Abstract
Background
Immunotherapy has demonstrated encouraging clinical benefits in patients with advanced breast carcinomas and Programmed death ligand 1 (PD-L1) expression has been proposed as an immunotherapy biomarker. Challenges with current PD-L1 testing exist and tumor mutation burden (TMB) is emerging as a biomarker to predict clinical response to immunotherapy in melanoma and non-small cell lung cancer patients. However, TMB has not been well characterized in breast carcinomas.
Methods
The study cohort included 62 advanced breast cancer patients (13 primary and 49 metastatic). Genetic alterations and TMB were determined by FoundationOne CDx next generation sequencing (NGS) and the association with clinicopathologic features was analyzed.
Results
High TMB was observed in a relatively low frequency (3/62, 4.8%). TMB levels were positively associated tumor infiltrating lymphocytes and significantly higher TMB was observed in breast carcinomas with DNA damage repair gene mutation(s). There was no significant association between TMB levels and other analyzed clinicopathologic characteristics.
Conclusions
Our data indicate the importance of DNA damage repair proteins in maintaining DNA integrity and immune reaction and breast carcinoma patients with DDR mutation may benefit from immunotherapy.
Similar content being viewed by others
Introduction
Breast cancer (BC) is the most common malignancy in women [1] and biomarkers including estrogen receptor (ER)s, progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2), are routinely performed for therapeutic decision-making [2]. Although anti-hormonal and anti-HER2 targeted therapies are available for a large percentage of BC patients, up to 30% BC patients develop advanced disease during their disease courses [3, 4]. The lack/loss of efficacy of targeted therapies and the relatively poor prognosis of advanced BC patients have created the need to evaluate novel treatment approaches, including immunotherapy [5,6,7]. Recent studies have demonstrated pembrolizumab and atezolizumab plus nab-paclitaxel have demonstrated encouraging clinical benefits in patients with advanced triple negative BC [5, 6]. Although Programmed death ligand 1 (PD-L1) expression has been proposed as a biomarker for immunotherapy, challenges with PD-L1 testing exist, including interassay variability among different PD-L1 immunohistochemistry (IHC) assays with different reagents and platforms, lack of standardization among different PD-L1 IHC assays, and even interobserver variability in interpreting PD-L1 IHCs [8,9,10,11,12].
Tumor mutation burden (TMB) is defined as the total number of somatic mutations in a region of tumor genome and is associated with the immunogenicity of many different tumors, including BC [13, 14]. TMB is emerging as potential biomarker for immunotherapy decisions in melanoma or non-small lung cancer patients [15,16,17,18,19,20,21,22,23]; however, TMB has not been well characterized in BCs. Whole exome sequencing is the standard method to determine TMB, but it is time consuming and too expensive for routine clinical practice. Recently, commercially available cancer gene panels, such as FoundationOne CDx, have been shown to have similar accuracy in determining TMB and similar ability to predict outcomes to immunotherapy [13, 21, 24, 25]. In this study, we aimed to investigate TMB in BCs using FoundationOne CDx NGS and its association with different clinicopathologic features including histologic types, hormone receptor and HER2 status, and different genetic mutations.
Methods
Patients and specimens
The study cohort included 62 advanced breast cancer patients (13 primary and 49 metastatic) within a study period between January 2014 and June 2018. The specimens from these patients were sent to Foundation Medicine (Cambridge, MA) for analyzing genetic alterations and TMB by FoundationOne CDx next generation sequencing (NGS) (Foundation Medicine, Cambridge, MA). This study was approved by the Ohio State University institutional Research Board. Clinicopathologic characteristics were collected and breast cancer biomarkers (ER, PR, and HER2) were evaluated by breast subspecialized pathologists, with manual quantification [ER: clone SP1 (Spring, Pleasanton, CA), PR: clone PgR 636 (DAKO, Carpinteria, CA), HER2: 4B5 clone (Ventana, Tucson, AZ)].
Analyzing genetic alterations and tumor mutation burden by FoundationOne CDx NGS
Genetic alterations were determined by FoundationOne CDx NGS performed at Foundation Medicine and the results were extracted from FoundationOne CDx reports. TMB was also determined by FoundationOne CDx as the number of somatic, coding base substitutions and short insertions and deletions per megabase of tumor genome examined [13]. TMB levels are divided into three groups on FoundationOne CDx reports, including low TMB (1–5 muts/mb), intermediate TMB (6–19 muts/mb), and high TMB (≥ 20 muts/mb).
