Abstract
Basic research that has focused on achieving a mechanistic understanding of mitosis has provided unprecedented molecular and biochemical insights into this highly complex phase of the cell cycle. The discovery process has uncovered an ever-expanding list of novel proteins that orchestrate and coordinate spindle formation and chromosome dynamics during mitosis. That many of these proteins appear to function solely in mitosis makes them ideal targets for the development of mitosis-specific cancer drugs. The clinical successes seen with anti-microtubule drugs such as taxanes and the vinca alkaloids have also encouraged the development of drugs that specifically target mitosis. Drugs that selectively inhibit mitotic kinesins involved in spindle and kinetochorefunctions, as well as kinases that regulate these activities, are currently in various stages of clinical trials. Ourincreased understanding of mitosis has also revealed that this process is targeted by inhibitors of farnesyltransferase, histone deacetylase, and Hsp90. Although these drugs were originally designed to block cell proliferation by inhibiting signaling pathways and altering gene expression, it is clear now that these drugs can also directly interfere with the mitotic process.
The increased attention to mitosis as a chemotherapeutic target has also raised an important issue regarding the cellular determinants that specify drug sensitivity. One likely contribution is the mitotic checkpoint, a fail safe mechanism that delays mitotic exit so that cells whose chromosomes are not properly attached to the spindle have extra time to correct their errors. As the biochemical activity of the mitotic checkpoint is finite, cells cannot indefinitely sustain the delay, as in cases where cells are treated with anti-mitotic drugs. When the mitotic checkpoint activity is eventually lost, cells will exit mitosis and become aneuploid. While many of the aneuploid cells may die because of massive chromosome imbalance, survivors that continue to proliferate will no doubt be selected. This is clearly an undesirable outcome, thus efforts to obtain fundamental insights into why some cells that arrest in mitosis die without exiting mitosis will be exceedingly important in enhancing our understanding of the drug sensitivity of cancer cells.
Similar content being viewed by others
References
Mitchison T, Kirschner M, Authors FN, et al. Dynamic instability of microtubule growth. Nature 1984; 312(5991): 237–42
Palmer CG, Livengood D, Warren AK, et al. The action of the vincaleukolastine on mitosis in vitro. Exp Cell Res 1960; 20: 198–201
Samson F, Donoso JA, Heller-Bettinger I, et al. Nocodazole action on tubulin assembly, axonal ultrastructure and fast axoplasmic transport. J Pharmacol Exp Ther 1979; 208(3): 411–7
Schiff PB, Horwitz SB. Taxol stabilizes microtubules in mouse fibroblast cells. Proc Natl Acad Sci U S A 1980; 77(3): 1561–5
Chan GK, Liu ST, Yen TJ. Kinetochore structure and function. Trends Cell Biol 2005 Nov; 15(11): 589–98
Wood KW, Cornwell WD, Jackson JR. Past and future of the mitotic spindle as an oncology target. Curr Opin Pharmacol 2001; 1(4): 370–7
Jablonski SA, Liu ST, Yen TJ. Targeting the kinetochore for mitosis-specific inhibitors. Cancer Biol Ther 2003; 2(3): 236–41
Brown KD, Coulson RM, Yen TJ, et al. Cyclin-like accumulation and loss of the putative kinetochore motor CENP-E results from coupling continuous synthesis with specific degradation at the end of mitosis. J Cell Biol 1994; 125(6): 1303–12
Sharp DJ, Rogers GC, Scholey JM. Microtubule motors in mitosis. Nature 2000; 407(6800): 41–7
