Summary
Abstract
Manidipine is a dihydropyridine calcium antagonist, which causes systemic vasodilation by inhibiting the voltage-dependent calcium inward currents in smooth muscle cells. The resulting reduction in blood pressure (BP) in patients with hypertension is maintained over 24 hours.
Manidipine 10 to 40mg once daily for 4 weeks significantly lowered office BP from baseline and compared with placebo, and significantly reduced 24-hour BP compared with placebo in patients with essential hypertension in a well controlled trial. The decline in BP was maintained over 24 hours (trough to peak BP ratios were >50%) without disturbing the circadian BP pattern. BP reductions with therapeutic dosages of manidipine were maintained for up to 1 year in noncomparative trials.
The BP-lowering capacity of manidipine 5 to 20 mg/day appears to be similar to that of other calcium antagonists with which it has been compared in randomised double-blind and nonblind trial.
In a well controlled short term trial, manidipine 10mg daily significantly decreased trough sitting BP compared with placebo in elderly patients with mild to moderate essential hypertension. Decreases in BP were maintained for up to 3 years of treatment.
The drug (10 or 20 mg/day) also significantly lowered sitting BP from baseline in patients with hypertension and type 2 diabetes mellitus in randomised, long term comparative trials. In general, the observed reduction in BP with manidipine was similar to that observed with amlodipine, enalapril or delapril. The effects of manidipine on urinary albumin excretion (UAE) have not been clearly demonstrated in clinical trials in this patient group. BP was also reduced with manidipine in patients with impaired glucose tolerance.
Manidipine was well tolerated in clinical trials, with most adverse effects related to vasodilation. Commonly reported events included ankle oedema, headache, palpitation, flushing, dizziness, rash and fatigue. Manidipine appears to have less potential for pedal oedema than amlodipine.
Conclusions: Manidipine has shown antihypertensive efficacy and appears to be well tolerated in adult and elderly patients with mild or moderate essential hypertension. The BP-lowering effects of the drug in patients with hypertension and type 2 diabetes mellitus or impaired glucose tolerance were not associated with any adverse metabolic effects. The effects of manidipine on UAE in this patient group remain unclear. Manidipine provides an additional treatment option for patients for whom dihydropyridine calcium antagonists are appropriate.
Pharmacodynamic Properties
Manidipine is a second generation dihydropyridine calcium antagonist, which inhibits the voltage-dependent calcium inward currents in smooth muscle cells. The subsequent peripheral vasodilation leads to a reduction in blood pressure (BP) in patients with hypertension, which is maintained over a 24-hour period.
The drug is vasoselective and has shown less in vitro negative inotropic activity than nisoldipine, nicardipine, nifedipine, verapamil and diltiazem. Heart rate (HR) did not significantly increase with manidipine 10 to 30mg once daily; however, increases in HR were observed with manidipine 40mg daily. Manidipine 10 or 20mg daily significantly reduced measures of left ventricular mass in patients with essential hypertension and hypertension in diabetes.
Results from experimental animal studies and trials in patients with essential hypertension indicate that manidipine produces vasodilation of the efferent as well as the afferent arterioles, and causes natriuresis and diuresis. Administration of manidipine was also associated with retardation of end-stage renal pathology in rats and a reduction in urinary albumin excretion (UAE) from baseline in patients with essential hypertension and normotensive patients with type 2 diabetes mellitus. However, consistent reductions in UAE have not been demonstrated in patients with type 2 diabetes mellitus and hypertension after manidipine.
The drug has been shown to decrease the incidence of or completely inhibit stroke in stroke-prone rat models. Clinical trials in patients with essential hypertension or patients with hypertension and type 2 diabetes mellitus indicate that manidipine (10 to 40 mg/day) has neutral effects on lipid profiles and glucose metabolism (including atherogenic index in one trial). Therapeutic dosages of the drug significantly improved insulin sensitivity in patients with hypertension in diabetes.
Pharmacokinetic Profile
The mean maximum plasma concentration (Cmax; 7.2 μg/L) of manidipine was reached 1.5 hours after oral administration of a single 20mg dose in 12 fasting healthy volunteers; the area under the plasma concentration-time curve extrapolated to infinity (AUC∞) was 20.8 μg/L Dh. The presence of food increases manidipine absorption (AUC∞ 29.1 μg/L Dh). Manidipine appears to undergo a high degree of plasma protein binding (99%).
