.
Similar content being viewed by others
References
Ahlskog JE, Muenter MD. Treatment of Parkinson’s disease with pergolide: a double-blind study. Mayo Clinic Proceedings 63: 969–978, 1988a
Ahlskog JE, Muenter MD. Pergolide: long-term use in Parkinson’s disease. Mayo Clinic Proceedings 63: 979–987, 1988b
Al-Sereiti MR, Quik RFP, Turner P. The effect of a single oral dose of pergolide on intraocular pressure and pupil diameter. British Journal of Clinical Pharmacology 28: 263–268, 1989
Arneric SP, Chow SA, Long JP, Fischer LJ. Inhibition of insulin release from rat pancreatic islets by drugs that are analogues of dopamine. Diabetes 33: 888–893, 1984
Arnt J, Begese KP, Hyttel J, Meier E. Relative dopamine D1 and D2 receptor affinity and efficacy determine whether dopamine agonists induce hyperactivity or oral stereotypy in rats. Pharmacology & Toxicology 62: 121–130, 1988
Arnt J, Hyttel J. Inhibition of SKF 38393-and pergolide-induced circling in rats with unilateral 6-OHDA lesion is correlated to dopamine D-1 and D-2 receptor affinities in vitro. Journal of Neural Transmission 67: 225–240, 1986
Askenasy JJM, Yahr MD. Reversal of sleep disturbance in Parkinson’s disease by antiparkinsonian therapy: a preliminary study. Neurology 35: 527–532, 1985
Barrett RJ, Lokhandwala MF. Dopaminergic inhibition of cardiac sympathetic nerve function by pergolide European Journal of Pharmacology 77: 79–83, 1982
Blackwell RE, Bradley EL, Kline LB, Duvall ER, Vitek JJ, et al. Comparison of dopamine agonists in the treatment of hyper-prolactinemic syndromes: a multicenter study. Fertility and Sterility 39: 744–748, 1983
Boyce S, Jenner P, Marsden CD. Alterations in brain dopamine receptor function following chronic administration of L-Dopa, bromocriptine or pergolide to rats. British Journal of Pharmacology 86: 632P, 1985
Cavero I, Lorrain J, Di Paola ED, Lhoste F, Payen B, et al. Pharmacological, hemodynamic and biochemical mechanisms involved in the blood pressure lowering effects of pergolide, in normotensive and hypertensive dogs. Journal of Pharmacology and Experimental Therapeutics 235: 798–809, 1985
Claustre Y, Fage D, Zivkovic B, Scatton B. Relative selectivity of 6,7-dihydroxy-2-dimethylaminotetrelin, N-n-propyl-3-(3-hydroxyphenyl) piperidine, N-n-propylnorapomorphine and pergolide as agonists at striatal dopamine autoreceptors and postsynaptic dopamine receptors. Journal of Pharmacology and. Experimental Therapeutics 232: 519–525, 1985
Critchley P, Langdon N, Parkes JD, Quinn NP, Shindler JS. Domperidone. British Medical Journal 290: 788, 1985
De Meirleir K, Baeyens L, L’Hermite M, L’Hermite-Balériaux M, Olbrecht J, et al. Pergolide mesylate inhibits exercise-induced prolactin release in man. Fertility and Sterility 43: 628–631, 1985
De Meirleir KJ, Gerlo F, Hollmann W, Vanhaelst L. Cardiovascular effects of pergolide mesylate during dynamic exercise. British Journal of Clinical Pharmacology 23: 633P, 1987
Diamond SG, Markham CH. Evaluating the evaluations: or how to weigh the scales of parkinsonian disability. Neurology 33: 1098–1099, 1983
Diamond SG, Markham CH. One-year trial of pergolide as an adjunct to sinemet in treatment of Parkinson’s disease. Advances in Neurology 40: 537–539, 1984
Diamond SG, Markham CH, Treciokas LJ. Double-blind trial of pergolide for Parkinson’s disease. Neurology 35: 291–295, 1985
Factor SA, Sanchez-Ramos JR, Weiner WJ. Parkinson’s disease: an open label trial of pergolide in patients failing bromocriptine therapy. Journal of Neurology, Neurosurgery and Psychiatry 51: 529–533, 1988
