Abstract
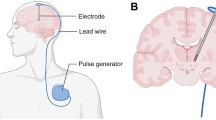
Deep brain stimulation of nuclei in the basal ganglia has been recognized as the most effective neurosurgical therapy for hypokinesia in patients with Parkinson’s disease; however, the mechanism underlying its curative effect remains unknown. In addition, the known effects of the two major pathways of the basal ganglia on the thalamus can offer information on optimal targets for further exploration and research. To simulate high-frequency stimulation to the different targets in Parkinson’s disease, a cortico-basal-thalamic network model was constructed based on the biological principles of anatomical structures and utilization of conductance-based models. Taking three different nucleus regions as targets, we simulated and analyzed the diversity of different stimulus durations and periods, along with stimulus efficacy, for the three targets. Then, by adopting different stimulus magnitudes that acted on the three targets, a comparative analysis of the effects of different stimulus magnitudes and targets for the treatment of Parkinson’s disease was performed. To identify the optimal target, different effects of the two major pathways on the thalamus were calculated. The calculation results show that the cortico-basal-thalamic network is reliable, and through the use of feasible models, high-frequency stimulation of the three targets can improve the pathological thalamic rhythmicity. It is shown that the direct pathway excites the thalamus, while the indirect pathway plays a regulatory role in the thalamus.









Similar content being viewed by others
References
Shou, T. D. (2001). Neurobiology. Beijing: Higher Education Press.
Gurney, K., Prescott, T. J., Wickens, J. R., & Redgrave, P. (2004). Computational models of the basal ganglia: From robots to membranes. Trends in Neurosciences, 27(8), 453–459.
Sakas, D. E. (2007). Operative neuromodulation: Neural networks surgery (Vol. 2). Vienna: Springer.
Mink, J. W., & Thach, W. T. (1993). Basal ganglia intrinsic circuits and their role in behavior. Current Opinion in Neurobiology, 3(3), 950–957.
Narayanan, S. (2003). The role of cortico-basal-thalamic loops in cognition: a computational model and preliminary results. Neurocomputing, 52–54(02), 605–614.
Groenewegen, H. J. (2003). The basal ganglia and motor control. Neural Plasticity, 10(1–2), 107–120.
Mao, Z. H., & Massaquoi, S. G. (2007). Dynamics of winner-take-all competition in recurrent neural networks with lateral inhibition. IEEE Transactions on Neural Networks, 18(1), 55–69.
Middleton, F. A., & Strick, P. L. (2000). Basal ganglia and cerebellar loops: motor and cognitive circuits. Brain Research Reviews, 31(2–3), 236–250.
Wichmann, T., & DeLong, M. R. (2012). The basal ganglia. In E. R. Kandel, J. H. Schwartz, T. M. Jessell, S. A. Siegelbaum, & A. J. Hudspeth (Eds.), Principles of neural sciences (Vol. 5, pp. 982–998). New York: McGraw-Hill Professional.
Moro, E., & Lang, A. E. (2006). Criteria for deep-brain stimulation in Parkinson’s disease: review and analysis. Expert Review of Neurotherapeutics, 6(11), 1695–1705.
Apetauerova, D., Ryan, R. K., Ro, S. I., Arle, J., Shils, J., Papavassiliou, E., et al. (2006). End of day dyskinesia in advanced Parkinson’s disease can be eliminated by bilateral subthalamic nucleus or globus pallidus deep brain stimulation. Movement Disorders, 21(8), 1277–1279.
Lozano, A. M., Snyder, B. J., Clement, H., Hutchison, W. D., & Dostrovsky, J. O. (2010). Basal ganglia physiology and deep brain stimulation. Movement Disorders, 25(S1), S71–S75.
Kreitzer, A., & Malenka, R. (2008). Striatal plasticity and basal ganglia circuit function. Neuron, 60(4), 543–554.
Hutchison, W. D., Dostrovsky, J. O., Walters, J. R., Courtemanche, R., Boraud, T., Goldberg, J., et al. (2004). Neuronal oscillations in the basal ganglia and movement disorders: evidence from whole animal and human recordings. Journal of Neuroscience, 24(42), 9240–9243.
Boraud, T., Bezard, E., Bioulac, B., & Gross, C. E. (2002). From single extracellular unit recording in experimental and human Parkinsonism to the development of a functional concept of the role played by the basal ganglia in motor control. Progress in Neurobiology, 66(4), 265–283.
Easton, N., Marshall, F., Fone, K., & Marsden, C. (2007). Atomoxetine produces changes in cortico-basal thalamic loop circuits: assessed by phMRI BOLD contrast. Neuropharmacology, 52(3), 812–826.
Rosin, B., Nevet, A., Elias, S., Rivlin-Etzion, M., Israel, Z., & Bergman, H. (2007). Physiology and pathophysiology of the basal ganglia—thalamo—cortical networks. Parkinsonism Related Disorders, 13(Suppl 3), S437–S439.
Yelnik, J. (2002). Functional anatomy of the basal ganglia. Movement Disorders, 17(S3), S15–S21.