After oral administration, manidipine undergoes extensive first-pass hepatic metabolism, with 63% of an oral dose eliminated in the faeces and 31% in the urine as metabolites. In healthy volunteers, the terminal elimination half-lives for a single oral dose of manidipine 5,10 and 20mg varied from 3.9 to 7.95 hours.
The pharmacokinetic profile of manidipine in patients with mild hepatic impairment appears to be similar to that observed in healthy volunteers, whereas elimination is significantly delayed in patients with more severe hepatic impairment. Therapeutic dosages of manidipine appear to have low potential for drug-drug interactions.
Therapeutic Efficacy
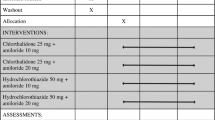
Manidipine 10 to 20 mg/day for 4 to 48 weeks reduced office SBP by 15 to 32mm Hg and DBP by 7 to 16mm Hg in randomised trials of adult patients with mild to moderate hypertension. Manidipine (10, 20 or 40mg once daily) significantly lowered office BP compared with baseline and placebo, and significantly lowered 24-hour BP compared with placebo after 4 weeks in adult patients with mild to moderate hypertension in a double-blind, randomised placebo-controlled trial. The decline in BP was maintained over 24 hours [trough to peak ratios ranged between 0.62 and 0.79 for systolic BP (SBP) and 0.54 to 0.67 for diastolic BP (DBP)] without disturbing the circadian BP pattern.
Manidipine 10 to 20mg once daily appears to have a similar BP-lowering capacity to that of other calcium antagonists with which it has been compared (once daily amlodipine 2.5 to 10mg, felodipine 5 or 10mg, lacidipine 4 or 6mg or nicardipine 10 or 20mg, or twice daily controlled release nifedipine (20 or 40mg). In contrast, in a randomised trial of 40 patients with mild to moderate essential hypertension, manidipine 10 to 40mg daily significantly reduced DBP compared with delapril 15 to 60mg daily at months 5, 6, 9 and 12.
Several long term, noncomparative studies in patients with mild to/or moderate hypertension suggest that BP reductions with recommended dosages of manidipine (10 or 20mg daily) are maintained for up to 1 year with no development of tolerance.
Special Patient Populations
Long term randomised, comparative trials indicate that manidipine 10 or 20mg once daily significantly lowers sitting BP from baseline in patients with hypertension and concomitant type 2 diabetes mellitus by 16 to 21mm Hg (SBP) and by 9 to 16mm Hg (DBP). The observed reduction in BP with manidipine was similar to that observed with other standard antihypertensive therapies (amlodipine, enalapril and delapril) in randomised multicentre trials.
Trough sitting SBP and DBP significantly decreased (by 16/7mm Hg) with manidipine 10mg once daily for 8 weeks compared with placebo in a study of 54 elderly patients (aged 76 to 89 years) with mild to moderate essential hypertension in a double-blind, randomised, placebo-controlled trial. In addition, BP normalised (DBP ≤ 90mm Hg) in more manidipine (63%) than placebo (4%) recipients. Decreases in BP from baseline were maintained for up to 3 years of treatment in a long term, nonrandomised, nonblind comparative trial in elderly patients.
BP was significantly reduced from baseline after 4 weeks’ treatment with manidipine 10 or 20mg once daily in a 12-week noncomparative trial in 16 patients with renal impairment of various causes; these reductions were maintained until study completion. Similar long term efficacy was demonstrated with manidipine 5 to 20mg once daily in a 48-week study in 32 patients with renal impairment. BP reductions from baseline with manidipine 10 or 20 mg/day were similar to those with nifedipine gastrointestinal therapeutic system (GITS) 30 or 60 mg/day in 83 patients with chronic renal failure.
Tolerability
Manidipine was well tolerated in clinical trials, with most adverse effects related to vasodilation. Ankle oedema (6%), headache (3.8%), palpitation (2.7%), flushing (2.2%), dizziness (1.6%), rash (0.5%) and fatigue (0.5%) were the most commonly reported adverse events in a noncomparative trial involving 183 patients ith mild to moderate hypertension treated with manidipine 10 or 20mg daily for up to 12 months.