Evaluating tumor infiltrating lymphocytes (TILs)
At Ohio State University, all slides from tumor cases had been digitally scanned (Philips Intel-liSite). Representative digital slides from our cohort except 5 cytology cases were reviewed with the Philips Digital Pathology Solutions viewer and TILs were scored as a percentage by reviewing the slides at 50x, 100x, and 200x magnifications.
DNA damage repair gene mutation analysis
Thirty-four DNA damage repair (DDR) genes are included in FoundationOne CDx NGS and analyzed for genetic alterations. These genes belongs several DDR canonical pathways including nucleotide excision repair (NER), mismatch repair (MMR), Fanconi Anemia (FA), homologous recombination (HR), checkpoint and others [26]. (Table 1).
Statistical analysis
All clinicopathologic variables were summarized using percentages and descriptive statistics (mean, range, frequencies). T test was used to compare the continuous values among different groups. Statistics were performed using SAS version 9.3 (SAS Institute Inc., Cary, North Carolina). For all results, a P-value of < 0.05 was considered significant.
Results
The demographic features of study cohort
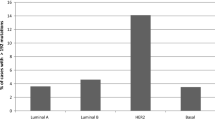
The average age of the patient’s studied in this cohort was 53.8 years old (range 30–78). The majority of specimens were from metastatic locations (49, 79.0%) because FoundationOne CDx was ordered mostly in patients with advanced stage disease. Fifty-two (83.9%) cases were invasive ductal carcinoma (IDC), 6 (9.7%) were invasive lobular carcinoma, 2 (3.2%) were metaplastic carcinoma, and 2 (3.2%) were neuroendocrine carcinomas. As for breast cancer biomarkers, 36 (58.1%) were ER positive, 38 (61.3%) were PR positive, 5 (8.1%) were HER2 positive, and 22 (35.5%) were triple negative. Among 62 cases, 3 (4.8%) had high TMB, 27 (43.6%) had intermediate TMB, and the remaining 32 (51.6%) had low TMB. Due to the rarity of high TMB, cases with high and intermediate TMB were grouped together and compared with cases with low TMB regarding to their clinicopathologic features. The group of cases with intermediate or high TMB showed significantly increased TILs than the group of cases with low TMB (p = 0.0018). In addition, a moderate correlation between TMB and TILs was identified by the Pearson correlation analysis with a coefficient (r) of 0.80696 (n = 57, P < .0001, y = 0.9177x + 0.3697, R2 = 0.6512). (Fig. 1) There was no significant association between TMB levels and other analyzed clinicopathologic characteristics, including biomarker status, histologic types and tumor nuclear grade. (Table 2).
The most common gene mutation identified among 62 cases was TP53 (59.7%) followed by PIK3CA (33.9%). Interestingly, of the 6 BCs with BRCA (1/2) mutations analyzed, 5 of them had intermediate or high TMB, while only one case showed low TMB (p = 0.0002). (Table 2) The association between TMB and DNA damage repair pathway.
Thirty-four DDR genes are included in FoundationOne CDx NGS panel and analyzed for genetic alterations. Thirteen cases showed at least one DDR gene mutation and the remaining 49 cases did not show any DDR gene mutation. Clinicopathologic features and TMB were analyzed between DDR mutated and non-DDR mutated cases. BCs harboring DDR mutation(s) averaged a higher TMB compared to those without DDR mutation (12.08 average mutations vs. 6.57; p = 0.043). No significant difference was found in other analyzed clinicopathologic characteristics between DDR mutated and non-DDR mutated cases. (Table 3).
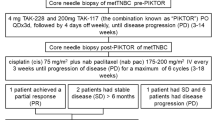
Cases with high TMB (≥ 20) harbored either MAGI2 or PTEN genetic mutations
Three cases had high TMB, including 2 invasive ductal carcinomas and one invasive lobular carcinoma. All three cases showed high expression of ER but were negative for PR and HER2. All three cases showed prominent tumoral lymphocytic infiltrates (Fig. 2). Of these three cases, two harbored MAGI2 mutations and one harbored a PTEN mutation. The two MAGI2 mutations were MAGI2 S220* and MAGI2 Q1193fs*35. (Table 4).
