Abstract
Background
Although the prevalence of non-B non-C hepatocellular carcinoma (NBNC HCC) has increased, its clinicopathologic characteristics remain unclear.
Methods
We retrospectively analyzed 518 HCC patients who underwent hepatic resection. Hepatitis B surface antigen- and hepatitis C antibody-negative patients were categorized into the NBNC HCC group (n = 145); others were categorized into the hepatitis B or C HCC (BC HCC) group (n = 373). We subdivided the etiologies of NBNC HCC according to alcohol intake and presence of steatosis.
Results
NBNC HCC was associated with nonalcoholic fatty liver disease (NAFLD) (13.1 %), fatty liver disease with moderate alcohol intake (9.0 %), alcoholic liver disease (ALD) (29.7 %), cryptogenic disease (44.1 %), and other known etiologies (4.1 %). The prevalence of obesity, diabetes mellitus, and hypertension was higher and hepatic function was better in the NBNC HCC group, which had significantly larger tumors than the BC HCC group. The entire NBNC HCC group displayed similar overall and disease-free survival as the BC HCC group. Among the subdivisions, NAFLD-associated HCC patients had significantly better disease-free survival than ALD-associated HCC and BC HCC patients. Microvascular invasion (hazard ratio [HR] 2.30; 95 % confidence interval [CI] 1.33–3.96) and steatosis area <5 % of noncancerous region (HR 2.13; 95 % CI 1.21–3.93) were associated with disease-free survival in NBNC HCC patients.
Conclusions
The prognosis of NBNC HCC was similar to that of BC HCC. Among NBNC HCC patients, NAFLD-associated HCC patients had a relatively low recurrence risk. Absence of steatosis in hepatic parenchyma had a significant impact on disease-free survival in NBNC HCC patients.



Similar content being viewed by others
References
Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet. 2003;362(9399):1907–17.
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics. CA Cancer J Clin. 2010;60(5):277–300.
Zaman SN, Melia WM, Johnson RD, Portmann BC, Johnson PJ, Williams R. Risk factors in development of hepatocellular carcinoma in cirrhosis: prospective study of 613 patients. Lancet. 1985;1(8442):1357–60.
Johnson PJ, Williams R. Cirrhosis and the aetiology of hepatocellular carcinoma. J Hepatol. 1987;4(1):140–7.
Bruix J, Sherman M, Llovet JM, et al. Clinical management of hepatocellular carcinoma. In: Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol. 2001;35(3):421–30.
Ikeda K, Saitoh S, Koida I, et al. A multivariate analysis of risk factors for hepatocellular carcinogenesis: a prospective observation of 795 patients with viral and alcoholic cirrhosis. Hepatology. 1993;18(1):47–53.
Tsukuma H, Hiyama T, Tanaka S, et al. Risk factors for hepatocellular carcinoma among patients with chronic liver disease. N Engl J Med. 1993;328(25):1797–801.
Abe H, Yoshizawa K, Kitahara T, Aizawa R, Matsuoka M, Aizawa Y. Etiology of non-B non-C hepatocellular carcinoma in the eastern district of Tokyo. J Gastroenterol. 2008;43(12):967–74.
Tanaka H, Imai Y, Hiramatsu N, et al. Declining incidence of hepatocellular carcinoma in Osaka, Japan, from 1990 to 2003. Ann Int Med. 2008;148(11):820–6.
Nagaoki Y, Hyogo H, Aikata H, et al. Recent trend of clinical features in patients with hepatocellular carcinoma. Hepatol Res. 2012;42(4):368–75.
Utsunomiya T, Shimada M. Molecular characteristics of non-cancerous liver tissue in non-B non-C hepatocellular carcinoma. Hepatol Res. 2011;41(8):711–21.
Starley BQ, Calcagno CJ, Harrison SA. Nonalcoholic fatty liver disease and hepatocellular carcinoma: a weighty connection. Hepatology. 2010;51(5):1820–32.
Bugianesi E, Leone N, Vanni E, et al. Expanding the natural history of nonalcoholic steatohepatitis: from cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology. 2002;123(1):134–40.
Nair S, Mason A, Eason J, Loss G, Perrillo RP. Is obesity an independent risk factor for hepatocellular carcinoma in cirrhosis? Hepatology. 2002;36(1):150–5.
Siegel AB, Zhu AX. Metabolic syndrome and hepatocellular carcinoma: two growing epidemics with a potential link. Cancer. 2009;115(24):5651–61.
Cauchy F, Zalinski S, Dokmak S, et al. Surgical treatment of hepatocellular carcinoma associated with the metabolic syndrome. Br J Surg. 2013;100(1):113–21.
