Summary
Coronary heart diseases (CHD) have high indices of mortality and morbidity. A number of CHD and myocardial ischaemic syndromes such as unstable angina pectoris, sudden death ischaemic heart disease, acute myocardial infarction and ventricular arrhythmias have been associated with losses of myocardial magnesium and potassium.
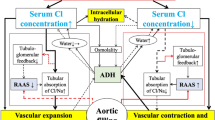
Mg++ ions are essential for regulation of Na+ and K+ transport across cell membranes, including those found in cardiac and vascular smooth muscle cells. Mg++ activates an Na+-K+-ATPase pump which in turn plays a major role in regulating Na+-K+ transport. Loss of cellular Mg++ results in loss of critically important phosphagens: MgATP and creatine phosphate. Thus, under conditions where cellular Mg++ is depleted (e.g. hypoxia, ischaemia, anoxia), the Na+-K+ pump and phosphagen stores will be compromised, leading to alterations in resting membrane potentials. Cellular Mg++ depletion has been found to result in concomitant depletion of K+ in a number of cells, including cardiac and vascular muscles. The consequences of these events are often production of cardiac arrhythmias. Myocardial and vascular injury lead to disturbances in electrolyte transport across cell membranes, whereby Na+ and Ca++ uptakes are enhanced and, just prior or concomitantly, Mg++ and K+ are lost. Such electrolyte disturbances often lead to necrotic foci.
Considerable evidence has accumulated to indicate that the extracellular concentracion of Mg++ is important in control of arterial tone and blood pressure via regulation of vascular membrane Mg++-Ca++ exchange sites. A reduction in the extracellular Mg++ concentracion can produce hypertension, coronary vasospasm and potentiation of vasoconstrictor agents by allowing excess entry of Ca++; concomitantly, the potency of vasodilator agents is reduced. Alterations in vascular membrane Mg++ result in arterial and nrteriolar membranes which are ‘leaky’, thus contributing to the cellular reduction in K+ and gain of Na+ and Ca+. Alterations in extracellular K+ or Na+ concentracions over physiological ranges, in the face of a Mg++ deficit, can exacerbate the coronary vasospasm noted with reduction in only extracellular Mg++. Since free Mg++ ions are necessary for maintaining Ca+ ions (both plasma membrane-bound and sarcoplasmic reticulum membrane-bound via Ca++ ATPases), intracellular free Mg++ would rise in conditions which result in cellular loss of Mg++, thereby exacerbating and contributing to elevation of blood pressure and coronary vasospasm. Data are also accumulating to suggest that Mg++ may control a Na+-Ca++ pump which is essential for maintenance of normal coronary vascular tone.
Overall, the available data suggest that Mg++ plays critical roles in maintenance of normal cardiac excitability and coronary vascular tone. Based on these and other findings reviewed herein, magnesium prophylaxis and intervention may be extremely useful in the prevention and treatment of CHD, sudden death ischaemic heart disease, hypertension and acute myocardial infarction.
Résumé
L’insuffisance coronarienne est grevée d’indices élevés de mortalité et de morbidité. Un certain nombre de formes cliniques d’insuffisance coronarienne et d’ischémie myocardique ont été mises en rapport avec un déficit en potassium et en magnésium. C’est le cas de l’angine de poitrine instable, de la mort subite par ischémie myocardique, de l’infarctus aigu du myocarde et des arythmies ventriculaires.
Les ions Mg++ sont essentiels au transport normal du Na+ et du K+ à travers la membrane cellulaire y compris celle du muscle cardiaque et celle du muscle vasculaire lisse. Le Mg++ active la Na+ -K+ -ATPase de la pompe membranaire laquelle régularise le transport Na+ -K+. Une perte de Mg + + cellulaire équivaut à une perte de phosphagènes dont le rôle est primordial à savoir le MgA TP et le phosphate de créatinine. Ainsi, dans les circonstances où existe une déplétion en Mg + + (i.e. l’hypoxie, l’ischémie, l’anoxie), le fonctionnement de la pompe Na+ -K+ et les réserves en phosphagènes sont compromises et il en résulte des altérations dans le potentiel membranaire de repos. La perte de Mg+ + entraîne une perte de K+ dans de nombreuses cellules y compris celles du coeur et du muscle vasculaire. La conséquence en est souvent le développement d’arythmies. Les altérations du myocarde et des vaisseaux coronaires conduit à des modifications du transport électrolytique à travers la membrane cellulaire où l’entrée de Na+ et de Ca+ sont facilités parallèlement à une perte de Mg+ + et K+. Ceci favorise la formation de foyers de nécrose.
On possède des preuves solides de l’importance de la concentration en Mg+ + extracellulaire dans le contrôle du tonus artériel et de la pression sanguine par le biais de sites d’échanges Mg + + -Ca + + au niveau de la membrane vasculaire. Une diminution du Mg+ + extracellulaire peut être à l’origine d’une réaction hypertensive, d’un spasme coronaire et d’une synergie d’effet avec des substances vasoconstrictrices en favorisant une entrée massive de Ca+ +. Parallèlement, l’effet des vasodilatateurs est diminué. Des modifications du Mg+ + de la membrane vasculaire rendent ‘perméables’ les artères et artérioles ce qui contribue à l’appauvrissement cellulaire en K+ et à son enrichissement en Na+ et Ca+ +. Une élévation du K+ ou du Na+ extracellulaires au-dessus des concentrations physiologiques accompagnée d’un déficit en Mg+ + peut renforcer le spasme coronaire observé avec la seule diminution de Mg + + extracellulaire. Puisque le Mg + + libre est indispensable au maintien d’un Ca+ + normal (Ca+ + lié à la membrane cytoplasmique et au réticulum endoplasmique via les Ca+ + ATPases) le Mg+ + libre intracellulaire s’élèverait dans les situations où existe une perte cellulaire de Mg + + contribuant de ce fait à une élévation de la pression sanguine et à un renforcement du spasme coronarien. Il existe aussi des données qui tendent à prouver que le Mg + + peut exercer un contrôle sur la pompe Na + -Ca + + qui est essentielle au maintien d’une tonicité normale des vaisseaux coronaires.
Au total, les données disponibles suggèrent que le Mg+ + joue un rôle fondamental dans le maintien d’un niveau normal d’excitabilité myocardique et de tonicité coronaire. Elles conduisent à penser que l’utilisation prophylactique et curative du magnésium est d’une grande utilité pour la prévention et le traitement de l’insuffisance coronarienne, la mort subite par ischémie myocardique, l’hypertension, l’infarctus aigu du myocarde.
Zusammenfassung
Koronare Herzkrankheiten (KHK) besitzen eine hohe Mortalitüt und Morbiditüt. Eine A nzahl von KHK und ischümischen Myokardsyndromen wie instabile Angina pectoris, plötzlicher Herztod bei ischümischer Herzkrankheit, akuter Herzinfarkt und ventrikulüre Arrhythmien wurden mit Verlusten an myokardialem Magnesium und Kalium in Verbindung gebracht.
