Abstract
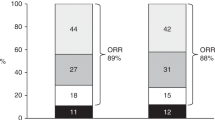
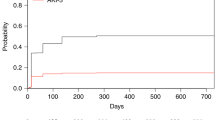
Acute kidney injury (AKI) is a complication related to important organ dysfunction during autologous stem cell transplantation (ASCT) in light chain (AL) amyloidosis. This study aims to validate the risk factors of AKI during different periods of ASCT and the impact of AKI on long-term outcomes. 302 patients with AL amyloidosis and kidney involvement who underwent ASCT were included. The procedures from stem cell mobilization to 30 days after transplantation were categorized into four periods: Period 0 (stem cell mobilization and harvest), Period 1 (preparation), Period 2 (conditioning and transplantation), and Period 3 (engraftment). The incidence of AKI during ASCT was 27.15% (0.66% in Period 0, 6.62% in Period 1, 15.23% in Period 2, and 6.95% in Period 3). The major causes of AKI were capillary leak syndrome in Period 0, ganciclovir or sulfamethoxazole/trimethoprim in Period 1, high-dose melphalan in Period 2, and engraftment syndrome in Period 3. AKI in different periods had distinct risk factors and predictive models. AKI was a risk factor for both kidney survival and overall survival (OS). Even recovered AKI reduced 10-year kidney survival from 91.7% to 68.4% (p = 0.002) and 10-year OS from 91.1% to 77.7% (p = 0.005).



Similar content being viewed by others
Data availability
The datasets are available in deidentified form from the corresponding author on reasonable request considering about the patient privacy.
References
Miao F, Ren G, Guo J, Zhao L, Xu W, Huang X. Characteristics of engraftment syndrome following autologous stem cell transplantation in light chain amyloidosis with renal involvement. Transplant Cell Ther. 2023;29:110.e1–110.e8.
Skinner M, Sanchorawala V, Seldin DC, Dember LM, Falk RH, Berk JL, et al. High-dose melphalan and autologous stem-cell transplantation in patients with AL amyloidosis: an 8-year study. Ann Intern Med. 2004;140:85–93.
Gatt ME, Palladini G. Light chain amyloidosis 2012: a new era. Br J Haematol. 2013;160:582–98.
D’Souza A, Dispenzieri A, Wirk B, Zhang MJ, Huang J, Gertz MA, et al. Improved outcomes after autologous hematopoietic cell transplantation for light chain amyloidosis: a center for international blood and marrow transplant research study. J Clin Oncol. 2015;33:3741–9.
Leung N, Slezak JM, Bergstralh EJ, Dispenzieri A, Lacy MQ, Wolf RC, et al. Acute renal insufficiency after high-dose melphalan in patients with primary systemic amyloidosis during stem cell transplantation. Am J Kidney Dis. 2005;45:102–11.
Nader R, Zhen A, Angel-Korman A, Pavlovich SS, Pogrebinsky A, Doros G, et al. Predictors and outcomes of acute kidney injury during autologous stem cell transplantation in AL amyloidosis. Nephrol Dial Transplant. 2022;37:1281–8.
Leung N, Kumar SK, Glavey SV, Dispenzieri A, Lacy MQ, Buadi FK, et al. The impact of dialysis on the survival of patients with immunoglobulin light chain (AL) amyloidosis undergoing autologous stem cell transplantation. Nephrol Dial Transplant. 2016;31:1284–9.
Bleeker JS, Gertz MA, Pellikka PA, Larson DR, Buadi F, Dingli D, et al. Evaluation of pretransplant factors predicting cardiac dysfunction following high-dose melphalan conditioning and autologous peripheral blood stem cell transplantation. Eur J Haematol. 2012;89:228–35.
Havasi A, Stern L, Lo S, Sun F, Sanchorawala V. Validation of new renal staging system in AL amyloidosis treated with high dose melphalan and stem cell transplantation. Am J Hematol. 2016;91:E458–60.
Obici L, Perfetti V, Palladini G, Moratti R, Merlini G. Clinical aspects of systemic amyloid diseases. Biochim Biophys Acta. 2005;1753:11–22.
Gertz MA, Leung N, Lacy MQ, Dispenzieri A, Zeldenrust SR, Hayman SR, et al. Clinical outcome of immunoglobulin light chain amyloidosis affecting the kidney. Nephrol Dial Transplant. 2009;24:3132–7.
Li T, Huang X, Wang Q, Zhao L, Ren G, Chen W, et al. A risk stratification for systemic immunoglobulin light-chain amyloidosis with renal involvement. Br J Haematol. 2019;187:459–69.
Huang X, Ren G, Chen W, Guo J, Zhao L, Zeng C, et al. The role of induction therapy before autologous stem cell transplantation in low disease burden AL amyloidosis patients. Amyloid. 2021;28:75–83.
Andronesi AG, Tanase AD, Sorohan BM, Craciun OG, Stefan L, Varady Z, et al. Incidence and risk factors for acute kidney injury following autologous stem cell transplantation for multiple myeloma. Cancer Med. 2019;8:3278–85.
Fadia A, Casserly LF, Sanchorawala V, Seldin DC, Wright DG, Skinner M, et al. Incidence and outcome of acute renal failure complicating autologous stem cell transplantation for AL amyloidosis. Kidney Int. 2003;63:1868–73.
Irazabal MV, Eirin A, Gertz MA, Dispenzieri A, Kumar S, Buadi FK, et al. Acute kidney injury during leukocyte engraftment after autologous stem cell transplantation in patients with light-chain amyloidosis. Am J Hematol. 2012;87:51–4.
Tamaki M, Nakasone H, Gomyo A, Hayakawa J, Akahoshi Y, Harada N, et al. Lower glomerular filtration rate predicts increased hepatic and mucosal toxicity in myeloma patients treated with high-dose melphalan. Int J Hematol. 2018;108:423–31.