Kapoor TM, Mayer TU, Coughlin ML, et al. Probing spindle assembly mechanisms with monastrol, a small molecule inhibitor of the mitotic kinesin, Eg5. J Cell Biol 2000; 150(5): 975–88
Mayer TU, Kapoor TM, Haggarty SJ, et al. Small molecule inhibitor of mitotic spindle bipolarity identified in a phenotype-based screen. Science 1999; 286(5441): 971–4
Luo L, Carson JD, Dhanak D, et al. Mechanism of inhibition of human KSP by monastrol: insights from kinetic analysis and the effect of ionic strength on KSP inhibition. Biochemistry 2004; 43(48): 15258–66
Stein MN, Rubin PD, Scott R, et al. Phase I clinical and pharmacokinetic (PK) trial of the kinesin spindle protein (KSP) inhibitor MK-0731 in cancer patients [abstract]. 2006 ASCO Annual Meeting Proceedings Part I. J Clin Oncol 2006; 24(18S, Jun 20 Suppl.): 2001
Holen KD, Belani CP, Wilding G, et al. Phase I study to determine tolerability and pharmacokinetics (PK) of SB-743921, a novel kinesin spindle protein (KSP) inhibitor [abstract]. 2006 ASCO Annual Meeting Proceedings Part I. J Clin Oncol 2006; 24(18S, Jun 20 Suppl.): 2000
Schaar BT, Chan GK, Maddox P, et al. CENP-E function at kinetochores is essential for chromosome alignment. J Cell Biol 1997; 139(6): 1373–82
McEwen BF, Chan GK, Zubrowski B, et al. CENP-E is essential for reliable bioriented spindle attachment, but chromosome alignment can be achieved via redundant mechanisms in mammalian cells. Mol Biol Cell 2001; 12(9): 2776–89
Yao X, Abrieu A, Zheng Y, et al. CENP-E forms a link between attachment of spindle microtubules to kinetochores and the mitotic checkpoint. Nat Cell Biol 2000; 2(8): 484–91
Chan GK, Schaar BT, Yen J. Characterization of the kinetochore binding domain of CENP-E reveals interactions with the kinetochore proteins CENP-F and hBUBRl. J Cell Biol 1998; 143(1): 49–63
Desai A, Verma S, Mitchison TJ, et al. Kin I kinesins are microtubule-destabilizing enzymes. Cell 1999; 96(1): 69–78
Maney T, Ginkel LM, Hunter AW, et al. The kinetochore of higher eucaryotes: a molecular view. Int Rev Cytol 2000; 194: 67–131
Hunter AW, Caplow M, Coy DL, et al. The kinesin-related protein MCAK is a microtubule depolymerase that forms an ATP-hydrolyzing complex at microtubule ends. Mol Cell 2003; 11(2): 445–57
Huang H, Feng J, Famulski J, et al. Tripin/hSgo2 recruits MCAK to the inner centromere to correct defective kinetochore attachments. J Cell Biol 2007 May 7; 177(3): 413–24
Cimini D, Degrassi F. Aneuploidy: a matter of bad connections. Trends Cell Biol 2005; 15(8): 442–51
Aoki K, Nakaseko Y, Kinoshita K, et al. CDC2 phosphorylation of the fission yeast dis1 ensures accurate chromosome segregation. Curr Biol 2006; 16 (16): 1627-35
Yao X, Anderson KL, Cleveland DW. The microtubule-dependent motor centromere-associated protein E (CENP-E) is an integral component of kinetochore corona fibers that link centromeres to spindle microtubules. J Cell Biol 1997; 139(2): 435–47
Abrieu A, Kahana JA, Wood KW, et al. CENP-E as an essential component of the mitotic checkpoint in vitro. Cell 2000; 102(6): 817–26
Cytokinetics, Inc. Cytokinetics announces selection of development candidate directed to second mitotic kinesin target. Press release: 2005 Dec 13 [online]. Available from URL: http://www.cytokinetics.com/cyto/pr_1134484958 [Accessed 2007 Jun 27]
Willumsen BM, Norris K, Papageorge AG, et al. Harvey murine sarcoma virus p21 ras protein: biological and biochemical significance of the cysteine nearest the carboxy terminus. EMBO J 1984; 3(11): 2581–5