Mg++ -Ionen sind für die Regulation des Na+ - und K+ -Transports durch die Zellmembran einschlieβlich der von kardialen und vaskulüren glatten Muskelzellen erforderlich. Mg+ + aktiviert die Na+ -K+ -ATPase die ihrerseits eine bedeutende Rolle für die Regulation des Na+ -K+ -Transports spielt. Ein Verlust an zellulürem Mg+ + führt zu Verlusten der kritisch wichtigen Phosphagene MgATP und Kreatinphosphat. Unter den Bedingungen, die zu einer zellulären Mg+ + -Erschöpfung führen (z.B. Hypoxie, Ischümie, Anoxie) wird die Funktion der Na+ -K+ -Pumpe und der Phosphagenspeicher beeinträchtigt was zu Veränderungen der Ruhemembranpotentiale führt. Es wurde nachgewiesen, daβ eine zellulüre Mg+ + -Verarmung in einer Anzahl von Zellen, einschlieβlich der Herz- und Gefäβmuskeln, eine gleichzeitige Verarmung an K+ ergibt. Die Konsequenzen dieser Ereignisse ist häufig das Auftreten von Herzarrhythmien. Myokardiale und vaskulüre Schüdigungen führen zu Störungen im Elektrolyttransport durch die Zellmembran, wodurch die Aufnahme von Na+ undCa+ + verstärkt und unmittelbar vorher oder gleichzeitig Mg+ + undK+ verloren gehen. Solche Elektrolytstörungen führen oft zu nekrotischen Bezirken.
Die vorliegenden Befunde zeigen daβ die extrazelluläre Konzentration von Mg+ + für die Kontrolle des arteriellen Tonus und Blutdrucks via Regulation der vaskulären Mg+ + -Ca+ + -Membranaustauschstellen wichtig ist. Eine Senkung der extrazellulären Mg+ + -Konzentration kann eine Hypertonie, koronare Vasospasmen und eine Potenzierung der Wirkung von Vasokonstriktoren durch einen gesteigerten Einstrom von Ca + + hervorrufen; gleichzeitig wird die Wirksamkeit von Vasodilatatoren vermindert. Veränderungen des Mg + + in der Gefäβmembran führen zu ‘durchlässigen’ und arteriolären Membranen, und begünstigen dadurch die Abnahme des intrazellulären K+ und Zunahme von Na+ und Ca+ +. Liegen neben dem Mg + + -Mangel Veränderungen der extrazellulären K+ - und Na+ -Konzentrationen vor, die über den physiologischen Bereich hinausgehen, kann dies zu einer weiteren Verschlimmerung der koronaren Vasospasmen führen. Da freie Mg++ -Ionen zum Erhalt von Ca++ -Ionen notwendig sind (sowohl über die Plasmamembran-gebundenen als auch am sarkoplasmatischen Retikulum Membran-gebundenen Ca+ + -ATPasen), steigt das intrazellulüre freie Mg+ + unter Bedingungen, die zu einem Verlust von zellulärem Mg + + und dadurch zu Exazerbationen und Beteiligungen an der Erhöhung des Blutdrucks und koronarer Vasospasmen führen. Es hüufen sich auch Hin weise, die vermuten lassen, daβ Mg + + eine Na+ -Ca++ -Pumpe kontrolliert, die zurAufrechterhaltung eines normalen Koronargefäβtonus erforderlich ist.
Insgesamt lassen die verfügbaren Daten vermuten, daβ Mg + + eine kritische Rolle für die Aufrechterhaltung der normalen kardialen Erregbarkeit und des koronaren Gefüβtonus spielt. Aufgrund dieser und anderer hier besprochener Befunde kann die Magnesium-Prophylaxe und Intervention für die Verhinderung und Behandlung von KHK, plötzlichem Tod bei ischämischer Herzkrankheit, Hypertonie und akutem Myokardinfarkt, auβerordentlich nützlich sein.
Sommario
La cardiopatia ischemica comporta indici elevati di mortalità e morbilitä. Numerose sindromi, espressione di’una miocardiopatia ischemica; quali l’angina instabile, la morte cardiaca improvvisa da ischemia miocardica, l’infarto miocardico acuto e le aritmie ventricolari, sono state associate ad un impoverimento miocardico di magnesio e di potassio.
Gli ioni Mg++ sono essenziali per la regolazione del trasporto del Na+ e del K+ attraverso le membrane cellutari, ivi incluse quelle delle cellule cardiache e delle miocellule vascolari lisce. Il Mg++ attiva una pompa Na+ -K+ -ATPasi dipendente la quule a sua volta esercita un ruolo fondamentale nel regolare il trasporto Na+ -K+. Una riduzione del Mg+ + cellulare comporta una perdita di composti a base di fosfato note volmente importanti: Mg-A TP e creatinfosfato. Pertanto, in condizioni di deplezione del Mg++ cellulare (per es. ipossia, ischemia, anossia) la pompa Na+ -K+ e le riserve di fosfageni saranno compromesse, con la conseguente alterazione dei potenziali di membrana a riposo. Si è osservato che l’impoverimento cellulare di Mg+ + comporta una deplezione concomitante di K+ in molti tipi di cellule, fra cui quelle muscolari, cardiache e vascolari. Come conseguenza di questo fenomeno si sviluppano spesso delle aritmie cardiache. Un danno miocardico e vascolare determina alterazioni nel trasporto di elettroliti attraverso le membrane cellulari, ove viene incrementata la captazione di Na+ di Ca+ + e, immediatamente prima o concomitantemente, si ha una perdita di Mg+ + e di K+. Tali squilibri elettrolitici determinano spesso necrosi parcellari.
Si sono accumulait numerosi dati sperimentali a favore dell’importanza delle concentrazioni extracellulari di Mg + + nel controllo del tono arterioso e della pressione arteriosa tramite la regolazione dei punti di scambio Mg+ + -Ca+ + sulle membrane vascolari. Una riduzione delle concentrazioni extracellulari di Mg+ + può produrre ipertensione, spasmo vascolare coronarico e potenziamento dell’azione di sostanze vasocostrittrici, facili-tando un eccessivo ingresso di Ca+ +; contemporaneamente è ridotta la potenza di sostanze vasodilatatrici. Alterazioni dei livelli di Mg+ + nelle membrane vascolari determinano la formazione di membrane arteriose e arteriolari ‘leaky’ (a maggiore permeabilité), contribuendo pertanto alla riduzione del contenuto cellulare di K+ ed all’ingresso di Na+ e Ca+ +. Alterazioni, nei limiti fisiologici, delle concentrazioni extracellulari di K+ o di Na+, in presenza di un deficit di Mg++, possono esacerbare lo spasmo vascolare coronarico osservato con la riduzione dei livelli del solo Mg+ + extracellulare. Dal momento che sono necessari ioni Mg+ + liberi per conservare gli ioni Ca+ + (sia legati alla membrana plasmatica sia legati alla membrana del reticolo sarcoplasmatico tramite Ca+ + A TPasi), le concentrazioni di Mg+ + libero intracellulare sarebbero incrementate in condizioni che comportino una perdita cellulare di Mg+ +, esacerbando pertanto e contribuendo ad elevare la pressione arteriosa e l’incidenza di spasmo coronarico. Viene anche suggerito da un numero sempre crescente di dati sperimentali che il Mg+ + puà controllare una pompa Na+ -Ca+ + di essenziale importanza per mantenere il normale tono vascolare coronarico.
