Abstract
Background: Failure of the cephalic venous approach in pacemaker and defibrillator implantation is always due to the small size and difficulty in isolation of the cephalic vein. We propose that pre-procedure imaging of the proximal cephalic vein is valuable to achieve successful access of cephalic vein. However, the feasibility and accuracy of duplex ultrasonographic imaging of the proximal cephalic vein are unknown.
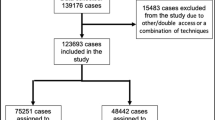
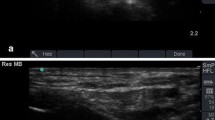
Methods: The study enrolled 30 consecutive patients who underwent new implantation of permanent pacemakers or defibrillators at our institute. An ultrasound probe scanned along the plane 2 cm beneath the inferior margin of the clavicle to locate the cephalic vein before device implantation. If the vein was well visualized, the venous diameter and the vertical depth were measured. The corresponding surface location of the vein on the chest wall was also identified and recorded by duplex ultrasonography. The echo-derived vertical depths and vascular findings were compared with those measured during surgery.
Results: All proximal cephalic veins were well visualized in the infraclavicular region by duplex ultrasonography. They were compressible, patent in color Doppler ultrasound imaging, and displayed phasic change of Doppler signal during respiration, indicating patency in all study veins. The average diameter of the target cephalic vein was 7.7 ± 1.6 mm (range, 5.0–11.1 mm). The echo-derived vertical depth of the proximal cephalic veins was highly correlated with the depth measured during surgery (28.4 ± 5.5 vs. 28.4 ± 5.6 mm, r = 0.93, P < 0.0001). All target cephalic veins were isolated after exploration via the estimated surface location of the chest wall by pre-procedure duplex ultrasonography. Seven (23%) of the studied patients did not have their cephalic vein cannulated successfully.
Conclusion: The target proximal cephalic vein in pacemaker and defibrillator implantation can be precisely imaged and localized by duplex ultrasonography. Although further studies are needed, our findings pave a way to further study and clarify the implantation problems of cephalic vein approach.
Similar content being viewed by others
References
Knight BP, Curlett K, Oral H, Pelosi F, Morady F, Strickberger SA. Clinical predictors of successful cephalic vein access for implantation of endocardial leads. J Interv Card Electrophysiol 2002;7:177-180.
Furman S. Venous cutdown for pacemaker implantation. Ann Thorac Surg 1986;41:438-439.
Gallik DM, Ben-zur UM, Gross JN, Furman S. Lead fracture in cephalic versus subclavian approach with transvenous implantable cardioverter defibrillator systems. Pacing Clin Electrophysiol 1996;19:1089-1094.
Gordon PJ, Pak A, Salerno TA, Lajos TZ. Pacemaker lead placement via a small cephalic vein. Ann Thorac Surg 1996;62:594-595.
Littleford PO, Parsonnet V, Specor SD. Method for the rapid and atraumatic insertion of permanent endocardial pacemaker electrodes through the subclavian vein. Am J Cardiol 1979;43:980-982.
Parsonnet V, Roelke M. The cephalic vein cutdown versus subclavian puncture for pacemaker/ICD lead implantation. Pacing Clin Electrophysiol 1999;22:695-697.
Furman S. Subclavian puncture for pacemaker lead replacement. Pacing Clin Electrophysiol 1986;9:467.
Calkins H, Ramza BM, Brinker J, Atiga W, Donahue K, Nsah E, Taylor E, Halperin H, Lawrence JH, Tomaselli G, Berger RD. Prospective randomized comparison of the safety and effectiveness of placement of endocardial pacemaker and defibrillator leads using the extrathoracic subclavian vein guided by contrast venography versus the cephalic approach. Pacing Clin Electrophysiol 2001;24:456-464.