Fischer PA. Antiparkinson drugs. Drugs of Today 23: 87–99, 1987
Franks S, Horrocks PM, Lynch SS, Butt WR, London DR. Effectiveness of pergolide mesylate in long term treatment of hyperprolactinaemia. British Medical Journal 286: 1177–1179, 1983
Fuller RW, Clemens JA, Hynes MD. Degree of selectivity of pergolide as an agonist at presynaptic versus postsynaptic dopamine receptors: implications for prevention or treatment of tardive dyskinesia. Journal of Clinical Psychopharmacology 2: 371–375, 1982
Fuller RW, Snoddy HD. Elevation of serum corticosterone concentrations in rats by pergolide and other dopamine agonists. Endocrinology 109: 1026, 1981
Goetz CG, Tanner CM, Glantz R, Klawans HL. Pergolide in Parkinson’s disease. Archives of Neurology 40: 785–787, 1983
Goetz CG, Tanner CM, Glantz RH, Klawans HL. Chronic agonist therapy for Parkinson’s disease: A 5-year study of bromocriptine and pergolide. Neurology 35: 749–751, 1985
Goldstein M, Lieberman A, Lew JY, Asano T, Rosenfeld MR, et al. Interaction of pergolide with central dopaminergic receptors. Proceedings of the National Academy of Sciences USA 77: 3725–3728, 1980
Gonce M, Delwaide PJ. Etude clinique du pergolide dans la maladie de Parkinson. Presse Médicale 14: 1409–1411, 1985
Grimes D, Hassan M, Mireles R, Garner P. Experience with pergolide mesylate in severe Parkinson’s disease. Canadian Journal of Neurological Sciences 9: 293, 1982
Grimes JD, Hassan MN, Sitwell LD, Gray P, Payne LW. Pergolide in the management of advanced Parkinson’s disease. Canadian Journal of Neurological Sciences 12: 173, 1985
Gust CM, Fuller RW. Further characterization of tolerance to the corticosterone-elevating effect of pergolide in rats. Neuroscience Letters 93: 307–311, 1988
Hahn RA. Development of selective dopamine receptor agonists as novel cardiovascular drugs. Drug Development Research 4: 285–300, 1984
Hoehn MM, Yahr MD. Parkinsonism: onset, progression, and mortality. Neurology 17: 427–442, 1967
Hurtig HI, Saykin A, Stern MB, Melvin G, Cline S, et al. Pergolide improves motor function in Parkinson’s disease without causing adverse mental effects: a neuropsychological study. Neurology 35: 202, 1985
Hynes MD, Fuller RW, Hymson D. Biphasic effects of selected dopamine agonists on locomotor activity: differential effects in normotensive and hypertensive rats. Pharmacologist 24: 197, 1982
Ilson J, Fahn S, Mayeux R, Cote L. Pergolide treatment in parkinsonism. In Calne et.al. (Eds) Lisuride and other dopamine agonists, pp. 443–451, Raven Press, New York, 1983
Jankovic J. Controlled trial of pergolide mesylate in Parkinson’s disease and progressive supranuclear palsy. Neurology 33: 505–507, 1983
Jankovic J. Long-term study of pergolide in Parkinson’s disease. Neurology 35: 296–299, 1985
Jankovic J, Orman J. Parallel double-blind study of pergolide in Parkinson’s disease. In Yahr & Bergmann (Eds) Advances in neurology, Vol. 45, pp. 551–554, Raven Press, New York, 1986
Jeanty P, Van den Kerchove M, Lowenthal A, De Bruyne H. Pergolide therapy in Parkinson’s disease. Journal of Neurology 231: 148–152, 1984
Jiang D-H, Reches A, Wagner HR, Fahn S. Biochemical and behavioral evaluation of pergolide as a dopamine agonist in the rat brain. Neuropharmacology 23: 295–301, 1984
Johnston DG, Hall K, Kendall-Taylor P, Patrick D, Watson M, et al. Effect of dopamine agonist withdrawal after long-term therapy in prolactinomas studies with high-definition computerised tomography. Lancet 2: 187–192, 1984