Adverse events with manidipine treatment (10 or 20 mg/day) appeared to occur with a similar incidence overall to those with placebo, amlodipine (5 or 10 mg/day), felodipine (5 or 10 mg/day), lacidipine (4 or 6 mg/day), controlled release nifedipine (20 to 40mg twice daily) or enalapril (10 or 20 mg/day) in randomised or nonrandomised clinical trials in patients with essential hypertension(including some patients with type 2 diabetes mellitus). However, manidipine appears to have less potential for oedema than amlodipine.
Dosage and Administration
Manidipine is indicated for the treatment of essential hypertension at a recommended initial dosage of 10mg once daily. In patients with an initial unsatisfactory response after 1 or 2 weeks, the dosage should be increased to 20mg oncedaily.
Manidipine is contraindicated in paediatric patients and women who are pregnant or breast feeding. In addition, dosage reductions are recommended for patients with hepatic impairment and patients over the age of 65 years, but not for patients with renal function impairment.










Similar content being viewed by others
References
Dhein S, Salameh A, Berkels R, et al. Dual mode of action of dihydropyridine calcium antagonists: a role for nitric oxide. Drugs 1999 Sep; 58: 397–404
Alderman M, Arakawa K, Beilin L, et al. 1999 World Health Organization — International Society of Hypertension Guidelines for the Management of Hypertension. Blood Press 1999; 8 Suppl. 1: 9–43
Joint National Committee on Prevention Detection Evaluation and Treatment of High Blood Pressure NHBPEPCC. The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Arch Intern Med 1997 Nov 24; 157: 2413–46
Singh V, Christiana J, Frishman WH. How to use calcium antagonists in hypertension: putting the JNC-VI guidelines into practice. Drugs 1999 Oct; 58: 579–87
Luscher TF, Cosentino F. The classification of calcium antagonists and their selection in the treatment of hypertension: a reappraisal. Drugs 1998; 55(4): 509–17
Shibouta Y, Kitayoshi T, Kitoh G, et al. Calcium channel blocking action of franidipine hydrochloride (CV-4093.2HC1) in vitro and in vivo. Jpn J Pharmacol 1988 Dec; 48: 463–72
Okabe K, Terada K, Kitamura K, et al. Selective and long-lasting inhibitory actions of the dihydropyridine derivative, CV-4093, on calcium currents in smooth muscle cells of the rabbit pulmonary artery. J Pharmacol Exp Ther 1987 Nov; 243: 703–10
Nakaya H, Hattori Y, Nakao Y, et al. Cardiac versus vascular effects of a new dihydropyridine derivative, CV- 4093. In. vitro comparison with other calcium antagonists. Eur J Pharmacol 1988 Jan 27; 146: 35–43
Tanabe M, Kawazoe K, Kito G, et al. Effects of manidipine hydrochloride (CV-4093.2HC1) on systemic hemodynamics, cardiac function and plasma renin activity in conscious renal hypertensive dogs [in Japanese]. Jpn Pharmacol Ther 1989; 17: 779–88
Tanabe M, Kawazoe K, Kito G, et al. Effects of manidipine hydrochloride (CV-4093 (2HCI)) on hemodynamics and cardiac function in conscious normotensive dogs [in Japanese]. Jpn Pharmacol Ther 1989; 17(3): 55–66
Oliviero M, Turco S, Tammaro P, et al. Manidipina versus amlodipina in type II diabetic patients with hypertension: comparison in double blind [abstract]. Diabetologia 1998 Aug;41 Suppl. 1: A340
Celentano A, Crivaro M, Perticone F, et al. Anti-hypertensive effect of manidipine: 24 hours monitoring evaluation and Doppler-echocardiographic remarks. Blood Press 1996; 5 Suppl. 5: 29–35
Fogari R, Zoppi A, Lusardi P, et al. Evaluation by 24-hour ambulatory blood pressure monitoring of efficacy of manidipine hydrochloride 10, 20 or 40 mg once daily as compared to placebo in treating mild to moderate essential hypertension: a double-blind, randomized, parallel group, placebo-controlled study. Blood Press 1996; 5 Suppl. 5:16–23