In sintesi i dati disponibili suggeriscono che il Mg + + svolge un ruolo critico nel mantenere una normale eccitabilitü cardiaca ed un normale tono vascolare coronarico. Sulla base di questi e di altri dati qui esaminati, la profilassi e la terapia con magnesio possono risultare estremamente utili nella prevenzione e nel trattamento della cardiopatia ischemica, della morte improvvisa da miocardiopatia ischemica, dell’ipertensione e dell’infarto miocardico acuto.
Resumen
Las cardiopatías coronarias (CC) tienen un elevado indice de morbimortalidad. Cierto numéro de cuadros de CC y de sindrome isquémico miocàrdico, tales como angor inestable, cardiopatía isquémica con muerte sübita, infarto agudo de miocardio y las arritmias ventriculares, se han asociado a pérdidas de potasio y magnesio miocárdicos.
Los iones Mg++ son esenciales para el transporte de Na+ y K+ a través de las membranas celulares, incluyendo las de las células musculares cardiacas y del müsculo liso. El Mg+ + activa una bomba Na+ -K+ -ATPasa que, asuvez, desempeña un papel fundamental en la regulación del transporte de Na+ y K+. La pérdida de Mg + + intracelular tiene como consecuencia la pérdida de fosfágenos críicamente importantes: el MgA TP y el fosfato de creatina. Por ello, en condiciones en las que el Mg++ es déficiente (p.ej., hipoxia, isquemia, anoxia), la bomba Na + -K+ y los depósitos de compuestos de fosfato se verán alterados, con las alteraciones consiguientes en el potential de la membrana en reposo. Se ha observado que en determinado número de células, entre otras las de los músculos cardiaco y vasculares, la pérdida de Mg + + intracelular se acompaña de una depletión concomitante de K+. Con frecuencia, las consecuencias de estos acontecimientos es la productión de arritmias cardiacas. Las lesiones miocárdicas y vasculares dan lugar a alteraciones del transporte electrolítico a través de las membranas celulares, de modo que la captación de Na+ y Ca++ aumentan y, justo antes de que esto ocurra, o simultáneamente con ello, se pierden Mg+ + y K+. Tales alteraciones electrolíticas tienen como consecuencia frecuente la aparición de focos necróticos.
Hay gran cantidad de datos que vienen a señalar la importancia de la concentración extracelular de Mg + + en el control del tono arterial y la tensión arterial mediante la regulatión de los puntos de intercambio Mg+ + -Ca++ de la membrana vascular. Una reducción de la concentración extracelular de Mg++ puede producir hipertensión, vasospasmo coronario y potenciación de los agentes vasoconstrictores, al posibilitar una mayor entrada de Ca+ +; concomitantemente, lapotencia de los vasodilatadores se ve reducida. Las alteraciones en el Mg+ + de las membranas vasculares da lugar a membranas arteriales y arteriolares ‘con fugas’, to que contribuye a la depletion celular de K+ y la mayor acumulación de Na+ y Ca + +. Las modificaciones más alla de limites fisiológicos de las concentracions extracelulares de K+ o Na+ en presencia de un déficit de Mg+ + pueden exacerbar el espasmo coronario que se observa cuando la reductión sólo afecta al Mg + + extracelular. Dado que los iones libres de Mg+ + son necesarios para conservar los de Ca+ + a concentracion estable (tanto el unido a la membrana plasmática, como a la del retículo sarcoplásmico, mediante las Ca+ + -ATPasas), el Mg+ + libre intracelular aumentaria en las situaciones que producen pérdida celular de Mg+ +, exacerbando y contribuyendo asi a la elevatión de la tensión arterial y al vasospasmo coronario. Se están reuniendo asimismo datos que sugieren que quizd el Mg + + controle una bomba de Na+-Ca+ + esencial para la conservación del tono vascular coronario normal.
En resumen, los datos de que se dispone sugieren que el Mg + + desempeña papeles fundamentales en la conservación de la excitabilidad cardiaca y tono coronario normales. Sobre la base de estos y otros hallazgos que se revisan a continuacíon, la profilaxis e intervención sobre el magnesio qui’a sea extraordinariamente util para la prevención y tratamiento de las CC, cardiopatía isquémica con muerte súbita, hipertensión e infarto agudo de miocardio.
Resumo
As doenças coronárias (DC) apresentam um alto índice de mortalidade e de morbidez. Uma série de DC s e de síndromes isquêmicas do miocardio, tais como a angina pectoris instável, as doenças cardiacas isquêmicas que conduzem à morte súbita, o enfarte agudo do miocárdio e as arritmias ventriculares, foram associadas a perdas de magnésio e de potàssio por parte do miocárdio.
Os íons de Mg+ + são essenciais para a regulação do transporte de Na+ e de K+ através da membrana das células, incluindo as que se encontram nas células dos músculos lisos vasculares e cardíacos. O Mg + + ativa a bomba Na+ -K+ -ATPase, que por sua vez desempenha um importante papel na regulação do transporte de Na + -K+. A perda de Mg+ + do interior das células resulta na perda de fosfatos críticamente importantes: o MgATP e o fosfato de creatinina. Assim sendo, as condições em que se verifica depleção de Mg+ + no interior das células (por exemplo, hipoxia, isquemia, anoxia) comprometem a bomba Na+-K+ e as provisoes de fosfagênio, conduzindo a alterações nos potenciais das membranas em descanso. Descobriu-se que uma depleção de Mg++ no interior das células resulta numa concomitante depleção de K+ numa série de células, incluindo as células dos músculos cardíacos e vasculares. Uma das consequências disso, muitas vezes, é a produção de arritmias cardíacas. Os danos ao miocárdio e vasculares conduzem a distúrbios no transporte de eletrólitos através da membrana das células, pelo qual a absorção de Na+ e de Ca+ + é acentuada, verificando-se também, logo antes ou simultâneamente, perdas de Mg+ + e de K+. Estes distúrbios eletrolíticos conduzem muitas vezes a focos necróticos.
J’ se acumulou evidência considerável indicativa de que a concentração de Mg+ + no exterior das células é importante no controle do tônus arterial e na pressão sanguínea, por meio da regulação dos locais de intercâmbio de Mg + + -Ca + + nas membranas vasculares. Uma redução na concentração de Mg ++ no exterior das células pode produzir hipertensão, espasmos dos vasos coronários e potencialização de agentes vasoconstritores, ao permitir a entrada excessiva de Ca+ +; simultâneamente, é reduzida a potência dos agentes vasodilatadores. As alterações na concentração de Mg+ + nas membranas vasculares resultam em membranas arteriais e arteriolares com ‘vazamentos’, contribuindo assim para a redução de K+ no interior das células e para um aumento de Na + e de Ca+ +. As alterações na concentração de K+ ou de Na+ no exterior das células, dentro dos limites fisiológicos, e diante de um déficit de Mg+ +, podem exacerbar os espasmos dos vasos coronários observados com redução apenas na concentração de Mg++ no exterior das células. Visto que os íons livres de Mg + + são necessários para a manutenção dos ions de Ca++ (tanto os ligados à membrana do plasma como os ligados à membrana da retícula sarcoplásmica, por meio das Ca+ + ATPases), o Mg+ + livre no interior das células aumentaria em condições que resultam em perdas celulares de Mg+ +, desse modo exacerbando e contribuindo para a elevação da pressão sanguínea e dos espasmos dos vasos coronários. Há também dados acumulados sugerindo que o Mg+ + pode controlar a bomba Na+-Ca+ +, que é essencial para a manutenção de um tônus vascular coronário normal.