Suzuki Y, Ohtake T, Nishiguchi S, et al. Survey of non-B, non-C liver cirrhosis in Japan. Hepatol Res. 2013;43(10):1020–31.
Eckel RH, Alberti KG, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2010;375(9710):181–3.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41(6):1313–21.
Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. The French METAVIR Cooperative Study Group. Hepatology. 1994;20(1 Pt 1):15–20.
Kondo R, Nakashima O, Sata M, et al. Pathological characteristics of patients who develop hepatocellular carcinoma with negative results of both serous hepatitis B surface antigen and hepatitis C virus antibody. Hepatol Res. 2014;44(11):1039–46.
Yano Y, Yamashita F, Sumie S, et al. Clinical features of hepatocellular carcinoma seronegative for both HBsAg and anti-HCV antibody but positive for anti-HBc antibody in Japan. Am J Gastroenterol. 2002;97(1):156–61.
Michitaka K, Nishiguchi S, Aoyagi Y, et al. Etiology of liver cirrhosis in Japan: a nationwide survey. J Gastroenterol. 2010;45(1):86–94.
Hamaguchi M, Kojima T, Takeda N, et al. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann Int Med. 2005;143(10):722–8.
Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology. 2005;42(1):44–52.
Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37(4):917–23.
Lok AS, Sterling RK, Everhart JE, et al. Des-gamma-carboxy prothrombin and alpha-fetoprotein as biomarkers for the early detection of hepatocellular carcinoma. Gastroenterology. 2010;138(2):493–502.
Marrero JA, Feng Z, Wang Y, et al. Alpha-fetoprotein, des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology. 2009;137(1):110–8.
Li C, Zhang Z, Zhang P, Liu J. Diagnostic accuracy of des-gamma-carboxy prothrombin versus α-fetoprotein for hepatocellular carcinoma: a systematic review. Hepatol Res. 2014;44(10):E11–25.
Taura N, Ichikawa T, Miyaaki H, et al. Frequency of elevated biomarkers in patients with cryptogenic hepatocellular carcinoma. Med Sci Monit. 2013;19:742–50.
Disclosures
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10434_2014_4181_MOESM3_ESM.tif
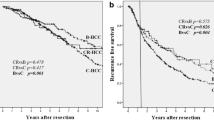
Supplemental Figure 2 Comparisons of overall survival rates among the etiologies. The survival line of other known etiology cases was omitted. Median survival time (MST), 95 % CI, and overall survival rate at 5 years (5-year OS rate), are shown below the graph. Blanks in MST and the upper limit of 95 % CI represent unreached. All groups were compared using the log-rank test; the combinations of groups with p < 0.10 were represented.
10434_2014_4181_MOESM4_ESM.tif
Supplemental Figure 3 Comparisons of disease-free survival rates among the etiologies in patients who underwent curative resection. The survival line of other known etiology cases was omitted. Median survival time (MST), 95 % CI, and disease-free survival rate at 5 years (5-year DFS rate) are shown below the graph. Blanks in MST and the upper limit of 95 % CI represent unreached. All groups were compared using the log-rank test; the combinations of groups with p < 0.10 were represented.
10434_2014_4181_MOESM5_ESM.tif
Supplemental Figure 4 Comparison of disease-free survival rates according to the presence of liver cirrhosis in BC HCC patients who underwent curative resection. Median survival time (MST), 95 % CI, and disease-free survival rate at 5 years (5-year DFS rate) are shown below the graph.
10434_2014_4181_MOESM6_ESM.tif
Supplemental Figure 5 Comparison of disease-free survival rates according to the presence of liver cirrhosis in NBNC HCC patients who underwent curative resection. Median survival time (MST), 95 % CI, and disease-free survival rate at 5 years (5-year DFS rate) are shown below the graph.
10434_2014_4181_MOESM7_ESM.tif
Supplemental Figure 6 Comparison of disease-free survival rates according to the presence of steatosis in NBNC HCC patients who underwent curative resection. Median survival time (MST), 95 % CI, and disease-free survival rate at 5 years (5-year DFS rate) are shown below the graph.
10434_2014_4181_MOESM8_ESM.tif
Supplemental Figure 7 Comparison of disease-free survival rates according to the presence of steatosis in BC HCC patients who underwent curative resection. Median survival time (MST), 95 % CI, and disease-free survival rate at 5 years (5-year DFS rate) are shown below the graph.
Rights and permissions
About this article
Cite this article
Nishio, T., Hatano, E., Sakurai, T. et al. Impact of Hepatic Steatosis on Disease-Free Survival in Patients with Non-B Non-C Hepatocellular Carcinoma Undergoing Hepatic Resection. Ann Surg Oncol 22, 2226–2234 (2015). https://doi.org/10.1245/s10434-014-4181-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-4181-9