Abstract
Background
A multimodal and preventative approach to providing postoperative analgesia is becoming increasingly popular for children and adults, with the aim of reducing reliance on opioids. We conducted a prospective, randomized double-blind study to compare the analgesic efficacy of intravenous paracetamol and dipyrone in the early postoperative period in school-age children undergoing lower abdominal surgery with spinal anesthesia.
Methods
Sixty children scheduled for elective lower abdominal surgery under spinal anesthesia were randomized to receive either intravenous paracetamol 15 mg/kg, dipyrone 15 mg/kg or isotonic saline. The primary outcome measure was pain at rest, assessed by means of a visual analog scale 15 min, 30 min, 1 h, 2 h, 4 h and 6 h after surgery. If needed, pethidine 0.25 mg/kg was used as the rescue analgesic. Time to first administration of rescue analgesic, cumulative pethidine requirements, adverse effects and complications were also recorded.
Results
There were no significant differences in age, sex, weight, height or duration of surgery between the groups. Pain scores were significantly lower in the paracetamol group at 1 h (P = 0.030) and dipyrone group at 2 h (P = 0.010) when compared with placebo. The proportion of patients requiring rescue analgesia was significantly lower in the paracetamol and dipyrone groups than the placebo group (vs. paracetamol P = 0.037; vs. dipyrone P = 0.020). Time to first analgesic requirement appeared shorter in the placebo group but this difference was not statistically significant, nor were there significant differences in pethidine requirements, adverse effects or complications.
Conclusion
After lower abdominal surgery conducted under spinal anesthesia in children, intravenous paracetamol appears to have similar analgesic properties to intravenous dipyrone, suggesting that it can be used as an alternative in the early postoperative period.
Trial registration
Clinical Trials.gov. Identifier: NCT01858402.
Similar content being viewed by others
Background
Acute pain is one of the most unpleasant experiences of childhood, and is generally a consequence of injury, illness, or medical intervention [1]. Acute pain management in children is increasingly characterized by multimodal or preventative approaches. The former comprises a combination of drugs and techniques such as non-steroidal anti-inflammatory drugs (NSAIDs), opioids, paracetamol, and regional or neuraxial anesthesia.
During the last three decades, spinal anesthesia has become increasingly popular in pediatric practice, but its use is not universal and some patients, anesthesiologists and surgeons still prefer general anesthesia. Nonetheless, spinal anesthesia is an easy and effective technique that provides highly effective analgesia, and sympathetic and motor block in the lower part of the body [2].
Single-shot intrathecal blocks have a limited duration of action, depending on the local anesthetic agent used. Therefore, a combination of other analgesics is required to treat pain when the spinal block wears off. These include opioids, non-opioids, and adjuvant drugs. Opioids are often used to treat moderate to severe pain in children; however, their use is limited by undesirable side effects such as cardiovascular, central nervous system and respiratory depression, itching, urinary retention, and nausea and vomiting [3].
Many studies in adults and children have shown that non-opioid analgesics such as paracetamol, NSAIDs, and dipyrone exhibit an opioid sparing effect and improve the quality of postoperative analgesia [4]. Paracetamol is the most commonly used analgesic to treat mild and moderate postoperative pain in children [1]; an intravenous formulation is now available. Dipyrone is a pyrazoline-derived analgesic drug with antipyretic, anti-inflammatory, and spasmolytic properties. The reliability and efficiency of intravenous paracetamol has been demonstrated in several clinical studies [5–7], and some have compared the antipyretic effectiveness of paracetamol with dipyrone in young children with fever [6, 7].
The aim of this study was to assess the analgesic effect of intravenous paracetamol and dipyrone for postoperative pain relief in children undergoing spinal anesthesia for lower abdominal surgery.
Methods
The Institutional Ethics Committee of Baskent University Faculty of Medicine approved the study protocol [Project no: KA 09/06]. Written, informed consent was obtained from the parents or guardians of each patient. A total of 63 healthy, ASA physical status I and II children, aged 8 to 15 years, undergoing elective lower abdominal surgery were enrolled in this study. Exclusion criteria included any known contraindication for spinal anesthesia, such as increased intracranial pressure, hemorrhagic diathesis and infection at the puncture site. Those with a known history of allergy to the study drugs were excluded.