Discussion
Immunotherapy has demonstrated encouraging clinical benefits in advanced BC patients and PD-L1 IHC testing has been used to select eligible patients for such therapy [5]. However, challenges with current PD-L1 testing do exist, such as interassay variability and interobserver variability [11, 12]. Tumors with high TMB are associated with significant clinical benefit to immunotherapy in melanoma and non-small cell lung cancer patients [22, 27, 28]. TMB levels are very different among different tumors and such information is lacking in BCs [13]. In this study, we investigated TMB in 62 BCs determined by FoundationOne CDx assay and found a relatively low percentage of BCs with a high TMB level (3/62, 4.8%), consistent with previous study [13], but no association of TMB levels with any of the analyzed clinicopathologic characteristics was identified, such as age, histologic types and other biomarkers (ER, PR and HER2).
Tumors with deficient mismatch repair (dMMR) or microsatellite instability (MSI) have shown a high TMB level [13, 29,30,31] and patients with dMMR and MSI-high tumor have benefited from immunotherapy [32,33,34,35]. Tumors with DNA polymerase epsilon (POLE) mutation also have high TMB level [36]. While tumors with POLE mutation, dMMR, or high MSI show high TMB level, the reverse is not always true. For example, melanoma and non-small cell lung carcinomas frequently have high TMB but dMMR, MSI-high or POLE mutations are rare in these tumors [37,38,39], indicating other mechanisms can contribute to increased TMB [13, 32, 36, 40]. Previously, we and others have demonstrated the frequency of dMMR is very low in breast carcinomas [41,42,43]. In current study, significantly higher TMB was observed in breast cancers with DNA damage repair gene mutation(s) or BRCA (1/2) gene mutation, suggesting the importance of DNA damage repair proteins in maintaining DNA integrity and immune reaction. Tumors with DDR mutations generally represent a triple negative phenotype, higher tumor grade and other aggressive features. However, no such correlation was identified in tumors with DDR mutation. This would be caused by the low number of the cases tested in current cohort, thus, further studies with larger cohorts would be warranted.
Current cohort included two metaplastic carcinomas, one with a TMB value of 6 muts/Mb and the other one with a TMB value of 3 muts/Mb. Although the metaplastic carcinoma case number is very small, the findings of low TMB in these metaplastic carcinomas are consistent with a recent study which reported that the metaplastic carcinomas consistently expressed a low TMB of between 3 and 10 muts/Mb. In addition, two neuroendocrine carcinomas of our cohort also showed low TMB values, consistent with a previous study demonstrating neuroendocrine carcinomas of the breast tend to have low TMB [44].
In our study, three cases had high TMB and all showed prominent tumoral lymphocytic infiltrates, suggesting the association between TMB and immune reaction. Furthermore, of the three cases with high TMB, two harbored MAGI2 mutations and one harbored a PTEN mutation. MAGI2 was initially characterized as a scaffolding protein that links cell adhesion molecules and receptors to cytoskeleton and maintains the architecture of cell junctions [45]. Further studies have revealed that MAGI2 promotes PTEN (tumor suppressor) function to regulate several kinase signaling pathways [46,47,48]. Additionally, MAGI2 is abnormally expressed in high grade prostatic intraepithelial neoplasia and prostate cancer compared to benign glandular epithelium [49,50,51,52,53]. In a recent study, glioblastoma patients who were not responsive to anti-PD-1 immunotherapy were significantly enriched for PTEN mutations and these PTEN mutations may induce a distinct immunosuppressive microenvironment, suggesting PTEN mutations’ involvement in immune reaction regualtion [54]. PTEN gene mutations are not uncommonly observed in many solid tumors, and are associated with immune suppression. In addition, loss of PTEN expression is correlated with up-regulation of PD-L1 in tumor cells and causes alteration in the tumor microenvironment, such as release of anti-inflammatory cytokines and significant reduction of T-cell activity [55]. Our findings of MAGI2 mutation in breast carcinoma with high TMB warrant future study to investigate MAGI2’s function in DNA repair pathway and PTEN signaling pathway.
