Abstract
Background
Mucormycosis is a rare and life-threatening invasive fungal infection. Pulmonary mucormycosis commonly occurs in patients with severe neutropenia. Typically, pulmonary mucormycosis causes tissue necrosis resulting from angioinvasion and subsequent thrombosis, so most cases can occur with necrotizing pneumonia and/or hemoptysis. Some complex cases may invade adjacent organs, such as the mediastinum, pericardium, and chest wall. However, to the best our knowledge there is little known regarding bronchoesophageal fistula due to pulmonary mucormycosis after induction chemotherapy for acute myeloid leukemia. We present a case report about this unusual presentation.
Case presentation
A 51-year-old Korean man was diagnosed as having acute myeloid leukemia and received induction chemotherapy. After prolonged severe neutropenia, he complained of coughing with aspiration. Imaging showed a bronchoesophageal fistula with extensive necrotizing pneumonia in the middle and lower lobes of his right lung. Bronchoscopy showed near total tissue necrosis in the middle lobe of his right lung, creating an orifice. A bronchial scope was passed through and was able to be connected with his esophagus; a bronchial wall biopsy was performed. Esophagoscopy revealed a large linear defect of his esophageal wall 30 cm from the incision that may have connected with the bronchus. A bronchial biopsy showed typical hyphae with necrotic tissue, indicating pulmonary mucormycosis. He was given amphotericin B, and a wide excision of lung and esophagus was planned. However, he suddenly died due to massive hemoptysis.
Conclusion
Here we present an extremely rare case of bronchoesophageal fistula with severe necrotizing pneumonia due to pulmonary mucormycosis.
Similar content being viewed by others
Background
Chemotherapy-induced immunosuppression has led to an increase in the incidence of fungal infections. Mucormycosis is a rare and life-threatening invasive fungal infection caused by fungi of the Zygomycetes class and Mucorales order. Pulmonary mucormycosis commonly occurs during chemotherapy-induced neutropenia often associated with hematologic malignancy and usually progresses rapidly [1–3].
Case presentation
A 51-year-old Korean man was diagnosed as having acute myeloid leukemia (acute myelomonocytic leukemia, M4) with normal karyotype (46,XY). An initial complete blood count (CBC) showed a white blood cell (WBC) count of 65.29×109/L, neutrophils 22 %, monocytes 67 %, hemoglobin 8.7 g/dL, and platelet count 18×109/L. He received induction chemotherapy of cytarabine (100 mg/m2 body surface area on days 1 to 7) and idarubicin (12 mg/m2 body surface area on days 1 to 3).
On day 3 of therapy, when his WBC count reached its nadir, and his absolute neutrophil count was 277/mL, filgrastim was immediately started. He had no signs of infection, including fever, coughing, or diarrhea.
On day 13 of chemotherapy, he developed a neutropenic fever and complained of right pleuritic chest pain with productive coughing and sticky sputum. A chest X-ray showed lobar infiltration of the lower lobe of his right lung. Antibiotics were subsequently changed from prophylactic ciprofloxacin to meropenem and vancomycin.
On day 17 of chemotherapy, his neutropenic fever persisted, and a chest X-ray showed increased infiltration of his right lung field with pleural effusion. Laboratory data were as follows: WBC count of 0.31 (103/mm3), neutrophils 51.2 %, lymphocytes 32.2 %, absolute neutrophil count of 150, hemoglobin 7.3 g/dL, platelet count 34 (103/mm3), C-reactive protein 27.1 mg/dL (normal range 0 to 0.5), and procalcitonin 1.74 ng/mL (normal range 0 to 0.5). We performed pleural puncture and pleural fluid examinations. Analysis of his right-side pleural fluid indicated an exudative type. His pleural fluid had a WBC count of 670 (42 % neutrophils), total protein 4.75 g/dL, and lactate dehydrogenase (LDH) 1183 IU/L. The results of pleural galactomannan and acid-fast bacilli tests were negative, but the pleural fluid culture grew Enterococcus faecium that was resistant to vancomycin.
His antibiotic regimen was switched to meropenem and linezolid, and the prophylactic antifungal agent (oral fluconazole) was changed to caspofungin, an empiric therapy, due to the prolonged neutropenia.
On day 19 of the therapy, his WBC count recovered to an absolute neutrophil count of 3360. A bone marrow biopsy was performed to confirm response to induction chemotherapy, and biopsy results indicated complete remission.
