Abstract
Purpose of Review
Sleep is a physiological process characterized by a crucial interaction between behavioural and neurobiological aspects, thereby directly influencing mental functionality. The present work aims at providing an overview of the structure, topological distribution, and functions of the sleep slow oscillation (< 1 Hz), and at attempting to unveil how the mechanisms underlying its properties are altered in several mental disorders.
Recent Findings
Slow wave sleep and especially the sleep slow oscillation appear to regulate essential mechanisms at the basis of neuronal and synaptic health, such as an efficient functional connectivity, brain plasticity, memory consolidation, metabolic clearance, and sleep maintenance. Alterations of these functions can be observed at various levels in a wide range of mental disorders, ranging from insomnia to overt psychiatric disorders.
Summary
We propose a guidance for research and clinical practice related to the sleep slow oscillation, considering the lack of clinical emphasis on this wave and highlighting the potential benefits of its direct non-invasive modulation. In this framework, we propose that targeting insomnia would be crucial for mental health by regulating the sleep slow oscillation.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Majde JA, Krueger JM. Links between the innate immune system and sleep. J Allergy Clin Immunol. 2005;116:1188–98.
Siclari F, Tononi G (2016) Chapter 7 — sleep and dreaming. In: Laureys S, Gosseries O, Tononi G (eds) Neurol. Conciousness Second Ed. Academic Press, San Diego, pp 107–128
• Palagini L, Hertenstein E, Riemann D, Nissen C. Sleep, insomnia and mental health. J Sleep Res. 2022;31:e13628. This review highlights how insomnia disorder represents a transdiagnostic symptom for many psychiatric disorders, as well as marker of disrupted neuroplasticity and dysregulation of different neurobiological mechanisms involved in several mental conditions. In this framework, treating insomnia may offer new future directions for integrated and non-pharmacological treatments of psychiatric disorders.
Tubbs AS, Dollish HK, Fernandez F, Grandner MA. Chapter 1 — the basics of sleep physiology and behavior. In: Grandner MA, editor. Sleep Health. Academic Press; 2019. p. 3–10.
Xiao X, Rui Y, Jin Y, Chen M. Relationship of sleep disorder with neurodegenerative and psychiatric diseases: an updated review. Neurochem Res. 2023. https://doi.org/10.1007/s11064-023-04086-5.
• Appelbaum LG, Shenasa MA, Stolz L, Daskalakis Z. Synaptic plasticity and mental health: methods, challenges and opportunities. Neuropsychopharmacology. 2023;48:113–20. This review comprehensively explores the mechanisms of neural plasticity and provides insights into the historical progression and future directions of techniques enabling the imaging of synaptic changes associated with psychiatric disorders. The review also emphasizes emerging therapeutics and discusses the challenges and opportunities in this rapidly evolving field of study.
Purves D, Augustine GJ, Fitzpatrick D, Katz LC, LaMantia A-S, McNamara JO, Williams SM (2001) Stages of Sleep. Neurosci. 2nd Ed.
Tononi G, Cirelli C. Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron. 2014;81:12–34.
Genzel L, Kroes MCW, Dresler M, Battaglia FP. Light sleep versus slow wave sleep in memory consolidation: a question of global versus local processes? Trends Neurosci. 2014;37:10–9.
Steriade M, Nuñez A, Amzica F. A novel slow (< 1 Hz) oscillation of neocortical neurons in vivo: depolarizing and hyperpolarizing components. J Neurosci Off J Soc Neurosci. 1993;13:3252–65.
Murphy M, Riedner BA, Huber R, Massimini M, Ferrarelli F, Tononi G. Source modeling sleep slow waves. Proc Natl Acad Sci. 2009;106:1608–13.
Menicucci D, Piarulli A, Allegrini P, Laurino M, Mastorci F, Sebastiani L, Bedini R, Gemignani A. Fragments of wake-like activity frame down-states of sleep slow oscillations in humans: new vistas for studying homeostatic processes during sleep. Int J Psychophysiol. 2013;89:151–7.
Gemignani A, Menicucci D, Laurino M, Piarulli A, Mastorci F, Sebastiani L, Allegrini P. Linking Sleep Slow Oscillations with consciousness theories: new vistas on Slow Wave Sleep unconsciousness. Arch Ital Biol. 2015;153:135–43.
Menicucci D, Piarulli A, Laurino M, Zaccaro A, Agrimi J, Gemignani A. Sleep slow oscillations favour local cortical plasticity underlying the consolidation of reinforced procedural learning in human sleep. J Sleep Res. 2020;29:e13117.
Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, Reynolds CF III, Riemann D. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. 2016;142:969–90.
Laurino M, Menicucci D, Piarulli A, Mastorci F, Bedini R, Allegrini P, Gemignani A. Disentangling different functional roles of evoked K-complex components: mapping the sleeping brain while quenching sensory processing. Neuroimage. 2014;86:433–45.
Crunelli V, Hughes SW. The slow (<1 Hz) rhythm of non-REM sleep: a dialogue between three cardinal oscillators. Nat Neurosci. 2010;13:9–17.
Gemignani A, Laurino M, Provini F, et al. Thalamic contribution to Sleep Slow Oscillation features in humans: a single case cross sectional EEG study in Fatal Familial Insomnia. Sleep Med. 2012;13:946–52.
Menicucci D, Piarulli A, Debarnot U, d’Ascanio P, Landi A, Gemignani A. Functional structure of spontaneous sleep slow oscillation activity in humans. PLoS ONE. 2009;4:e7601.
Yoshida K, Shi S, Ukai-Tadenuma M, Fujishima H, Ohno R, Ueda HR. Leak potassium channels regulate sleep duration. Proc Natl Acad Sci. 2018;115:E9459–68.
Ode KL, Katsumata T, Tone D, Ueda HR. Fast and slow Ca2+-dependent hyperpolarization mechanisms connect membrane potential and sleep homeostasis. Curr Opin Neurobiol. 2017;44:212–21.
Steriade M. Grouping of brain rhythms in corticothalamic systems. Neuroscience. 2006;137:1087–106.
Marshall L, Helgadóttir H, Mölle M, Born J. Boosting slow oscillations during sleep potentiates memory. Nature. 2006;444:610–3.
Rasch B, Born J. About sleep’s role in memory. Physiol Rev. 2013;93:681–766.
Mölle M, Bergmann TO, Marshall L, Born J. Fast and slow spindles during the sleep slow oscillation: disparate coalescence and engagement in memory processing. Sleep. 2011;34:1411–21.
Helfrich RF, Lendner JD, Mander BA, Guillen H, Paff M, Mnatsakanyan L, Vadera S, Walker MP, Lin JJ, Knight RT. Bidirectional prefrontal-hippocampal dynamics organize information transfer during sleep in humans. Nat Commun. 2019;10:3572.
Halonen R, Kuula L, Lahti J, Räikkönen K, Pesonen A-K. The association between overnight recognition accuracy and slow oscillation-spindle coupling is moderated by BDNF Val66Met. Behav Brain Res. 2022;428:113889.
Cash SS, Halgren E, Dehghani N, et al. The human K-complex represents an isolated cortical down-state. Science. 2009;324:1084–7.
Sanchez-Vives MV, Mattia M, Compte A, Perez-Zabalza M, Winograd M, Descalzo VF, Reig R. Inhibitory modulation of cortical up states. J Neurophysiol. 2010;104:1314–24.
Jenkins JG, Dallenbach KM. Obliviscence during sleep and waking. Am J Psychol. 1924;35:605–12.
Huber R, Felice Ghilardi M, Massimini M, Tononi G. Local sleep and learning. Nature. 2004;430:78–81.
• Menicucci D, Lunghi C, Zaccaro A, Morrone MC, Gemignani A. Mutual interaction between visual homeostatic plasticity and sleep in adult humans. ELife. 2022;11:e70633. The authors report a correlation between individual susceptibility to visual homeostatic plasticity after deprivation and the changes in occipital sleep slow oscillations and spindle power, in line with a slow-wave sleep-driven modulation occurring in the early occipital visual cortex.
Rozov AV, Valiullina FF, Bolshakov AP. Mechanisms of long-term plasticity of hippocampal GABAergic synapses. Biochem Mosc. 2017;82:257–63.
Bliss TVP, Lømo T. Long-lasting potentiation of synaptic transmission in the dentate area of the anaesthetized rabbit following stimulation of the perforant path. J Physiol. 1973;232:331–56.
Vinogradova OS. Hippocampus as comparator: role of the two input and two output systems of the hippocampus in selection and registration of information. Hippocampus. 2001;11:578–98.
Yang G, Lai CSW, Cichon J, Ma L, Li W, Gan W-B. Sleep promotes branch-specific formation of dendritic spines after learning. Science. 2014;344:1173–8.
Aton SJ, Suresh A, Broussard C, Frank MG. Sleep promotes cortical response potentiation following visual experience. Sleep. 2014;37:1163–70.