Farries, M. A., Meitzen, J., & Perkel, D. J. (2005). Electrophysiological properties of neurons in the basal ganglia of the domestic chick: conservation and divergence in the evolution of the avian basal ganglia. Journal of Neurophysiology, 94(1), 454–467.
Wolf, J. A., Moyer, J. T., Lazarewicz, M. T., Contreras, D., Benoit-Marand, M., O’Donnell, P., et al. (2005). NMDA/AMPA ratio impacts state transitions and entrainment to oscillations in a computational model of the nucleus accumbens medium spiny projection neuron. Journal of Neuroscience, 25(40), 9080–9095.
Steephen, J. E., & Manchanda, R. (2009). Differences in biophysical properties of nucleus accumbens medium spiny neurons emerging from inactivation of inward rectifying potassium currents. Journal of Computational Neuroscience, 27(3), 453–470.
John, J., & Manchanda, R. (2011). Modulation of synaptic potentials and cell excitability by dendritic KIR and KAs channels in nucleus accumbens medium spiny neurons: a computational study. Journal of Biosciences, 36(2), 309–328.
Pospischil, M., Toledo-Rodriguez, M., Monier, C., Piwkowska, Z., Bal, T., Frégnac, Y., et al. (2008). Minimal Hodgkin-Huxley type models for different classes of cortical and thalamic neurons. Biological Cybernetics, 99(4–5), 427–441.
Rubin, J. E., & Terman, D. (2004). High frequency stimulation of the subthalamic nucleus eliminates pathological thalamic rhythmicity in a computational model. Journal of Computational Neuroscience ,16(3), 211–235.
Migliore, M., Cannia, C., & Canavier, C. C. (2008). A modeling study suggesting a possible pharmacological target to mitigate the effects of ethanol on reward-related dopaminergic signaling. Journal of Neurophysiology, 99(5), 2703–2707.
Wang, L., & Liu, S. Q. (2011). Neural circuit and its functional roles in cerebellar cortex. Neuroscience Bulletin, 27(3), 173–184.
Gu, H. G. (2013). Experimental observation of transition from chaotic bursting to chaotic spiking in a neural pacemaker. Chaos, 23(2), 295–308.
Chen, S. D. (2006). Parkinson Disease. Beijing: People’s Medical Publishing House.
Lehéricy, S., Bardinet, E., Tremblay, L., Pf, V. D. M., Pochon, J. B., Dormont, D., et al. (2006). Motor control in basal ganglia circuits using fMRI and brain atlas approaches. Cerebral Cortex, 16(2), 149–161.
Larson, P. S. (2014). Deep brain stimulation for movement disorders. Journal of the American Society for Experimental Neurotherapeutics, 11(3), 465–474.
Blomstedt, P., Fytagoridis, A., Åström, M., Linder, J., Forsgren, L., & Hariz, M. I. (2012). Unilateral caudal zona incerta deep brain stimulation for Parkinsonian tremor. Parkinsonism & Related Disorders, 18(10), 1062–1066.
Plaha, P., Benshlomo, Y., Patel, N. K., & Gill, S. S. (2006). Stimulation of the caudal zona incerta is superior to stimulation of the subthalamic nucleus in improving contralateral parkinsonism. Brain, 129(1), 1732–1747.
Kitagawa, M., Murata, J., Uesugi, H., Kikuchi, S., Saito, H., Tashiro, K., et al. (2005). Two-year follow-up of chronic stimulation of the posterior subthalamic white matter for tremor-dominant Parkinson’s disease. Neurosurgery, 56(2), 281–289.
Acknowledgments
This work was supported by the National Natural Science Foundation of China under Grant 11572127 and 11172103.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Here, we describe the direct and indirect pathways internal synaptic connection strengths and external stimuli.
In the direct pathway, synaptic connection strengths are g N(PY→D1) = 0.02196, g A(PY→D1) = 1.134, g G(D1→GPi) = 26.265, g N(DA→D1) = 0.0488, g A(DA→D1) = 0.252, and g G(GPi→TH) = 0.85 μS. External stimuli are I S(DA) = 0.3 and I S(GPi) = −3.74 nA. In the indirect pathway, the internal connection strengths are g N(PY→D2) = 0.03172, g A(PY→D2) = 0.1638, g N(PY→STN) = 10.5, g A(PY→STN) = 3.15, g G(DA→D2) = 0.34, g G(D2→GPe) = 0.425, g G(GPe→STN) = 8.5, g N(STN→GPi) = 0.0122, g A(STN→GPi) = 0.063, and g G(GPi→TH) = 0.425 μS. The external stimuli are I S(DA) = 0.3, I S(GPe) = −1.5, and I S(GPi) = −4.0 nA. For g syn(x→y) , syn indicates the type of synapse and (N, A, G = NMDA, AMPA, GABA), x → y indicates that neuron y was affected by synapses that came from neuron x. I S(X) indicates that neuron X incurred an external stimulus.
Rights and permissions
About this article
Cite this article
Jiang, X., Liu, S., Lu, B. et al. High-Frequency Stimulation for Parkinson’s Disease and Effects on Pathways in Basal Ganglia Network Model. J. Med. Biol. Eng. 36, 704–717 (2016). https://doi.org/10.1007/s40846-016-0170-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40846-016-0170-8