Abstract
Background
The histology of epithelial “borderline lesions” of the breast, which have features in between atypical ductal hyperplasia (ADH) and ductal carcinoma in situ (DCIS), is well described, but the clinical behavior is not. This study reports subsequent ipsilateral breast events (IBE) in patients with borderline lesions compared with those with DCIS.
Methods
Patients undergoing breast-conserving surgery for borderline lesions or DCIS from 1997 to 2010 were identified from a prospective database. IBE was defined as the diagnosis of subsequent ipsilateral DCIS or invasive ductal carcinoma.
Results
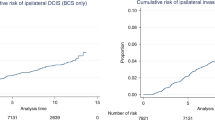
A total of 143 borderline-lesion patients and 2,328 DCIS patients were identified. Median follow-up was 2.9 and 4.4 years, respectively. 7 borderline-lesion and 172 DCIS patients experienced an IBE. 5 year IBE rates were 7.7 % for borderline lesions and 7.2 % for DCIS (p = .80). 5 year invasive IBE rates were 6.5 and 2.8 %, respectively (p = .25). Similarly, when analyses were restricted to patients who did not receive radiotherapy, or endocrine therapy, or both, borderline-lesion and DCIS patients did not demonstrate statistically significant differences in rates of IBE or invasive IBE.
Conclusions
When compared with DCIS, borderline lesions do not demonstrate lower rates of IBE or invasive IBE. Despite “borderline” histology, a 5 year IBE rate of 7.7 % and an invasive IBE rate of 6.5 % suggest that the risk of future carcinoma is significant and similar to that of DCIS.




Similar content being viewed by others
References
Page DL, Dupont WD, Rogers LW, Rados MS. Atypical hyperplastic lesions of the female breast. A long-term follow-up study. Cancer. 1985;55:2698–708.
Page DL. Cancer risk assessment in benign breast biopsies. Hum Pathol. 1986;17:871–4.
Page DL, Dupont WD, Rogers LW. Ductal involvement by cells of atypical lobular hyperplasia in the breast: a long-term follow-up study of cancer risk. Hum Pathol. 1988;19:201–7.
Rosai J. Borderline epithelial lesions of the breast. Am J Surg Pathol. 1991;15:209–21.
Page DL, Rogers LW. Combined histologic and cytologic criteria for the diagnosis of mammary atypical ductal hyperplasia. Hum Pathol. 1992;23:1095–7.
Masood S, Rosa M. Borderline breast lesions: diagnostic challenges and clinical implications. Adv Anat Pathol. 2011;18:190–8.
Rosen PP. “Borderline” breast lesions. Am J Surg Pathol. 1991;15:1100–2.
Dupont WD, Page DL. Risk factors for breast cancer in women with proliferative breast disease. N Engl J Med. 1985;312:146–51.
Dupont WD, Parl FF, Hartmann WH, Brinton LA, Winfield AC, Worrell JA, et al. Breast cancer risk associated with proliferative breast disease and atypical hyperplasia. Cancer. 1993;71:1258–65.
Page DL, Dupont WD. Anatomic markers of human premalignancy and risk of breast cancer. Cancer. 1990;66:1326–35.
Hartmann LC, Sellers TA, Frost MH, Lingle WL, Degnim AC, Ghosh K, et al. Benign breast disease and the risk of breast cancer. N Engl J Med. 2005;353:229–37.
Marshall LM, Hunter DJ, Connolly JL, Schnitt SJ, Byrne C, London SJ, et al. Risk of breast cancer associated with atypical hyperplasia of lobular and ductal types. Cancer Epidemiol Biomarkers Prev. 1997;6:297–301.
Fisher B, Costantino JP, Wickerham DL, Cecchini RS, Cronin WM, Robidoux A, et al. Tamoxifen for the prevention of breast cancer: current status of the National Surgical Adjuvant Breast and Bowel Project P-1 study. J Natl Cancer Inst. 2005;97:1652–62.
Schnitt SJ, Collins LC. Pathology of benign breast disorders. In: Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Diseases of the Breast. Philadelphia, PA: Lippincott Williams & Wilkins; 2010:71.
Schnitt SJ, Connolly JL, Tavassoli FA, Fechner RE, Kempson RL, Gelman R, et al. Interobserver reproducibility in the diagnosis of ductal proliferative breast lesions using standardized criteria. Am J Surg Pathol. 1992;16:1133–43.
Allred DC, Anderson SJ, Paik S, Wickerham DL, Nagtegaal ID, Swain SM, et al. Adjuvant tamoxifen reduces subsequent breast cancer in women with estrogen receptor-positive ductal carcinoma in situ: a study based on NSABP protocol B-24. J Clin Oncol. 2012;30:1268–73.
Hwang ES, Samli B, Tran KN, Rosen PP, Borgen PI, Van Zee KJ. Volume of resection in patients treated with breast conservation for ductal carcinoma in situ. Ann Surg Oncol. 1998;5:757–63.
Van Zee KJ, Liberman L, Samli B, Tran KN, McCormick B, Petrek JA, et al. Long term follow-up of women with ductal carcinoma in situ treated with breast-conserving surgery: the effect of age. Cancer. 1999;86:1757–67.
Bijker N, Meijnen P, Peterse JL, Bogaerts J, Van Hoorebeeck I, Julien JP, et al. Breast-conserving treatment with or without radiotherapy in ductal carcinoma-in situ: ten-year results of European Organisation for Research and Treatment of Cancer randomized phase III trial 10853–a study by the EORTC Breast Cancer Cooperative Group and EORTC Radiotherapy Group. J Clin Oncol. 2006;24:3381–7.
Hughes LL, Wang M, Page DL, Gray R, Solin LJ, Davidson NE, et al. Local excision alone without irradiation for ductal carcinoma in situ of the breast: a trial of the Eastern Cooperative Oncology Group. J Clin Oncol. 2009;27:5319–24.
Rudloff U, Jacks LM, Goldberg JI, Wynveen CA, Brogi E, Patil S, et al. Nomogram for predicting the risk of local recurrence after breast-conserving surgery for ductal carcinoma in situ. J Clin Oncol. 2010;28:3762–9.
Ho A, Goenka A, Ishill N, Van Zee K, McLane A, Gonzales AM, et al. The effect of age in the outcome and treatment of older women with ductal carcinoma in situ. Breast. 2011;20:71–7.
Wapnir IL, Dignam JJ, Fisher B, Mamounas EP, Anderson SJ, Julian TB, et al. Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS. J Natl Cancer Inst. 2011;103:478–88.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Choi, D.X., Eaton, A.A., Olcese, C. et al. Blurry Boundaries: Do Epithelial Borderline Lesions of the Breast and Ductal Carcinoma In Situ Have Similar Rates of Subsequent Invasive Cancer?. Ann Surg Oncol 20, 1302–1310 (2013). https://doi.org/10.1245/s10434-012-2719-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-012-2719-2