De maneira global, os dados disponíveis sugerem que o Mg + + desempenha papéis críticos na manutenção da excitabilidade cardíaca normal e do tônus dos vasos coronários. Com base nestas e em outras descobertas aqui analisadas, a profilaxia e a intervenção com magnésio podem ser extremamente úteis na prevenção e no tratamento de DCs, doenças cardiacas isquêmicas conduzindo a morte súbita, hipertensão e enfarte agudo do miocárdio.
Similar content being viewed by others
References
Abraham, A.S.; Eylath, U.; Weinstein, M. and Czaczkes, E.: Serum magnesium levels in patients with acute myocardial infarction. New England Journal of Medicine 296: 862–863 (1977).
Abraham, A.S.; Shaocil, R.; Shiminovitz, S.; Eylath, U. and Weinslein, M.: Serum magnesium levels in acute medical and surgical conditions. Biochemical Medicine 24: 1–6 (1980).
Aikawa, J.K.: Magnesium: Its Biologic Significance (CRC Press, Boca Ratan 1981).
Akera, T.: Ku, D. and Brody, T.M.: Alterations of ion movements as a mechanism of drug-induced arrhythmias and inotropic responses; in Huxtable and Barbeau (Eds) Taurine, p. 121 (Raven Press, New York 1976).
Altura, B.M.: Magnesium withdrawal and rhythmic contractility of arterial vs venous smooth muscle: Differential effects of multivalent cations and EDTA. Artery 4: 512–517 (1978).
Altura, B.M.: Sudden-death ischemic heart disease and dietary magnesium intake: Is the target site coronary vascular smooth muscle? Medical Hypotheses 5: 843–849 (1979).
Altura, B.T.: Type-A behavior and coronary vasospasm: A possible role of hypomagnesemia. Medical Hypotheses 6: 753–758 (1980).
Altura, B.M.: Magnesium and regulation of contractility of vascular smooth muscle. Advances in Microcirculation 11: 77–113 (1982).
Altura, B.M. and Altura, B.T.: Influence of magnesium on drug-induced contractions and ion content in rabbit aorta. American Journal of Physiology 220: 938–944 (1971).
Altura, B.M. and Altura, B.T.: Magnesium and contraction of arterial smooth muscle. Microvascular Research 7: 145–155 (1974).
Altura, B.M. and Altura, B.T.: Magnesium withdrawal and contraction of arterial smooth muscle: Effects of EDTA, EGTA and divalent cations. Proceedings of the Society for Experimental Biology and Medicine 151: 752–755 (1976).
Altura, B.M. and Altura, B.T.: Extracellular magnesium and contraction of vascular smooth muscle; in Casteels et al. (Eds) Excitation-Contraction Coupling in Smooth Muscle, pp. 137–144 (Elsevier/North-Holland, Amsterdam 1977a).
Altura, B.M. and Altura, B.T.: Ouabain, membrane Na+, K+-AT-Pase and the extracellular action of magnesium ions in arterial smooth muscle. Artery 3: 72–83 (1977b).
Altura, B.M. and Altura, B.T.: Magnesium and vascular tone and reactivity. Blood Vessels 15: 5–16 (1978).
Altura, B.T. and Altura, B.M.: Withdrawal of magnesium causes vasospasm while elevated magnesium produces relaxation of tone in cerebral arteries. Neuroscience Letters 20: 323–327 (1980).
Altura, B.M. and Altura, B.T.: Magnesium ions and contraction of vascular smooth muscles: Relationship to some vascular diseases. Federation Proceedings 40: 2672–2679 (1981a).
Altura, B.M. and Altura, B.T.: Role of magnesium ions in contractility of blood vessels and skeletal muscle. Magnesium-Bulletin 3(la): 102–114 (1981b).
Altura, B.M. and Altura, B.T.: General anesthetics and magnesium ions as calcium antagonists on vascular smooth muscle: in Weiss (Ed.) New Perspectives on Calcium Antagonists, pp.131–145 (American Physiology Society, Washington DC 1981c).
Altura, B.M. and Altura, B.T.: Magnesium modulates calcium entry and contractility in vascular smooth muscle; in Ohnishi and Endo (Eds) The Mechanism of Gated Calcium Transport Across Biological Membranes, pp. 137–145 (Academic Press, New York 1981d).
Altura, B.M. and Altura, B.T. (Eds): Dietary Minerals and Cardiovascular Disease (Karger, Basel 1982a).
Altura, B.M. and Altura, B.T.: Mg, Na and K interactions and coronary heart diseases. Magnesium 1: 241–265 (1982b).
Altura, B.T. and Altura, B.M.: The role of magnesium in etiology of strokes and cerebrovasospasm. Magnesium 1: 277–291 (1982c).
Altura, B.M. and Altura, B.T. (Eds): Magnesium, Diabetes and Carbohydrate Metabolism (Karger, Basel 1983a).
Altura, B.M. and Altura, B.T.: Pharmacologic inhibition of cerebral vasospasm in ischemia, hallucinogen ingestion, and hypomagnesemia: Barbiturates, calcium antagonists, and magnesium. American Journal of Emergency Medicine 1: 180–190 (1983b).
Altura, B.M. and Altura, B.T.: Role of magnesium in hypertension and ischemic vascular disorders; in Stokely-Van Camp Annual Symposium — Food in Contemporary Society. Its Role in the Treatment and Recovery from Disease, pp.87–98 (University of Tennessee, Knoxville 1983c).
Altura, B.M. and Altura, B.T.: Influence of magnesium on vascular smooth muscle and serum biochemical parameters from diabetic and hypertensive rats. Magnesium 2: 253–266 (1983d).
Altura, B.M. and Altura, B.T.: Magnesium-calcium interaction and contraction of arterial smooth muscle in ischemic heart diseases, hypertension and vasospastic disorders; in Wester (Ed.) Electrolytes and the Heart, pp. 41–56 (Trans Medica Inc., New York 1983e).
Altura, B.M. and Altura, B.T.: Microcirculatory actions and uses of naturally-occurring (magnesium) and novel synthetic calcium channel blockers. Microcirculation, Endothelium and Lymphatics 1: 185–220(1984).
Altura, B.M.; Altura, B.T. and Carella, A.: Magnesium deficiency-induced spasms of umbilical vessels: Relation to preeclampsia, hypertension, growth retardation. Science 221: 376–378 (1983).
Altura, B.M.; Altura, B.T.; Carella, A. and Turlapaty, P.D.M.V.: Hypomagnesemia and vasoconstriction: Possible relationship to etiology of sudden-death ischemic heart disease and hypertensive vascular diseases. Artery 9: 212–231 (1981).
Altura, B.M.; Altura, B.T.; Carella, A. and Turlapaty, P.D.M.V.: Ca2+ coupling in vascular smooth muscle: Mg2+ and buffer effects on contractility and membrane Ca2+ movements. Canadian Journal of Physiology and Pharmacology 60: 459–482 (1982).
Altura, B.M.; Altura, B.T.; Gebrewold, A.; Ising, H. and Günther, T.: Magnesium deficiency and hypertension: Correlation between magnesium-deficient diets and microcirculatory changes in situ. Science 223: 1315–1317 (1984).
Altura, B.M.; Halevy, S. and Turlapaty, P.D.M.V.: Vascular smooth muscle in diabetes mellitus and its influence on reactivity of blood vessels: in Davis (Ed.) The Microcirculation in Diabetes Mellitus, pp. 118–150 (Karger, Basel 1979).