Kato K, Cox AD, Hisaka MM, et al. Isoprenoid addition to Ras protein is the critical modification for its membrane association and transforming activity. Proc Natl Acad Sci U S A 1992; 89(14): 6403–7
Bishop WR, Kirschmeier P, Baum C. Farnesyl transferase inhibitors: mechanism of action, translational studies and clinical evaluation. Cancer Biol Ther 2003; 2(4 Suppl.1): S96–104
Ashar HR, James L, Gray K, et al. Farnesyl transferase inhibitors block the farnesylation of CENP-E and CENP-F and alter the association of CENP-E with the microtubules. J Biol Chem 2000; 275(39): 30451–7
Hussein D, Taylor SS. Farnesylation of Cenp-F is required for G2/M progression and degradation after mitosis. J Cell Sci 2002; 115 (Pt 17): 3403–14
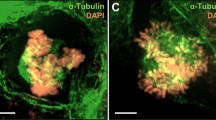
Crespo NC, Ohkanda J, Yen TJ, et al. The farnesyl transferase inhibitor, FTI-2153, blocks bipolar spindle formation and chromosome alignment and causes prometaphase accumulation during mitosis of human lung cancer cells. J Biol Chem 2001; 276(19): 16161–7
Adnane J, Chen Z, Ohkanda J, et al. Upregulation of Rhob transcription, not inhibition of Rhob prenylation, as a potential mechanism by which farnesyltransferase and geranyltransferase I inhibitors suppress human tumor growth [abstract]. 92nd AACR Annual Meeting; 2001 Mar 24–28; New Orleans (LA). Proc Am Assoc Cancer Res 2001; 42: 1406
Crespo N, Sun J, Ohkanda J, et al. Constitutively activated AKT-2 blocks the ability of FTI-2148 to inhibit the growth and to induce apoptosis of the human ovarian carcinoma OCVAR3 in nude mice [abstract]. 92nd AACR Annual Meeting; 2001 Mar 24–28; New Orleans (LA). Proc Am Assoc Cancer Res 2001; 42: 1403
Crespo N, Ohkanda J, Yen JT, et al. FTI-2153 inhibits bipolar spindle formation in human cancer cells: a mechanism for FTI-induced mitotic arrest [abstract]. 92nd AACR Annual Meeting; 2001 Mar 24–28; New Orleans (LA). Proc Am Assoc Cancer Res 2001; 42: 2619
Sun J, Adnan J, Jackson R, et al. Loss of P21WAF1/CIP1 results in delayed FTI-2148-induced mammary tumor regression and accelerated tumor regrowth after FTI removal in an oncogenic H-RAS transgenic mouse model [abstract]. 92nd AACR Annual Meeting; 2001 Mar 24–28; New Orleans (LA). Proc Am Assoc Cancer Res 2001; 42: 2620
Oh SH, Hong WK, Lee HY. Insulin-like growth factor receptor signaling pathways and resistance to farnesyl transferase inhibitor SCH66336 (lonafarnib) in head and neck squamous cell carcinoma [abstract]. 97th AACR Annual Meeting; 2006 Apr 1–5; Washington, DC. Proc Am Assoc Cancer Res 2006; 1: 1246
Tap WD, Jiang C, Eilber FC, et al. Promising activity of farnesyltransferase inhibitors across seven different sarcoma subtypes [abstract]. 97th AACR Annual Meeting; 2006 Apr 1–5; Washington, DC. Proc Am Assoc Cancer Res 2006; 1: 3805
O’Brate AM, Marcus AI, Buey R, et al. Farnesyltransferase inhibitors (FTI) enhance taxol-binding to microtubules and reverse taxane-resistance [abstract]. 97th AACR Annual Meeting; 2006 Apr 1–5; Washington, DC. Proc Am Assoc Cancer Res 2006; 1: 3803
Whitesell L, Lindquist SL. HSP90 and the chaperoning of cancer. Nat Rev Cancer 2005; 5(10): 761–72
Niikura Y, Ohta S, Vandenbeldt KJ, et al. 17-AAG, an Hsp90 inhibitor, causes kinetochore defects: a novel mechanism by which 17-AAG inhibits cell proliferation. Oncogene 2006; 25(30): 4133–46
de Career G, do Carmo AM, Lallena MJ, et al. Requirement of Hsp90 for centrosomal function reflects its regulation of Polo kinase stability. EMBO J 2001; 20(11): 2878–84
Takai N, Hamanaka R, Yoshimatsu J, et al. Polo-like kinases (Plks) and cancer. Oncogene 2005; 24(2): 287–91