Intraoperative monitoring consisted of non-invasive blood pressure measurement, electrocardiogram, pulse oximetry, and end-tidal carbon dioxide measurement using a nasal adapter. After peripheral intravenous access had been obtained, an infusion of 0.45% NaCl in 5% glucose was administered at 5 ml/kg/h. All patients had been premedicated with intravenous midazolam 0.05 mg/kg before lumbar puncture and supplemental oxygen 3 l/min was administered. Children who were anxious or felt uncomfortable after premedication or during surgery received further sedation with intravenous boluses of propofol 0.5–1.0 mg/kg.
Lumbar puncture was performed with the children in the lateral decubitus position with the midline approach with a 26-gauge spinal needle (Atraucan; Braun, Melsungen, Germany) at the L4–5 intervertebral space. After free flow of CSF was observed, 0.3 mg/kg 0.5% hyperbaric bupivacaine was injected. The extent of sensory block was tested with a pinprick method, and the degree of motor blockade was assessed using the modified Bromage scale [6, 8].
The children were randomized to one of three groups according to a pre-generated randomization scheme created by the web site Randomization.com.
(http://www.randomization.com).
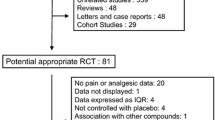
After spinal anesthesia, children in Group Paracetamol received intravenous paracetamol (Perfalgan™ Bristol-Myers Squibb GmbH, München, Germany) 15 mg/kg premixed with 0.9% NaCl to a total of 50 ml. Group Dipyrone received intravenous dipyrone (Adepiron®, Adeka, Istanbul, Turkey) 15 mg/kg premixed with 0.9% NaCl to a total of 50 ml. The placebo group, received 50 ml 0.9% NaCl intravenously (Figure 1). All study drugs had been prepared by a researcher (MS) blinded to the treatment protocol, and were administered using identical infusion pumps over 15 min by another researcher (AK) blinded to the content of the infusion.
Intraoperative hemodynamic data, operation types, duration of surgery and degree of motor blockade were recorded. After surgery, the children were transferred to the post-anesthesia care unit (PACU), and the time taken for the block to recede by two segments was recorded. A consultant anesthetist (EC) blinded to the group to which each patient had been assigned performed all subsequent assessments.
The intensity of postoperative pain at rest was assessed using a visual analog scale (VAS) (where 0 represented no pain and 10 the worst pain ever experienced) at 15 and 30 minutes, and 1 h, 2 h, 4 h and 6 h after surgery. Pain at rest was the primary outcome measure.
Each patient’s sedation level was measured using a graded scale (0 = fully awake, 1 = awake but drowsy, 2 = sleeping, but arousable by light touch or speech, and 3 = sleeping, not arousable) at the same time. Postoperative pain was treated according to the same protocol in all groups. Intravenous pethidine 0.25 mg/kg was administered as rescue analgesia when VAS exceeded 4 out of 10, until the pain score was less than 4 or to a total dose of 1 mg/kg. Time to first administration of pethidine and cumulative pethidine consumption during the first six postoperative hours were recorded as secondary outcome measures.
Sedation levels, and all adverse effects including hypotension (>20% decrease in systolic blood pressure from baseline), bradycardia (heart rate <60 beats/min), respiratory depression, and nausea or vomiting were recorded and treated until the child was discharged. Children were discharged from the PACU when they were fully awake, hemodynamically stable, breathing satisfactorily and able to flex their hips. The time taken to be ready for PACU discharge was also recorded.
Statistical analysis
A priori power analysis was performed based on the likely difference in the subjects’ postoperative pain scores evaluated by VAS. Sample size calculation was informed by the findings of a study previously undertaken at our institution [9], which indicated a likely 30% reduction in pain scores reported by subjects receiving an analgesic drug compared with placebo. We identified that the highest pain scores tended to be reported 2 h after surgery, equating to a maximum difference between means of 14 mm on the VAS with a standard deviation (SD) of 15 mm. Assuming a two-tailed type I error α = 0.05 and a power of 0.80, a priori analysis suggested 19 patients would be needed in each group (Power and Precision™ Biostat Inc., Englewood, NJ). All subsequent statistical analyses were performed using SPSS for Windows software (Statistical Package for the Social Sciences, version 17.0, SSPS Inc., Chicago, IL, USA). The analysis of variance test (ANOVA) was used for numerical and continuous variables to assess differences between groups. Homogeneity of variances was calculated using Levene’s test and Lilliefors significance correction. Post hoc analyses were performed with the Bonferroni test. Either the chi-square or Fisher’s exact test was used to analyze categorical variables when appropriate. Data are presented as mean ± SD, median with range or number of cases. A P value <0.05 was considered statistically significant.
