Abstract
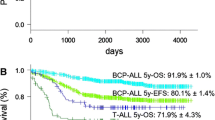
Despite many years of meticulous immunophenotyping of childhood acute lymphoblastic leukaemia (ALL) cases the prognostic significance of some subtypes remains unclear. The Medical Research Council UKALLXI trial (1990–1996) in which uniform treatment has been given to 2090 children with ALL below the age of 18 years and above the age of 1 year, has afforded the opportunity to review these issues. Children with ALL of mature B cell type were not entered into this trial. Immunophenotype analysis was performed in each individual trial centre, but results were centrally reviewed in all cases, and were both available and considered adequate in 1934 (93%) of the first 2090 patients entered. The main diagnostic categories were early pre-B or null reported in 60 cases (3.1%), common ALL in 1242 (64.2%), pre-B in 252 (13.0%), ‘common’ or pre-B in 172 (8.9%) and T cell in 207 (10.7%) cases. Children with T cell disease were significantly more likely to be over the age of 10 years, with central nervous system disease at diagnosis and to be CD34 negative. They also had a higher incidence of high white cell count and were more likely to be of the French–American–British (FAB) L2 morphological subtype. Patients with ‘null’ cell disease tended to be less than 2 years or greater than 10 years of age, and CD13 and CD33 positive. CD10 was associated with lower white cell count (WBC) at diagnosis, younger age and FAB L1 morphological subtype. The presence of cytoplasmic immunoglobulin in pre-B cells was not associated with any specific clinical or laboratory features. CD34 positivity was less common in T cell patients and was associated with low WBC. Disease-free survival (DFS) and 95% confidence intervals (CI) at 5 years from diagnosis was 52% (95% CI: 44–59%) for T cell disease, 58% (95% CI: 43–73%) for early pre-B (or null cell) disease and 65% (95% CI: 62–68%) for common or pre-B disease; there being no significant difference between common and pre-B disease with regard to disease outcome. Patients with T cell disease had a worse prognosis than any other immunophenotype group (P < 0.00005). however this worse outcome was no longer significant after allowing for the other principal prognostic factors of age, gender and white cell count at diagnosis except for the very small number with wbc <20 × 109/l and T cell disease. Those with CD10-positive leukaemia did better than those who were CD10 negative (P < 0.00005), with dfs at 5 years 64% (95% ci: 62–67%) for positive vs 56% (95% CI: 49–62%) for CD10 negative. CD10 positivity did not have independent significance when white count, gender and age were taken into account. CD13, CD33, and cytoplasmic μ positivity carried no prognostic significance.
Similar content being viewed by others
Author information
Authors and Affiliations
Consortia
Rights and permissions
About this article
Cite this article
Hann, I., Richards, S., Eden, O. et al. Analysis of the immunophenotype of children treated on the Medical Research Council United Kingdom Acute Lymphoblastic Leukaemia Trial XI (MRC UKALLXI). Leukemia 12, 1249–1255 (1998). https://doi.org/10.1038/sj.leu.2401093
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2401093
- Springer Nature Limited
Keywords
This article is cited by
-
Negative value of CD10−/CD34− immunophenotype in pediatric leukemia and development of a related cell line model for investigating drug resistance
Clinical and Translational Oncology (2022)
-
BCR-ABL Translocation in Pediatric Acute Lymphoblastic Leukemia in Southern India
Indian Journal of Hematology and Blood Transfusion (2012)
-
Long-term follow-up of the United Kingdom medical research council protocols for childhood acute lymphoblastic leukaemia, 1980–2001
Leukemia (2010)
-
Clinical features, cytogenetics and outcome in acute lymphoblastic and myeloid leukaemia of infancy: report from the MRC Childhood Leukaemia working party
Leukemia (2002)
-
Long-term follow-up of the United Kingdom Medical Research Council protocols for childhood acute lymphoblastic leukaemia, 1980–1997
Leukemia (2000)