Nevertheless, his fever persisted, a chest X-ray showed no change in lung consolidation, and he complained of a cough that became more severe after swallowing.
An esophagram was subsequently performed and revealed an approximately 2 cm filling of a fistula at the mid-esophagus and the right bronchus intermedius (Fig. 1).
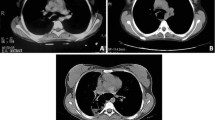
Further evaluations with a chest computed tomography (CT) as well as esophagoscopy and bronchoscopy were recommended. Chest CT imaging showed extensive necrotizing pneumonia of his right lung and bilateral pleural effusion predominantly on the right side. In addition, a small, linear, walled air collection was noted just medial to the bronchus intermedius tracking towards his esophagus, a finding suspicious for a bronchoesophageal fistula (Fig. 2).
a Chest X-ray on the day of admittance. b Chest X-ray on day 17 of therapy showing a newly appearing infiltration of right lung with pleural effusion. c, d Chest computed tomography scan on day 19 of the therapy shows air bronchograms, diffuse consolidation with necrotic low attenuation of right lung (c), and bronchoesophageal fistula (white arrow; d)
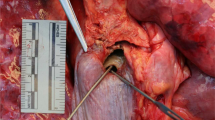
Flexible bronchoscopy showed mucosal hyperemia in his right upper bronchus and brownish extensive tissue necrosis in the middle lobe of his right lung (Fig. 3). Subsequent biopsy and culture were performed.
Esophagoscopy revealed a large linear defect of his esophageal wall 30 cm from the upper incision that perhaps connected with the bronchus (Fig. 4).
A bronchoscopic biopsy showed broad and pleomorphic hyphae with necrotic debris. The hyphae appeared non-septate. Branches arose haphazardly, often at right angles. These findings suggested pulmonary mucormycosis (Fig. 5). Lung tissue was cultured; unfortunately, the specimen was inadequate.
The antifungal agent was changed from caspofungin to liposomal amphotericin B (®AmBisome) at a starting dose of 5 mg/kg daily. A wide excision of his lung and perhaps of his esophagus was planned, as continued consolidation chemotherapy was required to treat the acute myeloid leukemia. However, he suddenly died due to massive hemoptysis. A timeline for our patient is given in Table 1.
Discussion
Mucormycosis is a relatively rare infection compared to species such as Candida and Aspergillus. The prevalence of mucormycosis is estimated at 1.7 cases per million people per year according to one population-based study and has ranged from 1 to 5 cases per 10,000 according to some autopsy studies [4–6]. Mucormycosis is found in 0 to 8.3 % cases of acute leukemia, and the most common pattern of presentation is pulmonary mucormycosis [1, 7, 8].
Both mononuclear and polymorphonuclear phagocytes of normal hosts kill Mucorales by generating oxidative metabolites and cationic peptides known as defensins. The most important conditions predisposing to mucormycosis include hematologic malignancy, stem cell transplantation, prolonged and severe neutropenia, poorly controlled diabetes mellitus with or without diabetic ketoacidosis, iron overload, major trauma, prolonged corticosteroid use, illicit intravenous drug use, neonatal prematurity, and malnourishment [1–3, 9, 10].
Based on the clinical presentation and involvement, mucormycosis can be divided into the following six major clinical forms: (1) rhinocerebral, (2) pulmonary, (3) cutaneous, (4) gastrointestinal, (5) disseminated, and (6) uncommon rare manifestations, such as endocarditis, osteomyelitis, peritonitis, and renal infection. Among them, pulmonary mucormycosis occurs most often in patients with neutropenia undergoing chemotherapy or stem cell transplantation [11, 12].
The clinical signs and symptoms of pulmonary mucormycosis are nonspecific and cannot be easily distinguished from pulmonary aspergillosis. It usually presents with necrotizing pneumonia, and the symptoms include prolonged high-grade fever and other various findings including cough, chest pain, dyspnea, and hypoxia. In particular, pulmonary mucormycosis results in tissue necrosis due to angioinvasion and subsequent thrombosis; if a major blood vessel is involved, it can lead to hemoptysis. Multiple reports show that in severe cases, it can invade adjacent organs, such as the mediastinum, pericardium, and chest wall [11–15].