Although this is one of the first studies to investigate TMB and its association with clinicopathologic features and genetic alterations in breast carcinomas, the significance of this study was limited by the small sample cohort (n = 62). The findings in current study need to be confirmed by future studies with larger cohort.
In conclusion, our data has demonstrated TMB levels were positively associated with TILs, but not any other analyzed clinicopathologic characteristics including breast cancer biomarker status, tumor histologic type and tumor nuclear grade. In addition, significantly higher TMB was observed in breast cancers with DNA damage repair gene mutation(s) or BRCA (1/2) gene mutation, suggesting the importance of DNA damage repair proteins in maintaining DNA integrity and immune reaction and breast cancer patients with DDR mutation may benefit from immunotherapy.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee.
Abbreviations
- PD-L1:
-
Programmed death ligand 1
- TMB:
-
Tumor mutation burden
- NGS:
-
Next generation sequencing
- BC:
-
Breast cancer
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- HER2:
-
Human epidermal growth factor receptor 2
- IHC:
-
Immunohistochemistry
- DDR:
-
DNA damage repair gene (DDR)
- NER:
-
Nucleotide excision repair
- MMR:
-
Mismatch repair
- FA:
-
Fanconi Anemia
- HR:
-
Homologous recombination
References
Howlader N NA, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA. SEER Cancer Statistics Review, 1975–2016, National Cancer Institute. https://seercancer.gov/csr/1975_2016/ 2019.
Duffy MJ, Walsh S, McDermott EW, Crown J. Biomarkers in breast Cancer: where are we and where are we going? Adv Clin Chem. 2015;71:1–23.
Mariotto AB, Etzioni R, Hurlbert M, Penberthy L, Mayer M. Estimation of the number of women living with metastatic breast Cancer in the United States. Cancer epidemiology biomarkers &. Prevention. 2017;26:809–15.
Gobbini E, Ezzalfani M, Dieras V, et al. Time trends of overall survival among metastatic breast cancer patients in the real-life ESME cohort. Eur J Cancer. 2018;96:17–24.
Schmid P, Adams S, Rugo HS, et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast Cancer. N Engl J Med. 2018;379:2108–21.
Nanda R, Chow LQ, Dees EC, et al. Pembrolizumab in patients with advanced triple-negative breast Cancer: phase Ib KEYNOTE-012 study. J Clin Oncol. 2016;34:2460–7.
Adams S, Schmid P, Rugo HS, et al. Pembrolizumab monotherapy for previously treated metastatic triple-negative breast cancer: cohort a of the phase II KEYNOTE-086 study. Ann Oncol. 2019;30:397–404.
Hersom M, Jorgensen JT. Companion and complementary diagnostics-focus on PD-L1 expression assays for PD-1/PD-L1 checkpoint inhibitors in non-small cell lung Cancer. Ther Drug Monit. 2018;40:9–16.
Kim JM, Chen DS. Immune escape to PD-L1/PD-1 blockade: seven steps to success (or failure). Ann Oncol. 2016;27:1492–504.
Buttner R, Gosney JR, Skov BG, et al. Programmed death-ligand 1 immunohistochemistry testing: a review of analytical assays and clinical implementation in non-small-cell lung Cancer. J Clin Oncol. 2017;35:3867–76.
Rimm DL, Han G, Taube JM, et al. Reanalysis of the NCCN PD-L1 companion diagnostic assay study for lung cancer in the context of PD-L1 expression findings in triple-negative breast cancer. Breast Cancer Res. 2019;21:72.
Rimm DL, Han G, Taube JM, et al. A prospective, multi-institutional, pathologist-based assessment of 4 immunohistochemistry assays for PD-L1 expression in non–small cell lung CancerAssessment of 4 assays for PD-L1 expression in NSCLCAssessment of 4 assays for PD-L1 expression in NSCLC. JAMA Oncol. 2017;3:1051–8.
Chalmers ZR, Connelly CF, Fabrizio D, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 2017;9:34.
Schumacher TN, Schreiber RD. Neoantigens in cancer immunotherapy. Science. 2015;348:69–74.
Snyder A, Makarov V, Merghoub T, et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 2014;371:2189–99.
Rizvi N, Hellmann M, Snyder A, et al. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–8.
Hellmann MD, Paz-Ares L. Lung Cancer with a high tumor mutational burden. N Engl J Med. 2018;379:1093–4.