Fogari R, Zoppi A, Mugellini A, et al. Effect of low-dose manidipine on ambulatory blood pressure in very elderly hypertensives. Cardiovasc Drugs Ther 1999 May; 13: 243–8
Fogari R, Zoppi A, Lusardi P, et al. Efficacy and tolerability of manidipine hydrochloride in the long-term treatment of mildmoderate hypertension. Manidipine Efficacy in Long-Term Treatment Group. Blood Press 1996; 5 Suppl. 5: 24–8
Nakamura T, Honma H, Kohno I, et al. Efficacy of manidipine on circadian blood pressure in essential hypertension. Blood Press 1992; 3 Suppl. 3: 94–101
Crivaro M, Celentano A, Palmieri V, et al. Mild arterial hypertension and impaired glucose tolerance: short-term effects of manidipine hydrochloride. Adv Ther 1996; 13(6): 365–72
Atarashi K, Takagi M, Minami M, et al. Effects of manidipine and delapril on glucose and lipid metabolism in hypertensive patients with non-insulin-dependent diabetes mellitus. Blood Press 1992; 1 Suppl. 3: 130–4
Mancia G, Omboni S, Agabiti-Rosei E, et al. Antihypertensive efficacy of manidipine and enalapril in hypertensive diabetic patients. J Cardiovasc Pharmacol 2000; 35(6): 926–31
Saruta T, Suzuki H. Efficacy of manidipine in the treatment of hypertension with renal impairment: a multicenter trial. Am Heart J 1993 Feb; 125 (2 Pt 2): 630–4
Mizuno K, Haga H, Takahashi M, et al. Clinical evaluation of the efficacy and safety of manidipine in hypertensive patients with renal disorders. Blood Press 1992; 3 Suppl. 3: 119–23
Fogari R, Zoppi A, Corradi L, et al. Effects of different dihydropyridine calcium antagonists on plasma norepinephrine in essential hypertension. J Hypertens 2000; 18: 1871–5
Lai Y-H, Guh J-Y, Chen H-C, et al. Effects of manidipine hydrochloride on blood pressure in hypertensive patients-a comparison with nifedipine retard. Kaohsiung J Med Sci 1993 Nov; 9: 625–31
Hase MI, Hase O, Igawa S, et al. Reduction of left ventricular mass by manidipine hydrochloride [abstract]. Am J Hypertens 1998 Apr; 11 (Pt 2):81
Takahashi K, Katoh T, Fukunaga M, et al. Studies on the glomerular microcirculatory actions of manidipine and its modulation of the systemic and renal effects of endothelin. Am Heart J 1993 Feb; 125 (2 Pt 2): 609–19
Takabatake T, Ushiogi Y, Ise T, et al. Effect of calcium antagonist, manidipine hydrochloride, on renal hemodynamics and tubuloglomerular feedback in spontaneously hypertensive rats. Am Heart J 1993 Feb; 125 (2 Pt 2): 578–81
Takabatake T, Ohta H, Sasaki T, et al. Renal effects of manidipine hydrochloride: a new calcium antagonist in hypertensive patients. Eur J Clin Pharmacol 1993; 45: 321–5
Murakami K, Kimura G, Imanishi M, et al. Effect of manidipine, a new calcium antagonist, on intrarenal hemodynamics in essential hypertension. Blood Press 1992; 3 Suppl. 3: 114–8
Nagaoka A, Shibota M. Natriuretic action of manidipine hydrochloride, a new calcium channel blocker, in spontaneously hypertensive rats. Jpn J Pharmacol 1989 Oct; 51: 299–301
Morimoto S, Ohyama T, Hisaki K, et al. Effects of CV-4093, a new dihydropyridine calcium channel blocker, on renal hemodynamics and function in stroke-prone spontaneously hypertensive rats (SHRSP). Jpn J Pharmacol 1989 Oct; 51: 257–65
Marusaki S, Shimamoto K, Komura H, et al. Effects of manidipine on renal sodium and calcium handling in patients with mild essential hypertension. Ther Res 1993; 14(7): 128–33
Kobayashi S, Hishida A. Manidipine attenuates a progressive renal injury in remnant kidneys of rats. Blood Press 1992; 3 Suppl. 3: 80–4
Kobayashi S, Hishida A. Effects of a calcium antagonist, manidipine, on progressive renal injury associated with mild hypertension in remnant kidneys [see comments]. J Lab Clin Med 1995 May; 125: 572–80