Jungmann E, Haak T, Althoff P-H, Fassbinder W, Schöffling K. Dopaminergic effects on kidney function and responsiveness of aldosterone, plasma renin activity, prolactin, catecholamines, and blood pressure to stimulation in patients with prolactinoma: comparison of the efficacy of pergolide and bromocriptine therapy. Arzneimittel-Forschung 38: 296–300, 1988
Klawans HL, Tanner CM, Glatt S, Goetz CG. A 6-month trial of pergolide mesylate in the treatment of idiopathic Parkinson’s, disease. In Fahn et al. (Eds) Advances in neurology: experimental therapeutics of movement disorders, Vol. 37, pp. 75–83, Raven Press, New York, 1983
Klawans HL, Tanner CM, Goetz CG, Glatt S, Nausieda P. Pergolide mesylate therapy in Parkinson disease: report of a 3-month trial in 20 patients. Neurology 31: 133, 1981
Kleinberg DL, Boyd AE, Wardlaw S, Frantz AG, George A, et al. Pergolide for the treatment of pituitary tumors secreting prolactin or growth hormone. New England Journal of Medicine 309: 704–709, 1983
Kleinberg DL, Lieberman A, Todd J, Greising J, Neophytides A, et al. Pergolide mesylate: a potent day-long inhibitor of prolactin in rhesus monkeys and patients with Parkinson’s disease. Journal of Clinical Endocrinology and Metabolism 51: 152–154, 1980
Kletzky OA, Borenstein R, Mileikowsky GN. Pergolide and bromocriptine for the treatment of patients with hyperprolactinemia. American Journal of Obstetrics and Gynecology 154: 431–435, 1986
Koller WC, Weiner WJ, Diamond BI, Nausieda PA, Klawans HL. The pharmacological evaluation of pergolide mesylate as a potential anti-Parkinson agent. Neuropharmacology 19: 831–837, 1980
Kurlan R, Miller C, Knapp R, Murphy G, Shoulson I. Double-blind assessment of potential pergolide-induced cardiotoxicity. Neurology 36: 993–995, 1986
Kurlan R, Miller C, Levy R, Macik B, Hamill R, et al. Long-term experience with pergolide therapy of advanced parkinsonism. Neurology 35: 738–742, 1985
Lang AE, Quinn N, Brincat S, Marsden CD, Parkes JD. Pergolide in late-stage Parkinson disease. Annals of Neurology 12: 243–247, 1982
Lees AJ, Stern GM. Pergolide and lisuride for levodopa-induced oscillations. Lancet 2: 577, 1981
Leibowitz M, Lieberman A, Goldstein M, Neophytides A, Kupersmith M, et al. Cardiac effects of pergolide. Clinical Pharmacology and Therapeutics 30: 718–723, 1981
Lemberger L, Crabtree R, Callaghan JT. Pergolide, a potent long-acting dopamine-receptor agonist. Clinical Pharmacology and Therapeutics 27: 642–651, 1980
LeWitt PA, Ward CD, Larsen TA, Raphaelson MI, Newman RP, et al. Comparison of pergolide and bromocriptine therapy in parkinsonism. Neurology 33: 1009–1014, 1983
L’Hermite M, Debusschere P. Potent 48 hours inhibition of prolactin secretion by pergolide in hyperprolactinaemic women. Acta Endocrinologica 101: 481–483, 1982
L’Hermite M, Debusschere PM, Gillet C, Deschepper C. Treatment of hyperprolactinaemic patients with pergolide. Acta Endocrinologica 103: 441–445, 1983
Lichter D, Kurlan R, Miller C, Shoulson I. Does pergolide slow the progression of Parkinson’s disease? A 7-year follow-up study. Neurology 38(3): 122, 1988
Lieberman A, Goldstein M, Leibowitz M, Neophytides, A, Kupersmith M, et al. Treatment of advanced Parkinson disease with pergolide. Neurology 31: 675–682, 1981
Lieberman AN, Goldstein M, Gopinathan G, Leibowitz M, Neophytides A, et al Further studies with pergolide in Parkinson disease. Neurology 32: 1181–1184, 1982b