Offin M, Rizvi H, Tenet M, et al. Tumor mutation burden and efficacy of EGFR-tyrosine kinase inhibitors in patients with EGFR-mutant lung cancers. Clin Cancer Res. 2019;25:1063–9.
Rizvi H, Sanchez-Vega F, La K, et al. Molecular determinants of response to anti-programmed cell death (PD)-1 and anti-programmed death-ligand 1 (PD-L1) blockade in patients with non-small-cell lung Cancer profiled with targeted next-generation sequencing. J Clin Oncol. 2018;36:633–41.
Hellmann MD, Nathanson T, Rizvi H, et al. Genomic Features of Response to Combination Immunotherapy in Patients with Advanced Non-Small-Cell Lung Cancer. Cancer Cell. 2018;33:843–52 e4.
Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus Ipilimumab in lung Cancer with a high tumor mutational burden. N Engl J Med. 2018;378:2093–104.
Hellmann MD, Callahan MK, Awad MM, et al. Tumor Mutational Burden and Efficacy of Nivolumab Monotherapy and in Combination with Ipilimumab in Small-Cell Lung Cancer. Cancer Cell. 2018;33:853–61 e4.
Yarchoan M, Hopkins A, Jaffee EM. Tumor mutational burden and response rate to PD-1 inhibition. N Engl J Med. 2017;377:2500–1.
Johnson DB, Frampton GM, Rioth MJ, et al. Targeted next generation sequencing identifies markers of response to PD-1 blockade. Cancer Immunol Res. 2016;4:959–67.
Rosenberg JE, Hoffman-Censits J, Powles T, et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet. 2016;387:1909–20.
Dietlein F, Thelen L, Reinhardt HC. Cancer-specific defects in DNA repair pathways as targets for personalized therapeutic approaches. Trends Genetics. 2014;30:326–39.
Rizvi NA, Hellmann MD, Snyder A, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–8.
Nathanson T, Ahuja A, Rubinsteyn A, et al. Somatic mutations and Neoepitope homology in melanomas treated with CTLA-4 blockade. Cancer Immunol Res. 2017;5:84–91.
Chen YP, Zhang Y, Lv JW, et al. Genomic analysis of tumor microenvironment immune types across 14 solid Cancer types: immunotherapeutic implications. Theranostics. 2017;7:3585–94.
Chabanon RM, Pedrero M, Lefebvre C, Marabelle A, Soria JC, Postel-Vinay S. Mutational landscape and sensitivity to immune checkpoint blockers. Clin Cancer Res. 2016;22:4309–21.
Buecher B, Cacheux W, Rouleau E, Dieumegard B, Mitry E, Lievre A. Role of microsatellite instability in the management of colorectal cancers. Digest Liver Dis. 2013;45:441–9.
Le DT, Uram JN, Wang H, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med. 2015;372:2509–20.
Hugo W, Zaretsky JM, Sun L, et al. Genomic and Transcriptomic features of response to anti-PD-1 therapy in metastatic melanoma. Cell. 2016;165:35–44.
Miao D, Margolis CA, Gao W, et al. Genomic correlates of response to immune checkpoint therapies in clear cell renal cell carcinoma. Science. 2018;359:801–6.
Fuchs CS, Doi T, Jang RW, et al. Safety and efficacy of Pembrolizumab Monotherapy in patients with previously treated advanced gastric and Gastroesophageal junction Cancer: phase 2 clinical KEYNOTE-059 trial. JAMA Oncol. 2018;4:e180013.
Campbell BB, Light N, Fabrizio D, et al. Comprehensive Analysis of Hypermutation in Human Cancer. Cell. 2017;171:1042–56 e10.
Bonneville R, Krook MA, Kautto EA, et al. Landscape of microsatellite instability across 39 Cancer types. JCO Precision Oncol. 2017;2017:10.1200/PO.17.00073. https://doi.org/10.1200/PO.17.00073.
Takamochi K, Takahashi F, Suehara Y, et al. DNA mismatch repair deficiency in surgically resected lung adenocarcinoma: Microsatellite instability analysis using the Promega panel. Lung cancer (Amsterdam, Netherlands). 2017;110:26–31.