Fujimaki M, Nagase M, Uchida S. Long-term effect of manidipine on renal function and structure in uninephrectomized spontaneously hypertensive rats. Clin Exp Pharmacol Physiol 1997 Jul; 24: 506–12
Reams GP, Villarreal D, Wu Z, et al. An evaluation of the renal protective effect of manidipine in the uninephrectomized spontaneously hypertensive rat. Am Heart J 1993 Feb; 125 (2 Pt 2): 620–5
Yamakado M, Shimomura H, Maehata E. Renoprotection of calcium antagonist: effect of manidipine on urinary microalbumin excretion and lipid peroxidation [abstract]. Am J Hypertens 1996 Apr; 9 (Pt 2): 154
Deerochanawong C, Kornthong P, Phongwiratchai S, et al. Effects in urinary albumin excretion and renal function changes by delapril and manidipine in normotensive type 2 diabetic patients with microalbuminuria. J Med Assoc Thai 2001 Feb; 84(2): 234–41
Okabe T, Hirobe Y, Hashizume H, et al. Effect of manidipine hydrochloride on persistent microalbuminuria in normotensive diabetic patients [in Japanese]. Shinryo to Shinyaku 1993; 30(9): 1715–8
Shimizu H, Miyashita K, Uehara Y, et al. Effects of manidipine hydrochloride on proteinuria in diabetic patients with hypertension [in Japanese]. Shinyaku to Rinsho 1994 Dec; 43: 2549–53
Ishida S, Banu N, Okamura M, et al. The effect of angiotensin converting enzyme inhibitor and calcium antagonists on urinary albumin excretion in non-insulin-dependent diabetic patients [abstract]. 15th International Diabetes Federation Congress 1994: Kobe, Jpn, 355
Inaba M, Maruno Y, Kosegawa I, et al. Effects of benazepril and manidipine on the progression of diabetic nephropathy [abstract]. Koketsuatsu 1998 Dec; 21: 315
Shiba T, Inoue M, Tada H, et al. Delapril versus manidipine in hypertensive therapy to halt the type-2-diabetes-mellitus-associated nephropathy. Diabetes Res Clin Pract 2000 Feb; 47: 97–104
Saku K, Zhang B, Hirata K, et al. Effects of manidipine and delapril on serum lipids, lipoproteins, and apolipoproteins in patients with mild to moderate essential hypertension: a randomized trial with one-year follow-up. Clin Ther 1992 Nov–Dec; 14:813–20
Suzuki S, Ohtomo M, Satoh Y, et al. Effect of manidipine and delapril on insulin sensitivity in type 2 diabetic patients with essential hypertension. Diabetes Res Clin Pract 1996 Jun; 33: 43–51
Iimura O, Shimamoto K, Masuda A, et al. Effects of a calcium channel blocker, manidipine, on insulin sensitivity in essential hypertensives. J Diabetes Complications 1995 Oct–Dec; 9:215–9
Fogari R, Malamani GD, Zoppi A, et al. Manidipine has less oedematigenous potential than amlodipine. J Hypertens 2000 Jun; 18 Suppl. 2: S154–155
Nagaoka A. Pharmacological prevention of cerebral stroke in stroke-prone spontaneously hypertensive rats. J Hypertens 1986; 4 Suppl. 3: S523–525
Morimoto S, Matsumura Y. Manidipine hydrochloride [CV-4093 (2HC1)]. Cardiovasc Drug Rev 1991; 9(3): 207–22
Pfaffendorf M, Mathy MJ, van Zwieten PA. Effects of manidipine and other calcium antagonists on rat renal arcuate arteries. Am Heart J 1993 Feb; 125 (2 Pt 2): 571–7
Nagaoka A, Kito G, Nagai Y. Antihypertensive action, calcium channel blocking action and receptor binding activity of manidipine hydrochloride in experimental animals [in Japanese]. Jpn Pharmacol Ther 1990; 18(7): 11–20
Ogihara T. Practitioner’s Trial on the Efficacy of Antihypertensive Treatment in the Elderly Hypertension (the PATE-Hypertension study) in Japan [in Japanese]. Am J Hypertens 2000; 13 (5 pt 1): 461–7
Hama H. Antihypertensive efficacy of amlodipine and manidipine on 24-hour blood pressure in patients with essential hypertension [in Japanese]. Therapeutic Research 1999; 20(2): 199–207