Lieberman AN, Goldstein M, Leibowitz M. Comparative efficacy of two dopamine agonists, pergolide and lergotrile, in Parkinson disease. New York State Journal of Medicine 88: 420–422, 1988
Lieberman AN, Goldstein M, Leibowitz M, Gopinathan G, Neophytides A. Long-term treatment with pergolide: decreased efficacy with time. Neurology 34: 223–226, 1984b
Lieberman AN, Goldstein M, Neophytides A, Leibowitz M, Gopinathan G, et al. The use of pergolide, a potent dopamine agonist, in Parkinson’s disease. Clinical Pharmacology and Therapeutics 32: 70–75, 1982a
Lieberman AN, Gopinathan G, Neophytides A. Efficacy of pergolide and mesulergine. European Neurology 25: 86–90, 1986
Lieberman AN, Gopinathan G, Neophytides A, Leibowitz M, Goldstein M. Pergolide and lisuride in advanced Parkinson’s disease. In Hassler & Christ (Eds) Advances in neurology, Vol. 40, pp. 503–507, Raven Press, New York, 1984a
Lieberman AN, Leibowitz M, Neophytides A, Kupersmith M, Mehl S, et al. Pergolide and lisuride for Parkinson’s disease. Lancet 2: 1129–1130, 1979
Lieberman AN, Neophytides A, Leibowitz M, Gopinathan G, Pact V, et al. Comparative efficacy of pergolide and bromocriptine in patients with advanced Parkinson’s disease. Advances in Neurology 37: 95–108, 1983
Lieberman A, Neophytides A, Leibowitz M, Kupersmith M, Pact V, et al. The use of two new dopamine agonists: pergolide and lisuride in Parkinson’s disease. In Rinne et al. (Eds) Parkinson’s disease-current progress, problems and management, pp 335–356, Elsevier, Amsterdam, 1980
McHale DM, Sage JI. Hallucinations and confusion after pergolide withdrawal. Clinical Neuropharmacology 11: 545–548, 1988
Mear J-Y, Barroche G, de Smet Y, Weber M, Lhermitte F, et al. Pergolide in the treatment of Parkinson’s disease. Neurology 34: 983–986, 1984
Monk BE, Parkes JD, Du Vivier A. Erythromelalgia following pergolide administration. British Journal of Dermatology 111: 97–99, 1984
Nielsen EB, Randrup K, Andersen PH. Amphetamine discrimination: effects of dopamine receptor agonists. European Journal of Pharmacology 160: 253–262, 1989
Olanow CW. Pergolide, parlodel crossover study. Neurology 38(3): 314, 1988
Olanow CW, Alberts MJ. Double-blind controlled study of pergolide mesylate in the treatment of Parkinson’s disease. Clinical Neuropharmacology 10: 178–185, 1987
Perryman RL, Rogol AD, Kaiser DL, MacLeod RM, Thorner MO. Pergolide mesylate: its effects on circulatory anterior pituitary hormones in man. Journal of Clinical Endocrinology and Metabolism 53: 772–778, 1981
Potter DE, Burke JA. Ocular effects of lergotrile, pergolide and bromocriptine. Federation Proceedings 41: 1057, 1982
Quinn NP, Lang AE, Thompson C, Brincat S, Marsden CD, et al. Pergolide in the treatment of Parkinson’s disease. In Hassler & Christ (Eds) Advances in neurology, Vol. 40, pp. 509–513, Raven Press, New York, 1984
Quinn NP, Toone B, Lang AE, Marsden CD, Parkes JD. Dopa dose-dependent sexual deviation British Journal of Psychiatry 142: 296–298, 1983
Richardson EP, Beal MF, Martin JB. Degenerative diseases of the nervous system. In Braunwald et al. (Eds) Harrison’s principles of internal medicine, 11th ed., McGraw Hill Book Company, New York, 1987
Rinne UK. Dopamine agonists as primary treatment in Parkinson’s disease. Advances in Neurology 45: 519–523, 1986
Rinne UK. Early combination of bromocriptine and levodopa in the treatment of Parkinson’s disease: a 5-year follow up. Neurology 37: 826–828, 1987
Rinne UK. Lisuride, a dopamine agonist in the treatment ofearly Parkinson’s disease. Neurology 39: 336–339, 1989
