Abstract
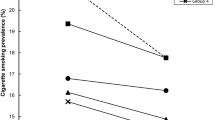
Persons with mental illness smoke at twice the rate of the general United States (US) population and die an average of 25-years younger, often from preventable diseases. This study seeks to determine whether disparities in smoking have increased over the past decade and whether Clean Indoor Air Laws (CIALs) are associated with changes in smoking among those with poor mental health. We used a fixed-effects model for estimation. CIALs were associated with 15 per cent decreased odds of smoking among adults in the US. Among those with poor mental health, these same laws had no effect. Between 2000 and 2010, the disparity in smoking rates between these two populations has steadily increased from 1.8 to 2.2 times greater. Given the lack of association between tobacco laws and smoking among those with poor mental health, alternative and more targeted tobacco reduction efforts may be necessary.


Similar content being viewed by others
References
Murphy, J.M., Horton, N.J., Monson, R.R., Laird, N.M., Sobol, A.M. and Leighton, A.H. (2003) Cigarette smoking in relation to depression: Historical trends from the Stirling County Study. American Journal of Psychiatry 160(9): 1663–1669.
King, B., Dube, S., Kaufmann, R., Shaw, L. and Pechacek, T. (2011) Vital Signs: Current Cigarette Smoking Among Adults Aged ≥18 Years-United States, 2005–2010. Centers for Disease Control and Prevention. Morbidity and Mortality Weekly Report 60(35): 1207.
Haw, S.J. and Gruer, L. (2007) Changes in exposure of adult non-smokers to secondhand smoke after implementation of smoke-free legislation in Scotland: National cross sectional survey. BMJ: British Medical Journal 335(7619): 549.
Farrelly, M.C., Davis, K.C., Haviland, M.L., Messeri, P. and Healton, C.G. (2005) Evidence of a dose-response relationship between ‘truth’ antismoking ads and youth smoking prevalence. American Journal of Public Health 95(3): 425–431.
Chaloupka, F. (1992) Clean Indoor Air Laws, addiction and cigarette smoking. Applied Economics 24(2): 193–205.
Farrelly, M.C. et al (2013) A comprehensive examination of the influence of state tobacco control programs and policies on youth smoking. American Journal of Public Health 103(3): 549–555.
Lasser, K., Boyd, J.W., Woolhandler, S., Himmelstein, D.U., McCormick, D. and Bor, D.H. (2000) Smoking and mental illness. JAMA: The Journal of the American Medical Association 284(20): 2606–2610.
Lawrence, D., Mitrou, F. and Zubrick, S.R. (2009) Smoking and mental illness: Results from population surveys in Australia and the United States. BMC Public Health 9(1): 285.
Mrazek, P.B. and Haggerty, R.J. (eds.) (1994) Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research: Summary. Washington DC: National Academies Press.
US Department of Health & Human Services. (2010) Healthy people 2020, http://www.healthypeople.gov, accessed 1 June 2014.
Levy, D.T., Chaloupka, F.J. and Gitchell, J. (2004) The effects of tobacco control policies on smoking rates: A tobacco control scoreboard. Journal of Public Health Management Practice 10(4): 338–353.
Chaloupka, F.J., Levy, D. and Huang, J. (2011) The Impact of Tax and Smoke Free Air Policy Changes. Princeton, NJ: Robert Wood Johnson Foundation.
Parks, J., Svendsen, D., Singer, P., Foti, M.E. and Mauer, B. (2006) Morbidity and Mortality in People with Serious Mental Illness. National Association of State Mental Health Program Directors (NASMHPD). Alexandria, VA: Medical Directors Council.
US Surgeon General. (1964) Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington DC: US Department of Health, Education and Welfare, Public Health Service Publication (1103).
US Surgeon General. (1982) The Health Consequences of Smoking. Chronic Obstructive Lung Disease. Washington DC: US Department of Health and Human Resources Publication (84-50205).
Department of Health and Human Services Centers for Disease Control and Prevention. (2010) How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA.
Colton, C. and Manderscheid, R. (2006) Congruencies in increased mortality rates, years of potential life lost, and cuases of death among mental health clients in eight states. Preventing Chronic Disease 3(2): 1–14.
Dinno, A. and Glantz, S. (2009) Tobacco control policies are egalitarian: A vulnerabilities perspective on Clean Indoor Air Laws, cigarette prices, and tobacco use disparities. Social Science and Medicine 68(8): 1439–1447.