Okuda Y, Asano H, Ito U, et al. Long-term efficacy and safety of manidipine hydrochloride in the treatment of hypertension patients [in Japanese]. Yakuri to Chiryo 1993 May; 21: 1539–57
Kaneko Y, Fukiyama K, Iimura O, et al. Clinical study of manidipine hydrochloride in essential hypertension: a double-blind controlled study with nicardipine hydrochloride. J Clin Exp Med 1989; 151(8): 471–92
Nagasawa K, Kitamoto K, Nagasawa T. A 3-year long-term evaluation of the efficacy and safety of manidipine hydrochloride (Calslot tablet) in the elderly with essential hypertension: a multicentre collaborative study [in Japanese]. Rinsho to Kenkyu 1997; 74(10): 2630–8
Zanchetti A, Omboni S, La Commare P, et al. Efficacy, tolerability and impact on quality of life and long-term treatment with manidipine or amlodipine in patients with essential hypertension. J Cardiovasc Pharmacol. In press
Mancia G, Celetano A, Portioli I, et al. Evaluation of the antihypertensive and metabolic efficacy of manidipine (10/20 mg/day) in the treatment of mild to moderate essential arterial hypertension in patients with noninsulin dependent diabetes mellitus. A randomised, parallel group study versus amlodipine (5/10 mg/day). Chiesi Farmaceutici, 1999. (Data on file)
Otero L, Degaute, Vandenbroucke M, et al. Evaluation of the antihypertensive and metabolic effect of manidipine (10/20 mg/day) in the treatment of essential arterial hypertension with non insulin dependent diabetes mellitus (type II). Multicentre, randomized, double blind, controlled parallel group, comparative trial with Enalapril (10/20 mg/day). Chiesi Farmaceutici, 2000. (Data on file)
Andreucci VE, Russo D, d’Amato R, et al. Antihypertensive treatment in the nephrotic patients [in Italian]. Cardiologia 1996; 41 Suppl. 1: 25–9
Morimoto S, Hisaki K, Matsumura Y. Effects of manidipine hydrochloride, nisoldipine and nitrendipine on renal hemodynamics and function in stroke-prone spontaneously hypertensive rats (SHRSP) [in Japanese]. Jpn Pharmacol Ther 1990; 18(8): 33–42
Sabbatini M, Vitaioli, Baldoni E, et al. Nephroprotective effect of treatment with calcium channel blockers in spontaneously hypertensive rats. J Pharmacol Exp Ther 2000; 294(3): 948–54
Sabbatini M, Leonardi A, Testa R, et al. Effect of calcium antagonists on glomerular arterioles in spontaneously hypertensive rats. Hypertension 2000 Mar; 35: 775–9
Nayler WG, Panagiotopoulos S. The antiatherosclerotic effect of the calcium antagonists and their implications in hypertension. Am Heart J 1993 Feb; 125 (2 Pt 2): 626–9
Fogari R, Malamani GD, Savino S, et al. Effects of different dihydropyridine calcium antagonists on pretibial subcutaneous tissue pressure in hypertensive patients [abstract]. Am J Hypertens 1998 Apr; 11 (Pt 2): 114
Nishikawa T, Omura M, Iizuka T, et al. Effect of manidipine chloride on various aspects of endocrine function, including plasma levels of endothelin-1 and human atrial natriuretic peptide, in patients with essential hypertension. Clin Ther 1996 Jul–Aug; 18:680–6
Hirakata H, lino K, Ishida I, et al. Effects of a new calcium antagonist, manidipine, on the renal hemodynamics and the vasoactive humoral factors in patients with diabetes mellitus. Blood Press 1992; 1 Suppl. 3: 124–9
Rosillon D, Stockis A, Poli G, et al. Food effect on the oral bioavailability of Manidipine: single dose, randomized, crossover study in healthy male subjects. Eur J Drug Metab Pharmacokinet 1998 Apr–Jun; 23: 197–202
Deroubaix X, Lins RL, Lens S, et al. Single dose pharmacokinetics of manidipine in hepatic impaired patients and healthy controls. Int J Clin Pharmacol Ther 1998 Jul; 36: 386–91
Tateno M. Pharmacokinetic study of CV-4093 (2 HC1) at single dose on healthy subjects [in Japanese]. Rinsho Iyaku 1989 Sep; 5: 1765–77