Song Z, Cheng G, Xu C, Wang W, Shao Y, Zhang Y. Clinicopathological characteristics of POLE mutation in patients with non-small-cell lung cancer. Lung cancer (Amsterdam, Netherlands). 2018;118:57–61.
Zehir A, Benayed R, Shah RH, et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med. 2017;23:703–13.
Hou Y, Nitta H, Parwani AV, Li Z. PD-L1 and CD8 are associated with deficient mismatch repair status in triple-negative and HER2-positive breast cancers. Hum Pathol. 2019;86:108–14.
Mills AM, Dill EA, Moskaluk CA, Dziegielewski J, Bullock TN, Dillon PM. The relationship between mismatch repair deficiency and PD-L1 expression in breast carcinoma. Am J Surg Pathol. 2018;42:183–91.
Wen YH, Brogi E, Zeng Z, et al. DNA mismatch repair deficiency in breast carcinoma: a pilot study of triple-negative and non-triple-negative tumors. Am J Surg Pathol. 2012;36:1700–8.
Vranic S, Palazzo J, Sanati S, et al. Potential novel therapy targets in neuroendocrine carcinomas of the breast. Clin Breast Cancer. 2019;19:131–6.
Balbas MD, Burgess MR, Murali R, et al. MAGI-2 scaffold protein is critical for kidney barrier function. Proc Natl Acad Sci U S A. 2014;111:14876–81.
Tolkacheva T, Boddapati M, Sanfiz A, Tsuchida K, Kimmelman AC, Chan AM. Regulation of PTEN binding to MAGI-2 by two putative phosphorylation sites at threonine 382 and 383. Cancer Res. 2001;61:4985–9.
Vazquez F, Grossman SR, Takahashi Y, Rokas MV, Nakamura N, Sellers WR. Phosphorylation of the PTEN tail acts as an inhibitory switch by preventing its recruitment into a protein complex. J Biol Chem. 2001;276:48627–30.
Wu X, Hepner K, Castelino-Prabhu S, et al. Evidence for regulation of the PTEN tumor suppressor by a membrane-localized multi-PDZ domain containing scaffold protein MAGI-2. Proc Natl Acad Sci U S A. 2000;97:4233–8.
David SN, Arnold Egloff SA, Goyal R, et al. MAGI2 is an independent predictor of biochemical recurrence in prostate cancer. Prostate. 2018;78:616–22.
Goldstein J, Borowsky AD, Goyal R, et al. MAGI-2 in prostate cancer: an immunohistochemical study. Hum Pathol. 2016;52:83–91.
Goldstein J, Goyal R, Roland JT, et al. MAGI-2 is a sensitive and specific marker of prostatic adenocarcinoma: a comparison with AMACR. Am J Clin Pathol. 2016;146:294–302.
Hu Y, Li Z, Guo L, et al. MAGI-2 inhibits cell migration and proliferation via PTEN in human hepatocarcinoma cells. Arch Biochem Biophys. 2007;467:1–9.
Mahdian R, Nodouzi V, Asgari M, et al. Expression profile of MAGI2 gene as a novel biomarker in combination with major deregulated genes in prostate cancer. Mol Biol Rep. 2014;41:6125–31.
Zhao J, Chen AX, Gartrell RD, et al. Immune and genomic correlates of response to anti-PD-1 immunotherapy in glioblastoma. Nat Med. 2019;25:462–9.
Cretella D, Digiacomo G, Giovannetti E, Cavazzoni A. PTEN alterations as a potential mechanism for tumor cell escape from PD-1/PD-L1 inhibition. Cancers. 2019;11:1318.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Study design: All. Data collection: PM, CEF and ZL. Data analysis: PM, CEF, LW and ZL. Statistical oversight: LW. Manuscript preparation: All. Manuscript revision: All. Manuscript approval: All.
Corresponding author
Ethics declarations
Consent for publication
All.
Availability of data and materials: Original data are available from the authors upon request.
Competing interests: All authors have no competing interests to disclose.
Competing interests
All authors have no potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The abstract was presented as platform on USCAP Annual meeting in Washington DC on March 9th, 2019.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mei, P., Freitag, C.E., Wei, L. et al. High tumor mutation burden is associated with DNA damage repair gene mutation in breast carcinomas. Diagn Pathol 15, 50 (2020). https://doi.org/10.1186/s13000-020-00971-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13000-020-00971-7