Abstract
Background
Laparoscopic liver resection (LLR) is increasingly utilized for patients with hepatocellular carcinoma (HCC). However, long-term outcomes for patients requiring conversion to an open procedure during LLR have not been examined.
Methods
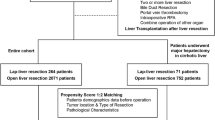
Patients undergoing attempted LLR for HCC were identified within the National Cancer Database. Patients undergoing successful LLR were compared with those who required unplanned conversion with regard to perioperative outcomes and overall survival (OS). Those experiencing conversion were further compared with patients who underwent planned open resection after propensity score matching.
Results
Unplanned conversion occurred in 228 (18.0%) of 1270 patients undergoing LLR. Compared with successful LLR, conversion was associated with greater length of stay (6 vs. 4 days, p < 0.001), higher readmission rates (7.8% vs. 2.6%, p = 0.001), and reduced OS (55.1 vs. 67.6 months, p = 0.074). Unplanned conversion during major hepatectomy was associated with significantly worse OS (median 35.7 months) compared with successful major and minor LLR (median not reached and 67.6 months, respectively, p = 0.004). Compared with planned open resection, similar results were noted as conversion during major LLR was associated with worse OS (median 27.3 months) compared with open major hepatectomy (median not reached; p = 0.002). Unplanned conversion was independently associated with increased mortality (hazard ratio 1.38) after adjustment in a multivariable model. Tumor size was the strongest predictor of conversion on logistic regression analysis.
Conclusions
Unplanned conversion during LLR for HCC is associated with inferior OS. This difference is most pronounced for major hepatectomy. LLR should be considered cautiously in patients with larger, more advanced tumors likely to require major resection.


Similar content being viewed by others
References
Belli G, Limongelli P, Fantini C, et al. Laparoscopic and open treatment of hepatocellular carcinoma in patients with cirrhosis. Br J Surg. 2009;96(9):1041–8. https://doi.org/10.1002/bjs.6680.
Dagher I, Belli G, Fantini C, et al. Laparoscopic hepatectomy for hepatocellular carcinoma: a European experience. J Am Coll Surg. 2010;211(1):16–23. https://doi.org/10.1016/j.jamcollsurg.2010.03.012.
Tranchart H, Di Giuro G, Lainas P, et al. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc. 2010;24(5):1170–6. https://doi.org/10.1007/s00464-009-0745-3.
Cherqui D, Laurent A, Tayar C, et al. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease. Ann Surg. 2006;243(4):499–506. https://doi.org/10.1097/01.sla.0000206017.29651.99.
Fancellu A, Rosman AS, Sanna V, et al. Meta-analysis of trials comparing minimally-invasive and open liver resections for hepatocellular carcinoma. J Surg Res. 2011;171(1):e33–45. https://doi.org/10.1016/j.jss.2011.07.008.
Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261(4):619–29. https://doi.org/10.1097/sla.0000000000001184.
Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection—2,804 patients. Ann Surg. 2009;250(5):831–41. https://doi.org/10.1097/sla.0b013e3181b0c4df.
Berardi G, Van Cleven S, Fretland ÅA, et al. Evolution of laparoscopic liver surgery from innovation to implementation to mastery: perioperative and oncologic outcomes of 2,238 patients from 4 European Specialized Centers. J Am Coll Surg. 2017;225(5):639–49. https://doi.org/10.1016/j.jamcollsurg.2017.08.006.
Dagher I, OʼRourke N, Geller DA, et al. Laparoscopic major hepatectomy. Ann Surg. 2009;250(5):856–60. https://doi.org/10.1097/sla.0b013e3181bcaf46.
Dagher I, Gayet B, Tzanis D, et al. International experience for laparoscopic major liver resection. J Hepatobiliary Pancreat Sci. 2014;21(10):732–6. https://doi.org/10.1002/jhbp.140.
Kasai M, Cipriani F, Gayet B, et al. Laparoscopic versus open major hepatectomy: a systematic review and meta-analysis of individual patient data. Surgery. 2018;163(5):985–95. https://doi.org/10.1016/j.surg.2018.01.020.
Troisi RI, Montalti R, Van Limmen JGM, et al. Risk factors and management of conversions to an open approach in laparoscopic liver resection: analysis of 265 consecutive cases. HPB. 2014;16(1):75–82. https://doi.org/10.1111/hpb.12077.
Stiles ZE, Behrman SW, Glazer ES, et al. Predictors and implications of unplanned conversion during minimally invasive hepatectomy: an analysis of the ACS-NSQIP database. HPB. 2017;19(11):957–65. https://doi.org/10.1016/j.hpb.2017.06.012.
Cauchy F, Fuks D, Nomi T, et al. Risk factors and consequences of conversion in laparoscopic major liver resection. Br J Surg. 2015;102(7):785–95. https://doi.org/10.1002/bjs.9806.
Goh BKP, Chan C-Y, Wong J-S, et al. Factors associated with and outcomes of open conversion after laparoscopic minor hepatectomy: initial experience at a single institution. Surg Endosc. 2015;29(9):2636–42. https://doi.org/10.1007/s00464-014-3981-0.
Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005;12(5):351–5. https://doi.org/10.1007/s00534-005-0999-7.
Halls MC, Cipriani F, Berardi G, et al. Conversion for unfavorable intraoperative events results in significantly worst outcomes during laparoscopic liver resection. Ann Surg. 2017. https://doi.org/10.1097/sla.0000000000002332.
Buell JF, Cherqui D, Geller D, et al. The international position on laparoscopic liver surgery. Ann Surg. 2009;250(5):825–30. https://doi.org/10.1097/sla.0b013e3181b3b2d8.
Komatsu S, Scatton O, Goumard C, et al. Development process and technical aspects of laparoscopic hepatectomy: learning curve based on 15 years of experience. J Am Coll Surg. 2017. https://doi.org/10.1016/j.jamcollsurg.2016.12.037.
van der Poel MJ, Besselink MG, Cipriani F, et al. Outcome and learning curve in 159 consecutive patients undergoing total laparoscopic hemihepatectomy. JAMA Surg. 2016;151(10):923. https://doi.org/10.1001/jamasurg.2016.1655.
Nomi T, Fuks D, Kawaguchi Y, et al. Learning curve for laparoscopic major hepatectomy. Br J Surg. 2015;102(7):796–804. https://doi.org/10.1002/bjs.9798.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
All authors deny conflicts of interest pertinent to this work.
Additional information
Disclaimer: The National Cancer Data Base (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC’s NCDB and the hospitals participating in the CoC NCDB are the source of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Stiles, Z.E., Glazer, E.S., Deneve, J.L. et al. Long-Term Implications of Unplanned Conversion During Laparoscopic Liver Resection for Hepatocellular Carcinoma. Ann Surg Oncol 26, 282–289 (2019). https://doi.org/10.1245/s10434-018-7073-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-018-7073-6