Demblon D, Lins R, Rosillon D, et al. Final report. Randomized cross-over study of the influence of food on the pharmacokinetics of manidipine (20 mg tablet) and its pyridone metabolite in 12 healthy male Caucasian volunteers. Chiesi Farmaceutici S.p.A. Jul 1993. (Data on file)
Chiesi Farmaceutici S.p.A/Takeda Italia Farmaceutici. Summary of product characteristics. Chiesi Farmaceutici S.p.A. Takeda Italia Farmaceutici, Jul 2000
Katoh M, Nakajima M, Shimada N, et al. Inhibition of human cytochrome P450 enzymes by 1,4-dihydropyridine calcium antagonists: prediction of in vivo drug-drug interactions. Eur J Clin Pharmacol 2000 Feb–Mar; 55: 843–52
Hashimoto Y, Shimizu A, Kuroda T, et al. Effect of dihydropyridine calcium channel blockers on the plasma digoxin level [in Japanese]. Jpn J Clin Pharmacol Ther 1996; 27(4): 665–71
Ogihara T, Nakagawa M, Ishikawa H, et al. Effect of manidipine, a novel calcium channel blocker, on quality of life in hypertensive patients. Blood Press 1992; 3 Suppl. 3: 135–9
Chiesi Farmaceutici S.p.A. Clinical expert report. Chiesi Farmaceutici S.p.A. Italy. (Data on file)
Colhoun HM, Dong W, Poulter NR. Blood pressure screening, management and control in England: results from the health survey for England 1994. J Hypertens 1994; 16: 747–52
Guideline Subcommittee. World Health Organization — International Society of Hypertension Guideline for the Management of Hypertension. Hypertension 1999; 17: 151–83
Singh RB. Hypertension and stroke in Asia: prevalence, control and strategies in developing countries for prevention. J Hum Hypertens 2000; 14: 749–63
Jones DW. Hypertension in East Asia. Hypertension 1995; 8: 111S–4S
Ramsay LE, Williams B, Johnston GD, et al. Guidelines for management of hypertension: report of the third working party of the British Hypertension Society. J Hum Hypertens 1999 Sep; 13: 569–92
Samuelsson O, Wilhelmsen L, Elmfeldt D, et al. Predictors of cardiovascular morbidity in treated hypertension: results from the Primary Preventive Trial in Goteborg. Swed J Hypertens 1985; 3: 167–76
Isles CG, Walker LM, Beevers GD, et al. Mortality in patients of the Glasgow Blood Pressure Clinic. J Hypertens 1986; 4: 141–56
Furberg CD, Psaty BM. Calcium antagonists: not appropriate as first line antihypertensive agents. Am J Hypertens 1996; 9(2): 122–5
Pahor M, Guralnik JM, Salive ME, et al. Do calcium channel blockers increase the risk of cancer? Am J Hypertens 1996; 9: 695–9
Pahor M, Guralnik JM, Ferrucci L, et al. Calcium channel blockade and incidence of cancer in aged populations. Lancet 1996; 348: 493–7
Epstein M. Role of a third generation calcium antagonist in the management of hypertension. Drugs 1999; 57 Suppl. 1: 1–10
Epstein M. Calcium antagonists should continue to be used for first-line treatment of hypertension. Arch Intern Med 1995; 155: 2150–6
Epstein M. Calcium antagonists: still appropriate as first-line antihypertensive agents. Am J Hypertens 1996; 9: 110–21
Stanton AV. Calcium channel blockers: the jury is still out on whether they cause heart attacks and suicide. BMJ 1998; 316: 1471–2
Cutler JA. Calcium-channel blockers for hypertension — uncertainty continues. N Engl J Med 1998; 338: 679–81
Salvetti A, Mattei P, Sudano I. Renal protection and antihypertensive drugs: current status. Drugs 1999; 57(5): 665–93
Locatelli F, Del Vecchio L, Marai P, et al. The renoprotective effect of antihypertensive drugs. J Nephrol 1998; 11(6): 330–6
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cheer, S.M., McClellan, K. Manidipine. Drugs 61, 1777–1799 (2001). https://doi.org/10.2165/00003495-200161120-00010
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200161120-00010