The most frequent radiographic findings include infiltration, consolidation, nodules, cavitations, atelectasis, effusion, posterior tracheal band thickening, hilar or mediastinal lymphadenopathy, and even normal findings. However, these findings are indistinguishable from those of pulmonary aspergillosis [16–18]. Therefore, the best mode of diagnosis for pulmonary mucormycosis is bronchoscopic or percutaneous lung biopsy. Ultimately, a confirmatory diagnosis of mucormycosis is based on both: (1) histopathological findings of tissue invasion by hyphae with tissue necrosis resulting from angioinvasion and subsequent thrombosis and 2) cultures isolating pathogens of the order Mucorales [1, 12, 19].
Other than histopathology, there are no biomarkers to identify this disease. Therefore, the high mortality observed in pulmonary mucormycosis may be related to delays in the diagnosis. Another cause of high mortality is rapid progression, extensive involvement, severe underlying conditions, and limited available therapy. The overall mortality rate in pulmonary mucormycosis is high (76 %); it is even higher in severely immunosuppressed patients [1, 12, 20].
Treatment of pulmonary mucormycosis is difficult and often delayed, as described above. Important factors for successful treatment of mucormycosis is rapidity of diagnosis, reversal of the underlying predisposing factor (if possible), appropriate surgical debridement of infected tissue, and appropriate antifungal therapy. Small focal lesions can often be surgically excised before they disseminate or progress to involve critical structures. The only recommended antifungal agents are members of the polyene class, including amphotericin B deoxycholate and its lipid derivatives.
Therefore, the main treatment for pulmonary mucormycosis is immediate surgical resection of the infected tissue, followed by administration of amphotericin B [21–24].
Typically, an esophagopulmonary fistula may occur as a complication of infectious disorders, foreign body ingestion, a complication of intubation with cuff-related tracheal injury, cancer, or congenital anomalies. Pulmonary mucormycosis may invade organs adjacent to the lungs, such as the mediastinum, pericardium, chest wall, or even the esophagus. However, to the best of our knowledge, little is known regarding bronchoesophageal fistula due to pulmonary mucormycosis [25–28].
Conclusions
Esophagopulmonary fistula is a rare but serious condition. It can occur as a complication of infections but, to the best of our knowledge, there has been no case report of bronchoesophageal fistula due to pulmonary mucormycosis. This is the first case report of such an unusual presentation.
Abbreviations
CBC, complete blood count; CT, computed tomography; LDH, lactate dehydrogenase; WBC, white blood cell
References
Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, et al. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634–53.
Spellberg B, Edwards Jr J, Ibrahim A. Novel perspectives on mucormycosis: pathophysiology, presentation, and management. Clin Microbiol Rev. 2005;18:556–69.
Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev. 2000;13:236–301.
Rees JR, Pinner RW, Hajjeh RA, Brandt ME, Reingold AL. The epidemiological features of invasive mycotic infections in the San Francisco Bay area, 1992–1993: results of population-based laboratory active surveillance. Clin Infect Dis. 1998;27:1138–47.
Yamazaki T, Kume H, Murase S, Yamashita E, Arisawa M. Epidemiology of visceral mycoses: analysis of data in annual of the pathological autopsy cases in Japan. J Clin Microbiol. 1999;37:1732–8.
Rüping MJ, Heinz WJ, Kindo AJ, Rickerts V, Lass-Flörl C, Beisel C, et al. Forty-one recent cases of invasive mucormycosis from a global clinical registry. J Antimicrob Chemother. 2010;65:296–302.
Nosari A, Oreste P, Montillo M, Carrafiello G, Draisci M, Muti G, et al. Mucormycosis in hematologic malignancies: an emerging fungal infection. Haematologica. 2000;85:1068–71.
Pagano L, Caira M, Candoni A, Offidani M, Fianchi L, Martino B, et al. The epidemiology of fungal infections in patients with hematologic malignancies: the SEIFEM-2004 study. Haematologica. 2006;91:1068–75.
Diamond RD, Haudenschild CC, Erickson 3rd NF. Monocyte-mediated damage to Rhizopus oryzae hyphae in vitro. Infect Immun. 1982;38:292–7.
Ibrahim AS, Spellberg B, Avanessian V, Fu Y, Edwards Jr JE. Rhizopus oryzae adheres to, is phagocytosed by, and damages endothelial cells in vitro. Infect Immun. 2005;73:778–83.