Altura, B.M. and Ising. H. (Eds): Magnesium and Health. Artery 9: 166–252 (1981).
Altura, B.M. and Turlapaty, P.D.M.V.: Withdrawal of magnesium enhances coronary arterial spasms produced by vaso-active agents. British Journal of Pharmacology 77: 649–659 (1982).
Anderson, T.W.; Neri, L.C.; Shreiber, G.; Talbot, F. and Zdre-jewski, A.: Ischemic heart disease, water hardness, and myocardial magnesium. Canadian Medical Association Journal 113: 199–203 (1975).
Anonymous: Magnesium and cardiac function (Merck, Rahway 1983).
Askar, A.O. and Mustafa, S.J.: Role of magnesium in the relaxation of coronary arteries by adenosine. Magnesium 2: 17–25 (1983).
Behr, G. and Burton, P.: Heart-muscle magnesium. Lancet 2: 450 (1973).
Bersohn, I.: Atherosclerosis and coronary heart disease — possible incrimination of magnesium deficiency in their promotion. Medical Proceedings of South Africa 4: 62–66 (1958).
Bersohn, I. and Oelofse, P.J.: Correlation of serum magnesium and serum cholesterol levels in South African Bantu and European subjects. Lancet 1: 1020–1021 (1957).
Bigg, R.P.C. and Chia, R.: Magnesium deficiency. Role in arrhythmias complicating acute myocardial infarction? Medical Journal of Australia 1: 346–348 (1981).
Binet, A. and Volfin, P.: Regulation by Mg2+ and Ca2+ of milochondrial membrane integrity. Archives of Biochemistry 170: 576–586(1975).
Blaustein, M.P.: Sodium ions, calcium ions, blood pressure regulation and hypertension: A reassessment and a hypothesis. American Journal of Physiology 232: C165–C173 (1977).
Brierley, G.P.: Ion transport by heart mitochondria. Journal of Biological Chemistry 242: 1115–1122 (1967).
Buckberg, G.: Intraoperative myocardial protection: Current status; in Brautbar (Ed.) Myocardial and Cellular Bioenergetics and Compartmentation (Plenum, New York; in press, 1984).
Bunce, G.E.; Chiemchaisri, Y. and Phillips, P.H.: The mineral requirements of the dog. Journal of Nutrition 76: 23–29 (1962).
Burch, G.E. and Giles, T.D.: The importance of magnesium deficiency in cardiovascular disease. American Heart Journal 94: 649–657 (1977).
Burton, R.F.: Adenosine triphosphate as a determinant of magnesium levels in cytoplasm. Comparative Biochemistry and Physiology 65A: 1–4 (1980).
Carrier Jr, O.; Hester, R.K.; Jurevics, H.A. and Tenner Jr, T.E.: Influence of magnesium on calcium- and potassium-related responses in vascular smooth muscle. Blood Vessels 13: 321–337 (1976).
Chadda, K.D.; Gupta, P.K. and Lichtenstein, E.: Magnesium in cardiac arrhythmia. New England Journal of Medicine 287: 1102(1972).
Chadda, K.D. and Schultz, N.A.: Magnesium deficiency and coronary vasospasm: Role in sudden cardiac death. Magnesium 1: 84–94(1982).
Chance, B. and Williams, G.R.: The respiratory chain and oxidative phosphorylation. Advances in Enzymology 17: 65–134 (1956).
Chernow, B.; Smith, J.; Rainey, T.G. and Finton, C: Hypomagnesemia: Implications for the critical care specialist. Critical Care Medicine 10: 193–196 (1982).
Chipperfield, B. and Chipperfield, J.R.: Heart-muscle magnesium, potassium, and zinc concentrations after sudden death from heart disease. Lancet 2: 293–295 (1973).
Chipperfield, B. and Chipperfield, J.R.: Differences in metal content of the heart muscle in death from ischemic heart disease. American Heart Journal 95: 732–737 (1978).
Cohen, L. and Kitzes, R.: Magnesium sulfate in the treatment of variant angina. Magnesium 3: 46–49 (1984).
Cohen, S.M. and Burt, CT.: 31P nuclear magnetic relaxation studies of phosphocreatine in intact muscle: Determination of intracellular free magnesium. Proceedings of the National Academy of Sciences 74: 4271–4275 (1977).
Crawford, T. and Crawford, M.D.: Prevalence and pathological changes of ischaemic heart-disease in a hard-water and in a soft water area. Lancet 1: 229–232 (1967).
Crawford, M.D.; Gardner, M.J. and Morris, J.N.: Mortality and hardness of local water supplies. Lancet 1: 827–831 (1968).
Dahl, L.K.; Leith, G. and Heine, M.: Influence of dietary potassium and sodium/potassium molar ratios on the development of salt hypertension. Journal of Experimental Medicine 136: 318–330 (1972).
Dawson, E.B.; Frey, M.J.; Moore, T.D. and McGanity, W.J.: Relationship of metal metabolism to vascular disease mortality rates in Texas. American Journal of Clinical Nutrition 31: 1188–1197 (1978).
DiGiorgio, J.; Vitale, J.J. and Hellerstein, E.E.: Sarcosomes and magnesium deficiency in ducks. Biochemical Journal 82: 184–187 (1962).
Durlach, J. and Durlach, V.: Hormonal controls of magnesium homeostasis. Magnesium (In press, 1984).
Durlach, J. and Rayssiguier, Y.: Recent advances on the relationships between magnesium and carbohydrate metabolism. I. Physiological data. Magnesium 2: 174–191 (1983a).
Durlach, J. and Rayssiguier, Y.: Recent advances on the relationships between magnesium and carbohydrate metabolism. II. Clinical and therapeutic data. Magnesium 2: 192–224 (1983b).
Dyckner, T.: Serum magnesium in acute myocardial infarction. Acta Medica Scandinavica 207: 59–66 (1980).
Dyckner, T.; Wester, P.O.: Ventricular extrasystoles and intracellular electrolytes before and after potassium and magnesium infusions in patients on diuretic treatment. American Heart Journal 97: 12–18(1979).
Dyckner, T. and Wester, P.O.: Relation between potassium, magnesium and cardiac arrhythmias. Acta Medica Scandinavica 647(Suppl.): 163–169 (1981a).
Dyckner, T. and Wester, P.O.: Effects of magnesium infusions in diuretic induced hyponatremia. Lancet 1: 585–586 (1981b).
Dyckner, T. and Wester, P.O.: Effect of magnesium on blood pressure. British Medical Journal 286: 1847–1849 (1983).
Ebel, H. and Günther, T.: Role of magnesium in cardiac disease. Journal of Clinical Chemistry and Clinical Biochemistry 21: 249–265 (1983).
Edwards, G.S.; Lane, M. and Smith, F.E.: Long-term treatment with cis-dichloradiamine-platinum (II(-vinblastine-bleomycin: Possible association with severe coronary artery disease. Cancer Treatment Reports 63: 551–552 (1979).
Elin, R.J.; Armstrong, W.D. and Singer, L.: Body fluid electrolyte composition of chronically magnesium-deficient and control rats. American Journal of Physiology 220: 543–548 (1971).