Results
Sixty-three patients were invited to participate. During screening, two patients were found not to meet the inclusion criteria, and one patient’s parents declined consent. A total of 60 patients constituted the study population (Figure 1). There were no statistically significant differences between the groups with regard to age, sex, weight, type of operation, duration of surgery, or anesthesia (Table 1).
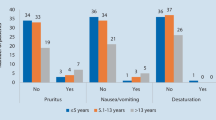
Visual analogue scale (VAS) scores were statistically significant between Group Paracetamol and the placebo group after 1 hour (p = 0.030) and between Group Dipyrone and the placebo group after 2 h (p = 0.010). There was no statistically significant difference in pain scores at any other times. The pain scores recorded on emergence from spinal anesthesia and in the first 6 hours after surgery are shown in Figure 2.
The number of patients who received rescue analgesia was significantly lower for the Paracetamol and Dipyrone groups compared with the placebo group (paracetamol versus placebo, p = 0.037; dipyrone versus placebo, p = 0.020) (Table 2). Intravenous pethidine was given to 14 (70%) patients in the Paracetamol group, 12 (60%) in the Dipyrone group and 19 (95%) in the placebo group (Figure 3).
The mean time to administration of rescue analgesia was 2.9 ± 1.3 h in the Paracetamol group, 2.1 ± 1.5 h in the Dipyrone group, and 1.8 ± 1.3 h in the placebo group, but these differences were not statistically significant (Table 2). There were also no significant differences in cumulative pethidine consumption or sedation scores between the three groups at any time point. Duration of stay in and time to meet the discharge criteria for the PACU, and time taken for regression of the sensory block and recovery of the motor block were broadly similar between the groups. There were no significant changes in hemodynamic parameters from baseline in either active treatment group. No episodes of hypotension or respiratory depression were recorded intraoperatively or in the PACU. Bradycardia was observed in two patients in each group (Table 3). There were also no significant differences in the incidence of postoperative nausea, vomiting, requirement for antiemetic rescue medication or any other perioperative adverse events between the groups (Table 3). No episodes of agranulocytosis were reported.
Discussion
We evaluated the efficacy of intravenous paracetamol and dipyrone for administered as postoperative analgesia after day-case lower abdominal surgery in children. We found that postoperative pain scores were significantly lower in the active treatment groups in the first and second postoperative hours when compared with placebo, but there were no statistical differences in pain scores between the three groups at other times. We also found that the proportion of patients requiring rescue analgesia was significantly lower in the active treatment groups compared with placebo; however, there were no statistical differences in cumulative analgesic consumption.
The historic view that young children neither respond to, nor remember, painful experiences to the same degree as adults is no longer thought to be true [1]. Most premature neonates are capable of experiencing pain, and under treatment of pain results in harmful physiological and behavioral responses that have long-lasting negative consequences on the developing nociceptive systems [8, 10]. Mather and Mackie [11] reported that 40% of children undergoing surgery experienced moderate to severe postoperative pain, and that 75% received inadequate pain treatment [12, 13].
It has been reported that providing inadequate analgesia to infants, preverbal children, and adolescents results not only in short term physiologic disturbance but also longer term behavioral changes, particularly during immunization [10, 14, 15]. It is now recognized that optimal postoperative pain management is essential for children, and that this should begin before surgery by providing children and their parents with information about the planned surgical procedure [16].
Treatments for postoperative pain include drugs such as opioids, NSAIDs, paracetamol and dipyrone, as well as regional anesthetic techniques such as spinal and caudal anesthesia. The provision of adequate pain control must be balanced against the risk of the side effects of analgesics.
Neuraxial anesthesia in children is safe, provided appropriate care and attention are paid. Spinal anesthesia modifies the neuroendocrine stress response, ensures a more rapid recovery, and may shorten hospital stay with fewer opioid-induced side effects [17]. Furthermore, spinal anesthesia provides profound analgesia with minimal physiologic perturbations or side effects [17], and there is a growing interest in using the technique for surgery in preschool and school aged children [18]. Most studies in these populations have focused on specific procedures; none has examined the efficacy of paracetamol or dipyrone for pain relief after spinal anesthesia has worn off.