Thomas, S. et al (2008) Population tobacco control interventions and their effects on social inequalities in smoking: Systematic review. Tobacco Control 17(4): 230–237.
Centers for Disease Control and Prevention (CDC) BRFSS. (2013) The BRFSS data user guide, 15 August.
Americans for Nonsmokers’ Rights. (2014) Smokefree lists, maps, and data, http://www.no-smoke.org/goingsmokefree.php?id=519, accessed 18 April 2014.
US Surgeon General. (1986) The Health Consequences of Smoking: A Report of the Surgeon General. Washington DC: US Department of Health and Human Services, Office on Smoking and Health.
Klein, J.D., Thomas, R.K. and Sutter, E.J. (2007) Self-reported smoking in online surveys: Prevalence estimate validity and item format effects. Medical Care 45(7): 691–695.
Moriarty, D., Zack, M. and Kobau, R. (2003) The centers for disease control and prevention’s healthy days measures – Population tracking of perceived physical and mental health over time. Health and Quality of Life Outcomes 1(1): 37.
Centers for Disease Control and Prevention (CDC). (1998) Self-reported frequent mental distress among adults – United States, 1993–1996. Morbidity and Mortality Weekly Report 47(16): 325–331.
Garrett, B.E., Dube, S.R., Trosclair, A., Caraballo, R.S. and Pechacek, T.F. and Centers for Disease Control and Prevention (CDC) (2011) Cigarette smoking – United States, 1965–2008. MMWR Surveillance Summary 60(1): 109–113.
Bien, T.H. and Burge, R. (1990) Smoking and drinking: A review of the literature. Substance Use & Misuse 25(12): 1429–1454.
Kaczynski, A.T., Manske, S.R., Mannell, R.C. and Grewal, K. (2008) Smoking and physical activity: A systematic review. American Journal of Health Behavior 32(1): 93–110.
Ettner, S.L. (1999) The relationship between continuity of care and the health behaviors of patients: Does having a usual physician make a difference? Medical Care 37(6): 547–555.
Borland, R., Yong, H.H., Cummings, K.M., Hyland, A., Anderson, S. and Fong, G.T. (2006) Determinants and consequences of smoke-free homes: Findings from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control 15(Suppl 3): 42–50.
Davern, M., Rodin, H., Beebe, T.J. and Call, K.T. (2005) The effect of income question design in health surveys on family income, poverty and eligibility estimates. Health Services Research 40(5, p1): 1534–1552.
Little, R.J. (1988) Missing-data adjustments in large surveys. Journal of Business & Economic Statistics 6(3): 287–296.
Siru, R., Hulse, G.K. and Tait, R.J. (2009) Assessing motivation to quit smoking in people with mental illness: A review. Addiction 104(5): 719–733.
Compton, M.T., Daumit, G.L. and Druss, B.G. (2006) Cigarette smoking and overweight/obesity among individuals with serious mental illnesses: A preventive perspective. Harvard Review of Psychiatry 14(4): 212–222.
DiClemente, C.C., Nidecker, M. and Bellack, A.S. (2008) Motivation and the stages of change among individuals with severe mental illness and substance abuse disorders. Journal of Substance Abuse Treatment 34(1): 25–35.
Khantzian, E.J. (1997) The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry 4(5): 231–244.
Evans, D.E. and Drobes, D.J. (2009) Nicotine self‐medication of cognitive‐attentional processing. Addiction Biology 14(1): 32–42.
Kumari, V. and Postma, P. (2005) Nicotine use in schizophrenia: The self medication hypotheses. Neuroscience & Biobehavioral Reviews 29(6): 1021–1034.
Lerman, C. et al (1998) Depression and self-medication with nicotine: the modifying influence of the dopamine D4 receptor gene. Health Psychology 17(1): 56.
Bryant, J., Bonevski, B., Paul, C., McElduff, P. and Attia, J. (2011) A systematic review and meta-analysis of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups. Addiction 106(9): 1568–1585.
Coverage of Preventative Health Service, 42 U.S.C. 300gg-13 (2010).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Larson, A., Bovbjerg, V. & Luck, J. State Clean Indoor Air Laws and smoking among adults with poor mental health. J Public Health Pol 37, 453–466 (2016). https://doi.org/10.1057/jphp.2016.17
Published:
Issue Date:
DOI: https://doi.org/10.1057/jphp.2016.17