Flatman, P. and Lew, V.L.: Use of ionophore A23187 to measure and to control free and bound cytoplasmic Mg in intact red cells. Nature 267: 360–362 (1977).
Fleckenstein, A.: Calcium Antagonism in Heart and Smooth Muscle (Wiley Interscience, New York 1983).
Fleckenstein, A.; Grün, G.; Byon, Y.K.; Doring, H.J. and Tritthart, H.: The basic Ca-antagonistic actions of nifedipine on cardiac energy metabolism and vascular smooth muscle tone; in Hashimoto et al. (Eds) New Therapy of Ischemic Heart Disease, pp. 31–44 (University of Tokyo Press, Tokyo 1975).
Folkow, B.: Physiological aspects of primary hypertension. Physiological Reviews 62: 347–504 (1982).
Freis, E.D.: Salt, volume and the prevention of hypertension. Circulation 53: 589–595 (1976).
Friedman, S.: Sodium ions and regulation of vascular tone, in Altura (Ed.) Ionic Regulation of the Microcirculation. Advances in Microcirculation Vol. 11 (Karger, Basel 1982).
Fujiwara, M.; Kitagawa, H. and Kurahashi, K.: Effects of magnesium on contractile responses induced by electrical transmural stimulation and noradrenaline in rabbit thoracic aorta. British Journal of Pharmacolgoy 63: 51–56 (1978).
George, G.A. and Heaton, F.W.: Changes in cellular composition during magnesium deficiency. Biochemical Journal 152: 609–615 (1975).
Ghani, M.G. and Smith, D.R.: The effectiveness of magnesium chloride in the treatment of ventricular tachyarrhythmias due to digitalis. American Heart Journal 88: 621–626 (1974).
Goldstein, S. and Zsotér, T.T.: The effect of magnesium on the response of smooth muscle to 5-hydroxytryptamine. British Journal of Pharmacology 62: 507–514 (1978).
Gueux, E. and Rayssiguier, Y.: The hypocholesterolaemic effect of magnesium deficiency following cholesterol feeding in the rat. Magnesium-Bulletin 2: 126–129 (1981).
Günther, T.: Wasser und Elektrolytverteilung in einigen Organen von Mg-arm ernährten Ratten. Zietschrift fuer Klinische Chemie und Klinische Biochemie 8: 65–68 (1970).
Günther, T.: Distribution and functions of magnesium; in Wester (Ed.) Electrolytes and the Heart, pp. 15–23 (TransMedica Inc., New York 1983).
Günther, T. and Dorn, F.: Die intrazellulaire Mg-Ioenaktivitat in verscheidenn Süugetierzellen. Zeitschrift fuer Naturforschung 26b: 176–177 (1971).
Gupta, R.K.; Benovic, T.L. and Rose, Z.B.: The determination of free magnesium level in the human red blood cell by 31P NMR. Journal of Biological Chemistry 254: 6172–6176 (1978).
Gupta, R.K. and Moore, R.D.: 31P NMR studies of intracellular free Mg2+ in intact frog skeletal muscle. Journal of Biological Chemistry 225: 3987–3993 (1980).
Haddy, F.J.: The role of potassium ions in regulating vascular resistance; in Altura (Ed.) Ionicregulation of the Microcirculation. Advances in Microcirculation Vol. 11 (Karger, Basel 1982).
Haddy, F.J. and Seelig, M.S.: Magnesium and the arteries. II. Physiologic effects of electrolyte abnormalities on arterial resistance; in Cantin and Seelig (Eds) Magnesium in Health and Disease, pp. 639–657 (Spectrum Publications, Holliswood 1980).
Hearse, D.J.; Stewart, D.A. and Braimbridge, M.V.: Myocardial protection during ischemic cardiac arrest. Journal of Thoracic and Cardiovascular Surgery 75: 877–885 (1978).
Heggtveit, H.A.; Tanser, P. and Hunt, B.: Magnesium content of normal and ischemic hearts. Proceedings of the 7th International Congress of Clinical Pathology, Montreal, p.53 (1969).
Hess, P. and Weingart, R.: Free magnesium in cardiac and skeletal muscle measured with ion-selective micro-electrodes. Journal of Physiology (London) 318: 14P–15P (1981).
Hochrein, H.; Kuschke, H.J.; Zagga, Q. and Fahl, F.: Das Verhalten der intracellularen Magnesium-Konzentration im Myokard bei Insuffizienz, Hypoxie und Kammerflimmern. Klinische Wochenschrift 45: 1093–1096 (1967).
Holden, M.P.; Ionescu, M.I. and Wooler, G.H.: Magnesium in patients undergoing open-heart surgery. Thorax 27: 212–218 (1972).
Hollifield, J.W.; Slaton Jr, P.E. and Moore, L.C.: Thiazide diuretics, hypokalemia, and cardiac arrhythmias; in Wester (Ed.) Electrolytes and the Heart, pp. 111–119 (TransMedica Inc., New York 1983).
Holtmeier, H.J.: Magnesiumstoffwechselstörungen und Herzinfarkt; in Heilmeyer and Holtmeier (Eds) Herzinfarkt und Schock, P.110 (Thieme, Stuttgart 1969).
Huddart, H. and Latham, H.: Calcium regulation in smooth muscle. II. Interaction of sodium and magnesium in calcium counterexchange. General Pharmacology 12: 161–168 (1981).
Huddart, H. and Saad, K.H.M.: The effect of sodium and magnesium and their interaction with quinine and lanthanum on spontaneous activity and related calcium movements of rat ileal smooth muscle. Journal of Comparative Physiology 126: 233–240(1978).
Hungerford, G.F. and Bernick, S.: Response of rat coronary arteries to dietary magnesium deficiency with and without cholesterolemia; in Cantin and Seelig (Eds) Magnesium in Health Disease, pp. 659–670 (Spectrum Publication, Holliswood 1980).
Imura, O.; Kijima, T.; Kituchi, K. et al.: Studies on the hypotensive effect of high potassium intake in patients with essential hypertension. Clinical Science 61: 77S–80S (1981).
Iseri, L.T.; Alexander, L.C.; MacCaughey, R.S.; Boyle, A.J. and Meyers, G.: Water and electrolyte content of cardiac and skeletal muscle in heart failure and myocardial infarction. American Heart Journal 43: 215–227 (1952).
Jennings, R.B.; Sommers, H.M.; Kaltenbach, J.P. and West, J.J.: Electrolyte alterations in acute myocardial ischaemic injury. Circulation Research 14: 260–269 (1964).
Johnson, C.J.; Peterson, D.R. and Smith, E.K.: Myocardial tissue concentrations of magnesium and potassium in men dying suddenly from ischemic heart disease. American Journal of Clinical Nutrition 32: 967–970 (1979).
Juan, D.J.: Clinical review: The clinical importance of hypomagnesemia. Surgery 91: 510–517 (1982).
Kakkar, B. and Mullick, D.N.: Effect of intramuscular injection of magnesium sulphate solution on the growth rate and serum composition in rats. Annals of Biochemical and Experimental Medicine 23: 299–330 (1963).
Karppanen, H.; Pennanen, R. and Passinen, L.: Minerals, coronary heart disease and sudden coronary death. Advances in Cardiology 25: 9–24(1978).
Khaw, K.T. and Thorn, S.: Randomised double-blind cross-over trial of potassium on blood pressure in normal subjects. Lancet 2: 1127–1129(1982).