The main limitation of spinal anesthesia is the variable and relatively short duration of the block obtained with a single-shot local anesthetic injection technique [2]. Adding parenteral or enteral analgesic drugs such as opioid or NSAIDs is one means of overcoming these problems and thereby increasing the quality and duration of analgesia. Opioids are often used to provide effective postoperative analgesia; however, undesirable side effects may frequently be observed as a consequence of their use. Ideally a non-opioid analgesic such as paracetamol, an NSAID or dipyrone should be used to provide effective pain relief to minimize the need for opioids [19]. The safety of analgesic therapy has improved considerably as this multimodal opioid-sparing approach has been adopted; however, there are limited data concerning the efficacy of these regimes in the early postoperative period after surgery in children [20].
Paracetamol is commonly used as an analgesic and antipyretic in pediatric practice. It primarily acts centrally, where it is a potent antipyretic and mild analgesic. In recent years, an intravenous formulation has been introduced, and its safety and pharmacokinetic profile have been established for children as young as 1 month of age [12, 21]. Dipyrone, a pyrazoline derivate, has antispasmodic, antipyretic and anti-inflammatory effects. It is widely used as an injectable non-opioid analgesic in several European and South American countries, where it has gained popularity due to the low incidence of adverse reactions (although like some other opioids it carries a low risk of agranulocytosis) [22]. Grundmann and colleagues stated that very large prospective studies would be needed to determine the true incidence of agranulocytosis [23]. A study comparing the adverse effects of paracetamol, diclofenac, aspirin and dipyrone reported that dipyrone was relatively well tolerated and shared many of the potential side effects of NSAIDs [22]. In our study, no incidences of agranulocytosis were reported.
Paracetamol may be preferred to dipyrone in children owing to its equal analgesic potency and lower risk of adverse effects. Several clinical studies have confirmed that the analgesic efficacy of intravenous paracetamol is comparable with that of NSAIDs or dipyrone in orthopedic, abdominal, and breast surgery in adults [22, 24, 25]. Landwehr and colleagues [24] reported that dipyrone and paracetamol had similar analgesic potencies after retinal surgery, whereas Grundmann and colleagues [23] demonstrated that the analgesic potency of dipyrone was superior to paracetamol during the first two postoperative hours after lumbar disc surgery. To date, the only study comparing the use of paracetamol with dipyrone in children examined their antipyretic properties [6]. Ours is the first study to examine their analgesic properties, and found that they have broadly similar efficacy in the first six hours after lower abdominal surgery in children.
Various studies have compared the analgesic efficacy of intravenous paracetamol with other analgesic agents such as tramadol, NSAIDs, and pethidine in children [5, 19]. Alhashemi and colleagues reported that intravenous paracetamol was as efficient an analgesic as intramuscular pethidine in children undergoing tonsillectomy [19]. Paracetamol provided significantly greater analgesic effect than a placebo after orthopedic surgery in children [26], and a relatively large intravenous dose improved pain control after major spinal surgery in children and adolescents [27].
Our results demonstrate that paracetamol and dipyrone provide effective and comparable analgesia 1 h and 2 h after surgery, respectively, based on a lower and equivalent VAS scores compared with placebo. Although more patients in the placebo group required rescue analgesia, pain scores and cumulative pethidine consumption in the three groups were not significantly different in the first six postoperative hours. This concurs with the findings of Cakan and colleagues, who found that paracetamol 1 g administered intravenously at the end of surgery and 6 hourly thereafter did not reduce opioid requirements but improved the quality of pain relief [28].
A possible explanation for these findings might be that the sample size in our study was not large enough to detect subtle differences. Our power analysis was based on the assumption that detecting a 30% decrease in pain score on a VAS was clinically relevant and should be our primary outcome measure, but this might not be sufficiently large to detect pethidine consumption. This might also explain the lack of a significant difference in time to first analgesic requirement. It is notable that in previous studies of the use of bupivacaine for spinal anesthesia in children, the time to first analgesic requirement in the placebo group was 168 ± 70 min, which was broadly similar to our findings [29]. It is likely that in some patients the spinal anesthesia was still effective in the early postoperative period. It has been suggested that if the duration of preemptive analgesia extends into the postoperative period, it is more likely that pain hypersensitivity can be avoided [3]. Also, the provision of pethidine as rescue analgesia is likely to have influenced the subsequent low pain scores in all groups.