Rougemont D, Baron JC, Collard P, Bustany P, Comar D, et al. Local cerebral glucose utilisation in treated and untreated patients with Parkinson’s disease. Journal of Neurology, Neurosurgery, and Psychiatry 47: 824–830, 1984
Rubin A, Lemberger L, Dhahir P. Physiologic disposition of pergolide. Clinical Pharmacology and Therapeutics 30: 258–265, 1981
Ruffolo RR, Cohen ML, Messick K, Horng JS. Alpha-2-adrenoceptor-mediated effects of pergolide. Pharmacology 35(3): 148–154, 1987
Sage JI, Duvoisin RC. Pergolide therapy in Parkinson’s disease: a double-blind, placebo-controlled study. Clinical Neuropharmacology 8(3): 260–265, 1985
Sage JI, Duvoisin RC. Long-term efficacy of pergolide in patients with Parkinson’s disease. Clinical Neuropharmacology 9: 160–164, 1986
Schmidt MJ, Root MA, Hall JL. Dopamine agonist-induced hyperglycemia in rats: structure-activity relationships and mechanisms of action. European Journal of Pharmacology 90: 169–177, 1983
Shoulson I, Miller C, Kurlan R, Levy R, Macik B. Parkinsonism and on-off fluctuations: long-term effects of pergolide therapy. Annals of Neurology 12: 97, 1982
Stern Y, Mayeux R, Ilson J, Fahn S, Cote L. Pergolide therapy for Parkinson’s disease: neurobehavi oral changes. Neurology 34: 201–204, 1984
Tanner CM, Chhablani R, Goetz C, Klawans HL. Pergolide mesylate: lack of cardiac toxicity in patients with cardiac disease. Neurology 35: 918–921, 1985
Tanner CM, Goetz CG, Glantz RH, Glatt SL, Klawans HL. Pergolide mesylate and idiopathic Parkinson disease. Neurology 32: 1175–1179, 1982
Teychenne PF, Bergsrud D, Crabtree R. Double-blind placebo-controlled trial of pergolide in idiopathic Parkinson’s disease. Comparison of clinical response with plasma levels of pergolide. Neurology 38(3): 178, 1988
Weaver A, Basmadjian GP, Parikh A, Tolbert MEM. In vivo regional brain distribution of [Se-75]-pergolide in the rat: effects of various dopamine receptor agonists and antagonists. Journal of Nuclear Medicine 27: 906, 1986
Wong DT, Reid LR. Activation of adenylate cyclase in rat striatum by an ergoline dopamine agonist, pergolide. Communications in Psychopharmacology 4: 269–275, 1980
Wright A, Lees AJ, Stern GM. Mesulergine and pergolide in previously untreated Parkinson’s disease. Journal of Neurology, Neurosurgery, and Psychiatry 49: 482–484, 1986
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: J.E. Ahlskog, Department of Neurology, Mayo Clinic, Rochester, Minnesota, USA; J. Arnt, Psychopharmacological Section, Pharmacological Research, H. Lundbeck A/S, Copenhagen-Valby, Denmark; K. De Meirleir, Vrije Universiteit Brussel, Brussels, Belgium; S.G. Diamond, Reed Neurological Research Center, UCLA School of Medicine, Center for Health Sciences, Los Angeles, California, USA; E. Jungmann, Zentrum der Inneren Medizin, Abteilung fur Endokrinologie, Johann Wolfgang-Goethe-Universitat, Frankfurt Main, West Germany; A. Lieberman, Barrow Neurological Institute, Phoenix, Arizona, USA; C.D. Marsden, University Department of Clinical Neurology, Institute of Neurology, University of London, London, England; N.P. Quinn, University Department of Clinical Neurology, Institute of Neurology, University of London, London, England; C.M. Tanner, Department of Neurological Sciences, Rush-Presbyterian-St Luke’s Medical Center, Chicago, Illinois, USA.
Rights and permissions
About this article
Cite this article
Langtry, H.D., Clissold, S.P. Pergolide. Drugs 39, 491–506 (1990). https://doi.org/10.2165/00003495-199039030-00009
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199039030-00009