Kobayashi, J.: Geographical relation between the chemical nature of river water and death-rate from apoplexy. Ber. Ohara lnst. Landw. Biol. II: 12–21 (1957).
Leary, W.P. and Reyes, A.J.: Magnesium and sudden death. South African Medical Journal 64: 697–698 (1983).
Leary, W.P.; Reyes, A.J.; Lockett, C.J.; Arbuckle, D.D. and Van Der Byl, K.: Magnesium and deaths ascribed to ischaemic heart disease in South Africa. A preliminary report. South African Medical Journal 64: 775–776 (1983).
Lehr, D.: Magnesium and cardiac necrosis. Magnesium-Bulletin 3: 178–191 (1981).
Lehr, D.; Blaiklock, R. and Brown, A.: Magnesium loss as a reliable measure of acute myocardial injury; in Cantin and Seelig (Eds) Magnesium in Health and Disease, pp.499–506 (Spectrum Publications, Holliswood 1980).
Lim, P.; Jacob, E.; Dong, S. and Khoo, O.T.: Values for tissue magnesium as a guide in detecting magnesium deficiency. Journal of Clinical Pathology 22: 417–421 (1969).
McCarron, D.A.; Filer, L.J. and Van Itallie, T.V. (Eds): Current Prospectives in Hypertension. A Symposium on Food, Nutrition, and Health. Hypertension 4 (Part II): 1–183 (1982).
MacGregor, G.A.: Dietary sodium and potassium intake and blood pressure. Lancet I: 750–753 (1983).
MacGregor, G.A.; Smith, S.J.; Markanda, N.D.; Banks, R.A. and Sagnella, G.A.: Moderate potassium supplementation in essential hypertension. Lancet 2: 567–570 (1982).
MacIntyre, I. and Davidson, D.: The production of secondary potassium depletion, sodium retention, nephrocalcinosis and hypercalcaemia by magnesium deficiency. Biochemical Journal 70: 456–462(1958).
Madden, J.A.; Smith, G.A. and Llaurado, J.G.: Myocardial K kinetics in rats on Mg-deficient diet. Journal of the American College of Nutrition 1: 323–329 (1982).
Marier, J.R.: Quantitative factors regarding magnesium status in the modern-day world. Magnesium 1: 3–15 (1982).
Marier, J.R.; Neri, U.C. and Anderson, T.W.: Water hardness, human health, and the importance of magnesium. National Research Council of Canada Publication No. 17581, pp. 1-119 (1979).
Martindale, L. and Heaton, F.W.: Magnesium deficiency in the adult rat. Biochemical Journal 92: 119–126 (1964).
Masironi, R.; Pisa, Z. and Clayton, D.: Myocardial infarction and water hardness in European towns. Journal of Environmental Pathology and Toxicology 4: 77–87 (1980).
Meneely, G.R. and Battarbee, H.D.: High sodium-low potassium environment and hypertension. American Journal of Cardiology 38: 768–785(1976).
Montgomery, R.D.: Mangesium balance studies in marasmic kwashiorkor. Journal of Pediatrics 59: 119–123 (1961).
Morgan, T.; Adam, W.; Gilles, A.; Wilson, M.; Morgan, G. and Garney, S.: Hypertension treated by salt restriction. Lancet 1: 227–280(1978).
Mountokalakis, T.D.: Diuretic-induced magnesium deficiency. Magnesium 2: 57–62 (1983).
Nakamura, M.; Ishiwara, Y.; Sata, T. and Toru, S.: Effects of dietary magnesium and glycerrhizine on experimental atheromatosis of rats (long-term experiment). Japanese Heart Journal 7: 474–486 (1966).
Nath, K.; Sikka, K.K.; Sur, B.K.; Saxena, C.P. and Srivastava, S.: Serum magnesium in clinical and experimental myocardial infarction. Indian Journal of Medical Research 57: 317–323 (1969).
Page, E. and Polimeni, R.I.: Magnesium exchange in rat ventricle. Journal of Physiology (London) 224: 121–139 (1972).
Palaty, V.: Distribution of magnesium in the arterial wall. Journal of Physiology (London) 218: 353–368 (1971).
Palaty, V.: Regulation of the cell magnesium in vascular smooth muscle. Journal of Physiology (London) 242: 555–569 (1974).
Papper, S.: Sodium: Its Biologic Significance (CRC Press, Boca Ratan 1982).
Popescu, L.M.: Cytochemical study of the intracellular calcium distribution in smooth muscle. Surface microvesicles and cellular calcium homeostasis; in Casteels et al. (Eds) Excitation-Contraction Coupling in Smooth Muscle, pp. 13–23 (Elsevier/ North-Holland, Amsterdam 1977).
Post, R.L.; Merritt, C.R.; Kinsolving, C.R. and Albright, CD.: Membrane adenosine triphosphatase as a participant in the active transport of sodium and potassium in the human erythrocyte. Journal of Biological Chemistry 235: 1796–1803 (1960).
Rayssiguier, Y.: Magnesium and lipids in interrelationships in the pathogenesis of vascular diseases. Magnesium-Bulletin 3(1a): 165–177 (1981).
Rouse, I.L.; Beillin, L.J.; Armstrong, B.K. and Vandongen, R.: Blood-pressure-lowering effect of a vegetarian diet: Controlled trial in normotensive subjects. Lancet 1: 5–10 (1983).
Rouslin, W.: Impairment of mitochondrial oxidative phosphorylation during extreme Ca2+ overloading: The role of the mitochondrial Pase: in Brautbar (Ed.) Myocardial and Cellular Bioenergetics and Compartmentation (Plenum Press, New York; in press, 1984).
Ryan, M.P.; Whang, R. and Yamalis, W.: Effect of magnesium deficiency on cardiac and skeletal muscle potassium during dietary potassium restriction. Proceedings of the Society for Experimental Biology and Medicine 143: 1045–1047 (1973).
St Cyr, J.A.; Ward, H.B.; Kriett, J.M.; Alyono, D.; Einzig, S.; Bianco, R.W.; Anderson, R.W. and Foker, J.E.: Enhanced recovery of myocardial ATP levels following global ischemia; in Brautbar (Ed.) Myocardial and Cellular Bioenergetics and Compartmentation (Plenum Press, New York; in press, 1984).
Seelig, J.M.; Wei, E.P.; Kontos, H.A.; Choi, S.C. and Becker, D.P.: Effect of changes in magnesium ion concentration on cat cerebral arteries. American Journal of Physiology 245: H22–H26 (1983).
Seelig, M.S.: Myocardial loss of functional magnesium. I. Effect on mitochondrial integrity and potassium retention; in Bajusz and Rona (Eds) Myocardiology, pp. 615–625 (University Park Press, Baltimore 1972).
Seelig, M.S.: Magnesium Deficiency in the Pathogenesis of Disease (Plenum Press, New York 1980).
Seelig, M.S. and Heggtveit, H.A.: Magnesium interrelationships in ischemic heart disease: A review. American Journal of Clinical Nutrition 27: 59–79 (1974).
Seller, R.H.; Canziano, J.; Kimm, E.; Mendelssohn, S.; Brest, A.N. and Swartz, CD.: Digitalis toxicity and hypomagnesemia. American Heart Journal 79: 57–68 (1970).