In our opinion, both paracetamol and dipyrone can be considered effective and equipotent analgesics in the early postoperative period, but that the small differences when compared with placebo indicate that they both only exert a mild effect.
The use of opioid analgesics is an important risk factor for postoperative nausea and vomiting (PONV). A reduction in the amount of systemic opioids would be expected to reduce the incidence of PONV and other common side effects. In our study, the use of pethidine was significantly lower in the paracetamol and dipyrone groups compared with the placebo group, but there was no statistically significant difference in the incidence of PONV between the groups. This may be a consequence of broadly similar cumulative pethidine doses administered to participants in each group.
Conclusion
In conclusion, our study showed that preemptive administration of intravenous paracetamol or dipyrone provided effective pain control and reduced pethidine requirements in the first and second postoperative hours compared with placebo. Paracetamol appears to be at least as effective as dipyrone for pain relief, and it can be recommended as a viable alternative to dipyrone after lower abdominal surgery in children.
Abbreviations
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- VAS:
-
Visual analog scale
- PONV:
-
Postoperative nausea and vomiting.
References
Kraemer WF: Treatment of acute pediatric pain. Semin Pediatr Neurol. 2010, 17 (4): 268-274.
Kokki H: Spinal blocks. Pediatr Anesth. 2012, 22 (1): 56-64.
Yaster M: Multimodal analgesia in children. Eur J Anaesthesiol. 2010, 27 (10): 851-857.
Marret E, Kurdi O, Zufferey P, Bonnet F: Effects of nonsteroidal anti-inflammatory drugs on patient-controlled analgesia morphine side effects: meta-analysis of randomized controlled trials. Anesthesiology. 2005, 102 (6): 1249-1260.
Uysal HY, Takmaz SA, Yaman F, Baltaci B, Basar H: The efficacy of intravenous paracetamol versus tramadol for postoperative analgesia after adenotonsillectomy in children. J Clin Anesth. 2011, 23 (1): 53-57.
Wong A, Sibbald A, Ferrero F, Plager M, Santolaya ME, Escobar AM, Campos S, Barragan S, De Leon GM, Kesselring GL, Fever Pediatric Study Group: Antipyretic effects of dipyrone versus ibuprofen versus acetaminophen in children: results of a multinational, randomized, modified double-blind study. Clin Pediatr (Phila). 2001, 40 (6): 313-324.
Kokki H, Tuovinen K, Hendolin H: Spinal anaesthesia for paediatric day-case surgery: a double-blind, randomized, parallel group, prospective comparison of isobaric and hyperbaric bupivacaine. Br J Anaesth. 1998, 81 (4): 502-506.
Walker SM, Franck LS, Fitzgerald M, Myles J, Stocks J, Marlow N: Long-term impact of neonatal intensive care and surgery on somatosensory perception in children born extremely preterm. Pain. 2009, 141 (1–2): 79-87.
Calışkan E, Sener M, Koçum A, Bozdoğan N, Arıboğan A: Our experiences with spinal anesthesia in pediatric patients. Agri. 2011, 23 (3): 100-106.
Taddio A, Katz J: The effects of early pain experience in neonates on pain responses in infancy and childhood. Pediatr Drugs. 2005, 7 (4): 245-257.
Mather L, Mackie J: The incidence of postoperative pain in children. Pain. 1983, 15 (3): 271-282.
Fitzgerald M, Beggs S: The neurobiology of pain: developmental aspects. Neuroscientist. 2001, 7 (3): 246-257.
Henneberg SW, Nilsson LB: Acute paediatric pain. Current Anaesth Crit Care. 2007, 18 (3): 126-134.
Taddio A, Nulman I, Koren BS, Stevens B, Koren G: A revised measure of acute pain in infants. J Pain Symptom Manage. 1995, 10 (6): 456-463.
Anand KJ, Hall RW: Pharmacological therapy for analgesia and sedation in the newborn. Arch Dis Child Fetal Neonatal Ed. 2006, 91 (6): F448-F453.