Gumireddy K, Reddy MV, Cosenza SC, et al. ON01910, a non-ATP-competitive small molecule inhibitor of Plk1, is a potent anticancer agent [erratum appears in Cancer Cell 2005 May; 7 (5): 497 Note: Boomi Nathan R (corrected to Boominathan R)]. Cancer Cell 2005; 7(3): 275–86
Smith P, Syed N, Crook T. Epigenetic inactivation implies a tumor suppressor function in hematologic malignancies for Polo-like kinase 2 but not Polo-like kinase 3. Cell Cycle 2006; 5(12): 1262–4
Syed N, Smith P, Sullivan A, et al. Transcriptional silencing of Polo-like kinase 2 (SNK/PLK2) is a frequent event in B-cell malignancies. Blood 2006; 107(1): 250–6
Ko MA, Rosario CO, Hudson JW, et al. Plk4 haploinsufficiency causes mitotic infidelity and carcinogenesis. Nat Genet 2005; 37(8): 883–8
Shannon KB, Salmon ED. Chromosome dynamics: new light on Aurora B kinase function. Curr Biol 2002; 12(13): R458–60
Ditchfield C, Johnson VL, Tighe A, et al. Aurora B couples chromosome alignment with anaphase by targeting BubR1, Mad2, and Cenp-E to kinetochores. J Cell Biol 2003; 161(2): 267–80
Li JJ, Li SA. Mitotic kinases: the key to duplication, segregation, and cytokinesis errors, chromosomal instability, and oncogenesis. Pharmacol Ther 2006; 111(3): 974–84
Katayama H, Brinkley WR, Sen S. The Aurora kinases: role in cell transformation and tumorigenesis. Cancer Metastasis Rev 2003; 22(4): 451–64
Cochran JC, Sontag CA, Maliga Z, et al. Mechanistic analysis of the mitotic kinesin Eg5. J Biol Chem 2004; 279(37): 38861–70
Adams RR, Carmena M, Earnshaw WC. Chromosomal passengers and the (Aurora) ABCs of mitosis. Trends Cell Biol 2001; 11(2): 49–54
Hauf S, Cole RW, LaTerra S, et al. The small molecule Hesperadin reveals a role for Aurora B in correcting kinetochore-microtubule attachment and in maintaining the spindle assembly checkpoint. J Cell Biol 2003; 161(2): 281–94
Ditchfield C, Keen N, Taylor SS. The Ipl1/Aurora kinase family: methods of inhibition and functional analysis in mammalian cells. Methods Mol Biol 2005; 296: 371–81
Andrews PD, Ovechkina Y, Morrice N, et al. Aurora B regulates MCAK at the mitotic centromere. Dev Cell 2004; 6(2): 253–68
Lan W, Zhang X, Kline-Smith SL, et al. Aurora B phosphorylates centromeric MCAK and regulates its localization and microtubule depolymerization activity. Curr Biol 2004; 14(4): 273–86
Liu ST, Rattner JB, Jablonski SA, et al. Mapping the assembly pathways that specify formation of the trilaminar kinetochore plates in human cells. J Cell Biol 2006; 175(1): 41–53
Andrews PD. Aurora kinases: shining lights on the therapeutic horizon? Oncogene 2005; 24(32): 5005–15
Rubin EH, Shapiro GI, Stein MN, et al. A phase I clinical and pharmacokinetic (PK) trial of the Aurora kinase (AK) inhibitor MK-0457 in cancer patients [abstract]. 2006 ASCO Annual Meeting Proceedings Part I. J Clin Oncol 2006; 24(18S, Jun 20 Suppl.): 3009
Medical News Today. Astex Therapeutics initiates clinical trial with investigational anti-cancer drug AT9283 [online]. Available from URL: http://www.medicalnewstoday.com/medicalnews.php?newsid=52769 [Accessed 2007 Jun 21]
Warner SL, Munoz RM, Stafford P, et al. Comparing Aurora A and Aurora B as molecular targets for growth inhibition of pancreatic cancer cells. Mol Cancer Ther 2006; 5(10): 2450–8
Dai W, Wang Q, Liu T, et al. Slippage of mitotic arrest and enhanced tumor development in mice with BubR1 haploinsufficiency. Cancer Res 2004; 64(2): 440–5
Dobles M, Liberal V, Scott ML, et al. Chromosome missegregation and apoptosis in mice lacking the mitotic checkpoint protein Mad2. Cell 2000 Jun 9; 101(6): 635–45