Hamillos G, Samonis G, Kontoyiannis DP. Pulmonary mucormycosis. Semin Respir Crit Care Med. 2011;32:693–702.
Lee FY, Mossad SB, Adal KA. Pulmonary mucormycosis: the last 30 years. Arch Intern Med. 1999;159:1301–9.
Harada M, Manabe T, Yamashita K, Okamoto N. Pulmonary mucormycosis with fatal massive hemoptysis. Acta Pathol Jpn. 1992;42:49–55.
Watts WJ. Bronchopleural fistula followed by massive fatal hemoptysis in a patient with pulmonary mucormycosis. A case report. Arch Intern Med. 1983;143:1029–30.
Connor BA, Anderson RJ, Smith JW. Mucor mediastinitis. Chest. 1979;75:525–6.
Hsu JW, Chiang CD. A case report of novel roentgenographic finding in pulmonary mucormycosis: thickening of the posterior tracheal band. Kaohsiung J Med Sci. 1996;12:595–600.
McAdams HP, Rosado de Christenson M, Strollo DC, Patz Jr EF. Pulmonary mucormycosis: radiologic findings in 32 cases. Am J Roentgenol. 1997;168:1541–8.
Chamilos G, Marom EM, Lewis RE, Lionakis MS, Kontoyiannis DP. Predictors of pulmonary mucormycosis versus invasive pulmonary aspergillosis in patients with cancer. Clin Infect Dis. 2005;41:60–6.
Wahidi MM, Rocha AT, Hollingsworth JW, Govert JA, Feller-Kopman D, Ernst A. Contraindications and safety of transbronchial lung biopsy via flexible bronchoscopy. A survey of pulmonologists and review of the literature. Respiration. 2005;72:285–95.
Fernandez JF, Maselli DJ, Simpson T, Restrepo MI. Pulmonary mucormycosis: what is the best strategy for therapy? Respir Care. 2013;58:e60–3.
Gleissner B, Schilling A, Anagnostopolous I, Siehl I, Thiel E. Improved outcome of zygomycosis in patients with hematological diseases? Leuk Lymphoma. 2004;45:1351–60.
Asai K, Suzuki K, Takahashi T, Ito Y, Kazui T, Kita Y. Pulmonary resection with chest wall removal and reconstruction for invasive pulmonary mucormycosis during antileukemia chemotherapy. Jpn J Thorac Cardiovasc Surg. 2003;51:163–6.
Pavie J, Lafaurie M, Lacroix C, Marie Zagdanski A, Debrosse D, Socié G, et al. Successful treatment of pulmonary mucormycosis in an allogenic bone-marrow transplant recipient with combined medical and surgical therapy. Scand J Infect Dis. 2004;36:767–9.
Reid VJ, Solnik DL, Daskalakis T, Sheka KP. Management of bronchovascular mucormycosis in a diabetic: a surgical success. Ann Thorac Surg. 2004;78:1449–51.
Burt M, Diehl W, Martini N, Bains MS, Ginsberg RJ, McCormack PM, et al. Malignant esophagorespiratory fistula: management options and survival. Ann Thorac Surg. 1991;52:1222–8.
Rodriguez AN, Diaz-Jimenez JP. Malignant respiratory-digestive fistulas. Curr Opin Pulm Med. 2010;16:329–33.
Deshpande G, Samarasam I, Banerjee S, Gnanamuthu RB, Chandran S, Mathew G. Benign esophagorespiratory fistula: a case series and a novel technique of definitive management. Dis Esophagus. 2013;26:141–7.
Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am. 2003;13:271–89.
Acknowledgements
None.
Funding
Not applicable.
Availability of data and materials
The dataset(s) supporting the conclusions of this article is (are) available in the figshare repository in https://figshare.com/account/home#/data.
Authors’ contributions
JHL was the major contributor in writing the manuscript. JSH, DYK, and HJL did the literature search and data collection. SGP conducted study design and reviewed the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lee, JH., Hyun, JS., Kang, Dy. et al. Rare complication of bronchoesophageal fistula due to pulmonary mucormycosis after induction chemotherapy for acute myeloid leukemia: a case report. J Med Case Reports 10, 195 (2016). https://doi.org/10.1186/s13256-016-0991-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-016-0991-7