Sheehan, J. and White, A.: Diuretic-associated hypomagnesemia. British Medical Journal 285: 1157–1159 (1982).
Shils, M.E.: Experimental human magnesium depletion. Medicine (Baltimore) 48: 61–82 (1969).
Shine, K.I.: Myocardial effects of magnesium. American Journal of Physiology 237: H413–H423 (1979).
Simpson, F.O.: Salt and hypertension: A sceptical review of the evidence. Clinical Science 57: 463S–480S (1979).
Skou, J.C.: Enzymatic basis for active transport of Na+ and K+ across cell membrane. Physiological Reviews 45: 596–617 (1965).
Somlyo, A.P. and Somlyo, A.V.: Effects and subcellular distribution of magnesium in smooth and striated muscles. Federation Proceedings 40: 2667–2671 (1981).
Specter, M.J.; Schweizer, E. and Goldman, R.H.: Studies on magnesium’s mechanism of action in digitalis-induced arrhythmias. Circulation 52: 1001–1005 (1975).
Speich, M.; Bousquet, B. and Nicolas, G.: Concentrations of magnesium, calcium, potassium, and sodium in human heart muscle after acute myocardial infarction. Clinical Chemistry 26: 1662–1665 (1980).
Storstein, O.; Hansteen, V.; Hatle, L.; Hillestad, L. and Storstein, L.: Studies on digitalis. XIV. Is there any correlation between hypomagnesemia and digitalis intoxication? Acta Medica Scandinavica 202: 445–447 (1977).
Szekely, P. and Wynne, N.A.: The effect of magnesium on cardiac arrhythmias caused by digitalis Clinical Science 10: 241–253 (1951).
Szelényi, I.: Magnesium and its significance in cardiovascular and gastrointestinal disorders. World Review of Nutrition and Dietetics, Vol. 17, pp. 189–224 (Karger, Basel 1973).
Turlapaty, P.D.M.V. and Altura, B.M.: Extracellular magnesium ions control calcium exchange and content of vascular smooth muscle. European Journal of Pharmacology 52: 421–423 (1978).
Turlapaty, P.D.M.V. and Altura, B.M.: Magnesium deficiency produces spasms of coronary arteries: Relationship to etiology of sudden death ischemic heart disease. Science 208: 198–200 (1980a).
Turlapaty, P.D.M.V. and Altura, B.M.: Magnesium ions and contractions of alloxan-diabetic vascular muscle. Artery 6: 375–384 (1980b).
Turlapaty, P.D.M.V. and Altura, B.M.: Influence of magnesium on adrenergic amine-induced responses of canine coronary arterial smooth muscle. Magnesiun 1: 57–68 (1982a).
Turlapaty, P.D.M.V. and Altura, B.M.: Effects of neurohypophyseal peptide hormones on isolated coronary arteries: Role of magnesium ions. Magnesium 1: 122–128 (1982b).
Turlapaty, P.D.M.V.; Weiner, R.; Altura, B.M.: Interactions of magnesium and verapamil on tone and contractility of vascular smooth muscle. European Journal of Pharmacology 74: 263–272(1981).
Van Breeman, C; Aaronson, P. and Loutzenhiser, R.: Sodium-calcium interactions in mammalian smooth muscle. Pharmacological Reviews 30: 167–208 (1978).
Velaso, D.; Guynn, R.W.; Oskarsson, M. and Veech, R.L.: The concentration of free and bound magnesium in rat tissues. Journal of Biological Chemistry 248: 4811–4819 (1973).
Vitale, J.J.; Hegsted, D.M.; Nakamura, M. and Connors, P.: The effect of thyroxine on magnesium requirement. Journal of Biological Chemistry 226: 597–601 (1957).
Vogelzang, N.J.; Bosl, G.J.; Johnson, K. and Kennedy, B.J.: Raynaud’s phenomenon: A common toxicity after combination chemotherapy for testicular cancer. Annals of Internal Medicine 95: 288–292 (1981).
Wacker, W.E.C.: Magnesium and Man (Harvard University Press, Cambridge 1980).
Walker, G.M. and Duffus, J.H.: Magnesium as the fundamental regulator of the cell cycle. Magnesium 2: 1–16 (1983).
Walker, W.G.; Whelton, P.K.; Saito, H.; Patterson, R.R. and Hermann, J.: Relation between blood pressure and renin, renin substrate, angiotensin II, aldosterone and urinary sodium and potassium in 575 ambulatory subjects. Hypertension 1: 287–291 (1979).
Webb, R.C. and Bohr, D.E.: Recent advances in the pathogenesis of hypertension: Consideration of structural, functional, and metabolic vascular abnormalities resulting in elevated arterial resistance. American Heart Journal 102: 251–264 (1981).
Wehrle, J.P.; Jurkowitz, M.; Scott, K.M. and Brierley, G.: Mg2+ and the permeability of heart mitochondria to monovalent cations. Archives of Biochemistry 174: 312–323 (1976).
Welt, L.G.: Experimental magnesium depletion. Yale Journal of Biology and Medicine 36: 325–349 (1964).
Whang, R. and Aikawa, J.K.: Magnesium deficiency and refractoriness to potassium depletion. Journal of Chronic Diseases 30: 65–68 (1977).
Whang, R.; Chrysant, S.; Dillard, B.; Smith, W. and Fryer, A.: Hypomagnesemia and hypokalemia in 1,000 treated ambulatory hypertensive patients. Journal of the American College of Nutrition 1: 317–322 (1982).
Whang, R.; Morosi, H.J.; Rodgers, D. and Reyes, R.: The influence of sustained magnesium deficiency on muscle potassium repletion. Journal of Laboratory and Clinical Medicine 70: 895–902 (1967).
Whang, R. and Welt, L.G.: Observations in experimental magnesium depletion. Journal of Clinical Investigation 43: 305–313(1963).
Whelton, P.K.: Thiazide-induced hypokalemia — an epidemiologic prospective; in Wester (Ed.) Electrolytes and the Heart, pp. 77–81 (TransMedica Inc., New York, 1983).
White, B.C.; Winegar, CD.; Wilson, R.F. and Kirause, G.S.: Calcium blockers in cerebral resuscitation. Journal of Trauma 23: 788–794(1983).
Wills, M.R.: Incidence of hypokalemia and hypomagnesemia related to diuretic usage; in Wester (Ed.) Electrolytes and the Heart, pp. 62–76 (TransMedica Inc., New York 1983).
Winkler, A.W.; Smith, P.K. and Hoff, H.E.: Intravenous magnesium sulfate in the treatment of nephritic convulsions in adults. Journal of Clinical Investigation 21: 207–216 (1942).
Wu, S.T.; Pieper, G.M.; Salhany, J.M. and Eliot, R.S.: Measurement of free magnesium in perfused and ischemic-arrested heart muscle. A quantitative phosphorus-31 nuclear magnetic resonance and multiequilibria analysis. Biochemistry 20: 7399–7403 (1981).
Yeager, J.C. and Masters, T.N.: Thermographic evidence that an ergonovine-induced coronary artery spasm can be produced in the dog by acutely lowering plasma Mg. Magnesium 1: 95–103(1982).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Altura, B.M., Altura, B.T. Magnesium, Electrolyte Transport and Coronary Vascular Tone. Drugs 28 (Suppl 1), 120–142 (1984). https://doi.org/10.2165/00003495-198400281-00013
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-198400281-00013