Da Costa A, Faure E, Romeyer C, Samuel B, Messier M, Lamaud M, Isaaz K. Safe and effective placement of two bipolar silicone leads in the cephalic vein using a hydrophilic guidewire and a split introducer. Pacing Clin Electrophysiol 2000;23:2065-2067.
Tse HF, Lau CP, Leung SK. A cephalic vein cutdown and venography technique to facilitate pacemaker and defibrillator lead implantation. Pacing Clin Electrophysiol 2001;24:496-473.
De Rosa F, Talarico A, Mancuso P, Plastina F. New introducer technique for implanting pacemakers and defibrillator leads: Percutaneous incannulaion of the cephalic vein. G Ital Cardiol 1998;28:1094-1098.
Shimada H, Hoshino K, Yuki M, Sakurai S, Owa M. Percutaneous cephalic vein approach for permanent pacemaker implantation. Pacing Clin Electrophysiol 1999;22:1499-1501.
Ong LS, Barold SS, Lederman M, Falkoff MD, Heinle RA. Cephalic vein guide wire technique for implantation of permanent pacemakers. Am Heart J 1987;114:753-756.
Dwivedi SK, Narain VS, Dhawan S, Soni D, Hasan M. Modified cephalic vein guide wire technique for permanent pacemaker implantation. Indian Heart J 1992;44:87-89.
Comerota AJ, Katz ML, Hashemi HA. Venous duplex imaging for the diagnosis of acute deep venous thrombosis. Haemostasis 1993;23(suppl 1):61-71.
Joynt GM, Kew J, Gomersall CD, Leung VY, Liu EK. Deep vein thrombosis caused by femoral venous catheters in critically ill adult patients. Chest 2000;117:178-183.
Hughes P, Scott C, Bodenham A. Ultrasonography of the femoral vessels in the groin: Implications for vascular access. Anaesthesia 2000;55:1192-1212.
Killewich LA, Bedford GR, Beach KW, Strandness DE Jr. Diagnosis of deep vein thrombosis. A prospective study comparing duplex scanning to contrast venography. Circulation 1989;79:810-814.
Luciani A, Clement O, Halimi P, Goudot D, Portier F, Bassot V, Luciani J-A, Avan P, Frija G, Bonfils P. Catheter-related upper extremity deep venous thrombosis in cancer patients: A prospective study based on Doppler US. Radiology 2001;220:655-660.
Huber TS, Ozaki CK, Flynn TC, Lee WA, Berceli SA, Hirneise CM, Carlton LM, Carter JW, Ross EA, Seeger JM. Prospective validation of an algorithm to maximize native arteriovenous fistulae for chronic hemodialysis access. J Vasc Surg 2002;36:452-459.
Ascher E, Hingoran A, Gunduz Y, Yorkovich Y, Ward M, Miranda J, Tsemekhin B, Kleiner M, Greenberg S. The value and limitations of the arm cephalic and basilic vein for arteriovenous access. Ann Vasc Surg 2001;15:89-97.
Sivanesan S, How TV, Barkran A. Sites of stenosis in AV fistulae for hemodialysis access. Nephrol Dial Transplant 1999;14:118-120.
Byrd CL. Safe introducer technique for pacemaker lead implantation. Pacing Clin Electrophysiol 1992;15:1355-1356.
Hsiao HC, Kong CW, Wang JJ, Chan WL, Wang SP, Chang MS, Chiang BN. Right ventricular electrode lead implantation via a persistent left superior vena cava. An improved technique. Angiology 1997;48:919-923.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, JY., Chang, KC., Lin, YC. et al. Feasibility and Accuracy of Pre-procedure Imaging of the Proximal Cephalic Vein by Duplex Ultrasonography in Pacemaker and Defibrillator Implantation. J Interv Card Electrophysiol 10, 31–35 (2004). https://doi.org/10.1023/B:JICE.0000011482.58569.74
Issue Date:
DOI: https://doi.org/10.1023/B:JICE.0000011482.58569.74