Abstract
Background: It is widely quoted that women with epilepsy have a higher than baseline risk for giving birth to a child with malformations, independent of the effects of antiepileptic drugs.
Objective: To determine, based on available evidence, if epilepsy per se represents a teratogenic risk. To systematically review all studies investigating the occurrence of major malformation rates among children of treated or untreated women with epilepsy and non-exposed controls who do not have epilepsy.
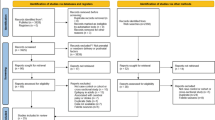
Methods: A meta-analysis, using a random effects model, was conducted of all cohort and case-control studies reporting malformation rates in children of women with epilepsy exposed or unexposed to antiepileptic drugs compared with that of children of nonepileptic women. Medline (1966–2001), EMBASE, the Cochrane database as well as REPROTOX (an information system on environmental hazards to human reproduction and development) databases were accessed.
Results: We found ten studies reporting results of untreated epilepsy (n = 400) and their non-epileptic healthy controls (n = 2492). Nine out of ten studies also reported results on 1443 patients exposed to antiepileptic drugs and their 2526 unexposed healthy controls. The risk for congenital malformations in the offspring of women with untreated epilepsy was not higher than among nonepileptic controls (odds ratio [OR] = 1.92; 95% CI 0.92–4.00). There was evidence of publication bias, thus with bias removed the OR was 0.99 (95% CI 0.49–2.01). In contrast, the offspring of epileptic women who received antiepileptic drugs had higher incidences of malformation than controls (OR 3.26; 95% CI 2.15–4.93).
Conclusion: Our study does not support the commonly held view that epilepsy per se represents a teratogenic risk. Our study suggests that this view is the result of a publication bias, with several small (<100 participants) positive studies leading to a premature conclusion.




Similar content being viewed by others
References
Devinsky O, Yerby M. Women with epilepsy: reproduction and effects of pregnancy on epilepsy. Neurol Clin 1994; 12: 479–95
Yerby MS. Pregnancy and epilepsy. Epilepsia 1991; 32Suppl. 6: s51–9
Martin PJ, Millac PAH. Pregnancy, epilepsy, management and outcome: a 10-year perspective. Seizure 1993; 2: 277–80
Janz D. On major malformations and minor anomalies in the offspring of parents with epilepsy: review of the literature. In: Janz D, Dam M, Richens A, et al., editors. Epilepsy, pregnancy, and the child. New York: Raven Press, 1982: 211–22
Majewski F, Steger M, Richter B, et al. The teratogenicity of hydantoins and barbiturates in humans, with considerations on the etiology of malformations and cerebral disturbances in the children of epileptic parents. Int J Biol Res Pregnancy 1981; 2(1): 37–45
Dansky LV, Finnell RH. Parental epilepsy, anticonvulsant drugs, and reproductive outcome: epidemiologic and experimental findings spanning three decades. 2: human studies. Reprod Toxicol 1991; 5(4): 301–35
Nulman I, Laslo D, Koren G. Treatment of epilepsy in pregnancy. Drugs 1999; 57(4): 535–44
Jones KL, Lacro RV, Johnson K, et al. Patterns of malformations in the children of women treated with carbamazepine during pregnancy. N Engl J Med 1989; 320: 1661–6
Clayton-Smith J, Donnai D. Fetal valproate syndrome. J Med Genet 1995; 32: 724–7
Nulman I, Scolnik D, Chitayat D, et al. Findings in children exposed in utero to phenytoin and carbamazepine monotherapy: independent effects of epilepsy medications. Am J Med Genet 1997; 68: 18–24
Koch S, Gopfert-Geyer I, Jager-Roman E, et al. Antiepileptika wahrend der schwangerschaft. Dtsch Med Wochenschr 1983; 108: 250–7
International League Against Epilepsy, Commission on Classification and Terminology of the International League Against Epilepsy. Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia 1990; 30: 389–99
Holmes LB, Harvey EA, Coull BA, et al. The teratogenicity of anticonvulsant drugs. N Engl J Med 2001; 344: 1132–8
Spiedel BD, Meadow SR. Maternal epilepsy and abnormalities of the fetus and newborn. Lancet 1972; 21: 839–43
Jick SS, Terris BZ. Anticonvulsants and congenital malformations. Pharmacotherapy 1997; 17: 561–4
Holmes LB, Rosenberger PB, Harvey EA, et al. Intelligence and physical features of children of women with epilepsy. Teratology 2000; 61: 196–202
Koch S, Losche G, Jager-Roman E, et al. Major and minor birth malformations and antiepileptic drugs. Neurology 1992; 42Suppl. 5: 83–8
Fedrick J. Epilepsy and pregnancy: a report from the Oxford Record Linkage Study. BMJ 1973; 2: 442–8
Koch S, Hartmann A, Jager-Roman E, et al. Major malformations in children of epileptic parents: due to epilepsy or its therapy? In: Janz D, Dam M, Richens A, et al., editors. Epilepsy, pregnancy and the child. New York: Raven Press, 1982: 313-5
Van der Pol MC, Hadders-Algra M, Huisjes HJ, et al. Antiepileptic medication in pregnancy: late effects on the children’s central nervous system development. Am J Obstet Gynecol 1991; 164: 121–8
Fabris C, Licata D, Stasiowska B, et al. Il neonato da madre epilettica: rischio malformativo ed auxologico. Pediatr Med Chir 1989; 11: 27–32
Yerby M. Pregnancy, teratogenesis and epilepsy. Neurol Clin 1994; 12: 749–71
Kaneko S, Otani K, Fukushima J, et al. Teratogenicity of antiepileptic drugs: analysis of possible risk factors. Epilepsia 1988; 29: 459–67
Kaneko S, Fukushima Y, Sato T, et al. Teratogenicity of antiepileptic drugs: a prospective study. Jpn J Psychiatry Neurol 1986; 40: 447–50
Byrne B. Epilepsy and pregnancy. Ir Med J 1997; 90: 173–4
Lopes-Cendes I, Andermann E, Candes F, et al. Risk factors for changes in seizure frequency during pregnancy of epileptic women: a cohort study [abstract]. Epilepsia 1992; 33Suppl. 3: 57
Donaldson JO. Neurologic disorders of pregnancy. In: Reece EA, Hobbins JC, Mahoney MJ, et al., editors. Medicine of the fetus and mother. Philadelphia (PA): JB Lippincott, 1992: 1097–102
Acknowledgments
Supported in part by Novartis, Barcelona, Spain. Eran Koser was supported by a Fellowship from the Research Training Center, The Hospital for Sick Children, Toronto, Ontario, Canada and Dr Gideon Koren is a senior scientist of the Canadian Institute for Health Research. The authors have no conflicts of interest directly relevant to the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fried, S., Kozer, E., Nulman, I. et al. Malformation Rates in Children of Women with Untreated Epilepsy. Drug-Safety 27, 197–202 (2004). https://doi.org/10.2165/00002018-200427030-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200427030-00004