Timofeev I, Chauvette S. Sleep slow oscillation and plasticity. Curr Opin Neurobiol. 2017;44:116–26.
Bushey D, Tononi G, Cirelli C. Sleep and synaptic homeostasis: structural evidence in Drosophila. Science. 2011;332:1576–81.
Vyazovskiy VV, Cirelli C, Pfister-Genskow M, Faraguna U, Tononi G. Molecular and electrophysiological evidence for net synaptic potentiation in wake and depression in sleep. Nat Neurosci. 2008;11:200–8.
Autry AE, Monteggia LM. Brain-derived neurotrophic factor and neuropsychiatric disorders. Pharmacol Rev. 2012;64:238–58.
Kossel AH, Cambridge SB, Wagner U, Bonhoeffer T. A caged Ab reveals an immediate/instructive effect of BDNF during hippocampal synaptic potentiation. Proc Natl Acad Sci U S A. 2001;98:14702–7.
Faraguna U, Vyazovskiy VV, Nelson AB, Tononi G, Cirelli C. A causal role for brain-derived neurotrophic factor in the homeostatic regulation of sleep. J Neurosci Off J Soc Neurosci. 2008;28:4088–95.
Kang H, Schuman EM. Long-lasting neurotrophin-induced enhancement of synaptic transmission in the adult hippocampus. Science. 1995;267:1658–62.
Knipper M, da Penha BM, Blöchl A, Breer H, Thoenen H, Lindholm D. Positive feedback between acetylcholine and the neurotrophins nerve growth factor and brain-derived neurotrophic factor in the rat hippocampus. Eur J Neurosci. 1994;6:668–71.
Sala R, Viegi A, Rossi FM, Pizzorusso T, Bonanno G, Raiteri M, Maffei L. Nerve growth factor and brain-derived neurotrophic factor increase neurotransmitter release in the rat visual cortex. Eur J Neurosci. 1998;10:2185–91.
Wardle RA, Poo M. Brain-derived neurotrophic factor modulation of GABAergic synapses by postsynaptic regulation of chloride transport. J Neurosci Off J Soc Neurosci. 2003;23:8722–32.
Sale A, Maya Vetencourt JF, Medini P, Cenni MC, Baroncelli L, De Pasquale R, Maffei L. Environmental enrichment in adulthood promotes amblyopia recovery through a reduction of intracortical inhibition. Nat Neurosci. 2007;10:679–81.
Steriade M, Timofeev I, Grenier F. Natural waking and sleep states: a view from inside neocortical neurons. J Neurophysiol. 2001;85:1969–85.
Akaneya Y, Tsumoto T, Kinoshita S, Hatanaka H. Brain-derived neurotrophic factor enhances long-term potentiation in rat visual cortex. J Neurosci Off J Soc Neurosci. 1997;17:6707–16.
Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342. https://doi.org/10.1126/science.1241224.
Fultz NE, Bonmassar G, Setsompop K, Stickgold RA, Rosen BR, Polimeni JR, Lewis LD. Coupled electrophysiological, hemodynamic, and cerebrospinal fluid oscillations in human sleep. Science. 2019;366:628–31.
Varga AW, Wohlleber ME, Giménez S, et al. Reduced slow-wave sleep is associated with high cerebrospinal fluid Aβ42 levels in cognitively normal elderly. Sleep. 2016;39:2041–8.
Ju Y-ES, Ooms SJ, Sutphen C, et al. Slow wave sleep disruption increases cerebrospinal fluid amyloid-β levels. Brain. 2017;140:2104–11.
Lucey BP, McCullough A, Landsness EC, et al. Reduced non-rapid eye movement sleep is associated with tau pathology in early Alzheimer’s disease. Sci Transl Med. 2019;11:eaau6550.
Winer JR, Mander BA, Kumar S, Reed M, Baker SL, Jagust WJ, Walker MP. Sleep disturbance forecasts β-amyloid accumulation across subsequent years. Curr Biol. 2020;30:4291-4298.e3.
Lim MM, Gerstner JR, Holtzman DM. The sleep–wake cycle and Alzheimer’s disease: what do we know? Neurodegener Dis Manag. 2014;4:351–62.
Ju Y-ES, McLeland JS, Toedebusch CD, Xiong C, Fagan AM, Duntley SP, Morris JC, Holtzman DM. Sleep quality and preclinical Alzheimer disease. JAMA Neurol. 2013;70:587–93.