Babu JR, Jeganathan KB, Baker DJ, et al. Rae1 is an essential mitotic checkpoint regulator that cooperates with Bub3 to prevent chromosome missegregation. J Cell Biol 2003 Feb 3; 160(3): 341–53
Baker DJ, Jeganathan KB, Cameron JD, et al. BubR1 insufficiency causes early onset of aging-associated phenotypes and infertility in mice. Nat Genet 2004 Jul; 36(7): 744–9
Cahill DP, da Costa LT, Carson-Walter EB, et al. Characterization of MAD2B and other mitotic spindle checkpoint genes. Genomics 1999 Jun 1; 58(2): 181–7
Imai Y, Shiratori Y, Kato N, et al. Mutational inactivation of mitotic checkpoint genes, hsMAD2 and hBUB1, is rare in sporadic digestive tract cancers. Jpn J Cancer Res 1999 Aug; 90(8): 837–40
Yamaguchi K, Okami K, Hibi K, et al. Mutation analysis of hBUB1 in aneuploid HNSCC and lung cancer cell lines. Cancer Lett 1999 May 24; 139(2): 183–7
Myrie KA, Percy MJ, Azim JN, et al. Mutation and expression analysis of human BUB1 and BUB1B in anrrest deficient 2 expression induces chemosensitization to a DNA-daeuploid breast cancer cell lines. Cancer Lett 2000 May 1; 152(2): 193–9
Sato M, Sekido Y, Horio Y, et al. Infrequent mutation of the hBUB1 and hBUBR1 genes in human lung cancer. Jpn J Cancer Res 2000 May; 97(5): 504–9
Masuda A, Maeno K, Nakagawa T, et al. Association between mitotic spindle checkpoint impairment and susceptibility to the induction of apoptosis by anti-microtubule agents in human lung cancers. Am J Pathol 2003; 163(3): 1109–16
Lee EA, Keutmann MK, Dowling ML, et al. Inactivation of the mitotic checkpoint as a determinant of the efficacy of microtubule-targeted drugs in killing human cancer cells. Mol Cancer Ther 2004; 3(6): 661–9
Kops GJ, Foltz DR, Cleveland DW. Lethality to human cancer cells through massive chromosome loss by inhibition of the mitotic checkpoint. Proc Natl Acad Sci U S A 2004; 101(23): 8699–704
Grabsch H, Takeno S, Parsons WJ, et al. Overexpression of the mitotic checkpoint genes BUB1, BUBR1, and BUB3 in gastric cancer: association with tumour cell proliferation. J Pathol 2003; 200(1): 16–22
Seike M, Gemma A, Hosoya Y, et al. The promoter region of the human BUBR1 gene and its expression analysis in lung cancer. Lung Cancer 2002; 38(3): 229–34
Lee H, Trainer AH, Friedman LS, et al. Mitotic checkpoint inactivation fosters transformation in cells lacking the breast cancer susceptibility gene, Brca2. Mol Cell 1999; 4(1): 1–10
Rao CV, Yang YM, Swamy MV, et al. Colonice tumorigenesis in BubRl +/t—ApcMin/+ compound mutant mice is linked to premature separation of sister chromatids and enhanced genomic instability. Proc Natl Acad Sci U S A 2005; 102(12): 4365–70
Sudo T, Nitta M, Saya H, et al. Dependence of paclitaxel sensitivity on a functional spindle assembly checkpoint. Cancer Res 2004; 64(7): 2502–8
Cheung HW, Jin DY, Ling MT, et al. Mitotic amaging agent, cisplatin, in nasopharyngeal carcinoma cells. Cancer Res 2005; 65(4): 1450–8
Acknowledgments
Dr Sudakin is an employee of GlaxoSmithKline, which is developing some of the anti-mitotic compounds discussed in this article. Dr Yen is supported by the Leukemia & Lymphoma Society, National Institutes of Health (NIH) grants (no. CA099423, CA06927, and CA75138), and an appropriation from the Commonwealth of Pennsylvania. Dr Yen has no conflicts of interest to declare that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sudakin, V., Yen, T.J. Targeting Mitosis for Anti-Cancer Therapy. BioDrugs 21, 225–233 (2007). https://doi.org/10.2165/00063030-200721040-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00063030-200721040-00003