İvani G, Tonetti F, Mossetti V: Update on postoperative analgesia in children. Minerva Anestesiol. 2005, 71 (9): 501-505.
Sang CN, Berde CB: A multicenter study on safety and risk factors in pediatric regional analgesia. Anesthesiology. 1994, 81 (3A): A1387-
Kokki H, Hendolin H, Turunen M: Postdural puncture headache and transient neurologic symptoms in children after spinal anesthesia using cutting and pencil point paediatric spinal needles. Acta Anaesthesiol Scand. 1998, 42 (9): 1076-1082.
Alhashemi JA, Daghistani MF: Effects of intraoperative i.v. acetaminophen vs i.m. meperidine on post-tonsillectomy pain in children. Br J Anaesth. 2006, 96 (6): 790-795.
Verghese ST, Hannallah RS: Acute pain management in children. J Pain Res. 2010, 15 (3): 105-123.
Wilson-Smith EM, Morton NS: Survey of i.v.paracetamol (acetaminophen) use in neonates and infants under 1 year of age by UK anesthetists. Pediatr Anaesth. 2009, 19 (4): 329-337.
Ohnesorge H, Bein B, Hanss R, Francksen H, Mayer L, Scholz J, Tonner PH: Paracetamol versus metamizol in the treatment of postoperative pain after breast surgery: a randomized controlled trial. Eur J Anaesthesiol. 2009, 26 (8): 648-653.
Grundman U, Wörnle C, Biedler A, Kreuer S, Wrobel M, Wilhelm W: The efficacy of the non-opioid analgesics parecoxib, paracetamol and metamizol for postoperative pain relief after lumbar microdiscectomy. Anesth Analg. 2006, 103 (1): 217-222.
Landwehr S, Kiencke P, Giesecke T, Eggert D, Thumann G, Kampe S: A comparison between IV paracetamol and IV metamizol for postoperative analgesia after retinal surgery. Curr Med Res Opin. 2005, 21 (10): 1569-1575.
Kampe S, Warm M, Landwehr S, Dagtekin O, Haussmann S, Paul M, Pilgram B, Kiencke P: Clinical equivalence of IV paracetamol compared to IV dipyrone for postoperative analgesia after surgery for breast cancer. Curr Med Res Opin. 2006, 22 (10): 1949-1954.
Granry JC, Rod B, Monrigal JP, Merckx J, Berniere J, Jean N, Boccard E: The analgesic efficacy of an injectable prodrug of acetaminophen in children after orthopedic surgery. Pediatr Anaesth. 1997, 7 (6): 445-449.
Hiller A, Helenius I, Nurmi E, Neuvonen PJ, Kaukonen M, Hartikainen T, Korpela R, Taivainen T, Meretoja OA: Acetaminophen improves analgesia but does not reduce opioid requirement after major pine surgery in children and adolescents. Spine (Phila Pa 1976). 2012, 37 (20): E1225-E1231.
Cakan T, Inan N, Culhaoglu S, Bakkal K, Basar H: Intravenous paracetamol improves the quality of postoperative analgesia but not decrease narcotic requirements. J Neurosurg Anesthesiol. 2008, 20 (3): 169-173.
Duman A, Apılıogulları S, Duman I: Effects of intrathecal fentanyl on quality of spinal anesthesia in children undergoing inguinal hernia repair. Pediatr Anaesth. 2010, 20 (6): 530-536.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2253/13/34/prepub
Acknowledgements
This study has been supported by the University research fund.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors have no conflicts of interest to declare.
Authors’ contributions
All those listed as authors contributed to the preparation of the manuscript. Each listed author participated in the work to the extent that they can all publicly defend its content. EC coordinated the study and wrote the draft manuscript. MS participated in study design and undertook the statistical analysis. AK, NB, SSE and AA conceived the study, participated in its design, and coordinated the drafting of the manuscript. All authors have read and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Caliskan, E., Sener, M., Kocum, A. et al. The efficacy of intravenous paracetamol versus dipyrone for postoperative analgesia after day-case lower abdominal surgery in children with spinal anesthesia: a prospective randomized double-blind placebo-controlled study. BMC Anesthesiol 13, 34 (2013). https://doi.org/10.1186/1471-2253-13-34
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2253-13-34