Gertz MA, Comenzo R, Falk RH, Fermand JP, Hazenberg BP, Hawkins PN, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18-22 April 2004. Am J Hematol. 2005;79:319–28.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179–84.
Palladini G, Dispenzieri A, Gertz MA, Kumar S, Wechalekar A, Hawkins PN, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol. 2012;30:4541–9.
Palladini G, Hegenbart U, Milani P, Kimmich C, Foli A, Ho AD, et al. A staging system for renal outcome and early markers of renal response to chemotherapy in AL amyloidosis. Blood. 2014;124:2325–32.
Huang X, Fu C, Chen L, Chen W, Ren G, Guo J, et al. Combination of bortezomib in the induction, conditioning and consolidation with autologous hematopoietic stem cell transplantation in patients with immunoglobulin light chain amyloidosis. Am J Hematol. 2019;94:E101–e4.
Shimizu Y, Hirai T, Ogawa Y, Yamada C, Kobayashi E. Characteristics of risk factors for acute kidney injury among inpatients administered sulfamethoxazole/trimethoprim: a retrospective observational study. J Pharm Health Care Sci. 2022;8:20.
Slater MB, Gruneir A, Rochon PA, Howard AW, Koren G, Parshuram CS. Identifying High-Risk Medications Associated with Acute Kidney Injury in Critically Ill Patients: A Pharmacoepidemiologic Evaluation. Paediatr Drugs. 2017;19:59–67.
Zavras P, Su Y, Fang J, Stern A, Gupta N, Tang Y, et al. Impact of Preemptive Therapy for Cytomegalovirus on Toxicities after Allogeneic Hematopoietic Cell Transplantation in Clinical Practice: A Retrospective Single-Center Cohort Study. Biol Blood Marrow Transplant. 2020;26:1482–91.
Lilly CM, Welch VL, Mayer T, Ranauro P, Meisner J, Luke DR. Evaluation of intravenous voriconazole in patients with compromised renal function. BMC Infect Dis. 2013;13:14.
Melphalan. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012.
Alix JL, Swiercz P, Schaerer R, Mousseau M, Cordonnier D, Couderc P.et al. [Nephrotoxicity of high-dose melphalan]. Presse Med. 1983;12:575–6.
Spencer A, Horvath N, Gibson J, Prince HM, Herrmann R, Bashford J, et al. Prospective randomised trial of amifostine cytoprotection in myeloma patients undergoing high-dose melphalan conditioned autologous stem cell transplantation. Bone Marrow Transplant. 2005;35:971–7.
Abidi MH, Agarwal R, Tageja N, Ayash L, Deol A, Al-Kadhimi Z, et al. A phase I dose-escalation trial of high-dose melphalan with palifermin for cytoprotection followed by autologous stem cell transplantation for patients with multiple myeloma with normal renal function. Biol Blood Marrow Transplant. 2013;19:56–61.
Gutiérrez-García G, Rovira M, Magnano L, Rosiñol L, Bataller A, Suárez-Lledó M, et al. Innovative strategies minimize engraftment syndrome in multiple myeloma patients with novel induction therapy following autologous hematopoietic stem cell transplantation. Bone Marrow Transplant. 2018;53:1541–7.
Liu Z, Zhang S, Horn B, Moreb JS. Postautologous stem cell transplantation engraftment syndrome: Improved treatment and outcomes. Clin Transplant. 2020;34:e13797.
McCoy IE, Chertow GM. AKI-A Relevant Safety End Point? Am J Kidney Dis. 2020;75:508–12.
Meyrier A, Niaudet P. Acute kidney injury complicating nephrotic syndrome of minimal change disease. Kidney Int. 2018;94:861–9.
Parikh CR, Coca SG. Acute kidney injury: defining prerenal azotemia in clinical practice and research. Nat Rev Nephrol. 2010;6:641–2.
Kellum JA, Romagnani P, Ashuntantang G, Ronco C, Zarbock A, Anders HJ. Acute kidney injury. Nat Rev Dis Primers. 2021;7:52.
Romagnani P, Remuzzi G, Glassock R, Levin A, Jager KJ, Tonelli M, et al. Chronic kidney disease. Nat Rev Dis Primers. 2017;3:17088.
Joslin J, Wilson H, Zubli D, Gauge N, Kinirons M, Hopper A, et al. Recognition and management of acute kidney injury in hospitalised patients can be partially improved with the use of a care bundle. Clin Med (Lond). 2015;15:431–6.
Mehta RL, Cerda J, Burdmann EA, Tonelli M, Garcia-Garcia G, Jha V, et al. International Society of Nephrology’s 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385:2616–43.
Brown JR, Kramer RS, Coca SG, Parikh CR. Duration of acute kidney injury impacts long-term survival after cardiac surgery. Ann Thorac Surg. 2010;90:1142–8.
Coca SG, King JT Jr., Rosenthal RA, Perkal MF, Parikh CR. The duration of postoperative acute kidney injury is an additional parameter predicting long-term survival in diabetic veterans. Kidney Int. 2010;78:926–33.
Author information
Authors and Affiliations
Contributions
WWX was responsible for designing the study, extracting and analyzing data, interpreting results and writing the manuscript. WCC, JZG, LZ, GSR collected the data of the subjects. XHH was responsible for designing the protocol, interpreting results, and helped perform the analysis with constructive discussions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, W., Chen, W., Guo, J. et al. Acute kidney injury during autologous stem cell transplantation in light chain amyloidosis with kidney involvement and their impact on prognosis. Bone Marrow Transplant (2024). https://doi.org/10.1038/s41409-024-02292-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41409-024-02292-5
- Springer Nature Limited