Yulug B, Hanoglu L, Kilic E. Does sleep disturbance affect the amyloid clearance mechanisms in Alzheimer’s disease? Psychiatry Clin Neurosci. 2017;71:673–7.
Krell-Roesch J, Syrjanen JA, Rakusa M, et al. Association of cortical and subcortical β-amyloid with standardized measures of depressive and anxiety symptoms in adults without dementia. J Neuropsychiatry Clin Neurosci. 2021;33:64–71.
Li P, Hsiao I-T, Liu C-Y, Chen C-H, Huang S-Y, Yen T-C, Wu K-Y, Lin K-J. Beta-amyloid deposition in patients with major depressive disorder with differing levels of treatment resistance: a pilot study. EJNMMI Res. 2017. https://doi.org/10.1186/s13550-017-0273-4.
Wegiel J, Frackowiak J, Mazur-Kolecka B, et al. Abnormal intracellular accumulation and extracellular Aβ deposition in idiopathic and Dup15q11.2-q13 autism spectrum disorders. PLOS ONE. 2012;7:e35414.
Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297:353–6.
Mander BA, Rao V, Lu B, Saletin JM, Lindquist JR, Ancoli-Israel S, Jagust W, Walker MP. Prefrontal atrophy, disrupted NREM slow waves, and impaired hippocampal-dependent memory in aging. Nat Neurosci. 2013;16:357–64.
Bennett ML, Viaene AN. What are activated and reactive glia and what is their role in neurodegeneration? Neurobiol Dis. 2021;148:105172.
Serrano-Pozo A, Muzikansky A, Gómez-Isla T, Growdon JH, Betensky RA, Frosch MP, Hyman BT. Differential relationships of reactive astrocytes and microglia to fibrillar amyloid deposits in Alzheimer disease. J Neuropathol Exp Neurol. 2013;72:462–71.
Troubat R, Barone P, Leman S, et al. Neuroinflammation and depression: a review. Eur J Neurosci. 2021;53:151–71.
Vallée A. Neuroinflammation in schizophrenia: the key role of the WNT/β-catenin pathway. Int J Mol Sci. 2022;23:2810.
Eissa N, Sadeq A, Sasse A, Sadek B. Role of neuroinflammation in autism spectrum disorder and the emergence of brain histaminergic system. Lessons Also for BPSD? Front Pharmacol. 2020;11. https://doi.org/10.3389/fphar.2020.00886.
Won E, Kim Y-K. Neuroinflammation-associated alterations of the brain as potential neural biomarkers in anxiety disorders. Int J Mol Sci. 2020;21:6546.
Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506.
Harvey AG, Murray G, Chandler RA, Soehner A. Sleep disturbance as transdiagnostic: consideration of neurobiological mechanisms. Clin Psychol Rev. 2011;31:225–35.
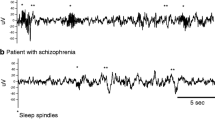
•• Hogan SE, Delgado GM, Hall MH, Nimgaonkar VL, Germain A, Buysse DJ, Wilckens KA. Slow-oscillation activity is reduced and high frequency activity is elevated in older adults with insomnia. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2020;16:1445–54. This study distinguished EEG subcomponents of slow-wave activity in the attempt of understanding the discrepancies found in insomnia disorders. The results highlighted that deficits in sleep EEG slow frequencies in insomnia are specific to the slow oscillations (<1 Hz).
Zhang J, Kendrick KM, Lu G. Feng J (2015) The fault lies on the other side: altered brain functional connectivity in psychiatric disorders is mainly caused by counterpart regions in the opposite hemisphere. Cereb Cortex N Y N. 1991;25:3475–86.
Baglioni C, Regen W, Teghen A, Spiegelhalder K, Feige B, Nissen C, Riemann D. Sleep changes in the disorder of insomnia: a meta-analysis of polysomnographic studies. Sleep Med Rev. 2014;18:195–213.
Aquino G, Benz F, Dressle RJ, Gemignani A, Alfì G, Palagini L, Spiegelhalder K, Riemann D, Feige B. Towards the neurobiology of insomnia: a systematic review of neuroimaging studies. Sleep Med Rev. 2024;73:101878.
Dulawa SC, Janowsky DS. Cholinergic regulation of mood: from basic and clinical studies to emerging therapeutics. Mol Psychiatry. 2019;24:694–709.
Palagini L, Baglioni C, Ciapparelli A, Gemignani A, Riemann D. REM sleep dysregulation in depression: state of the art. Sleep Med Rev. 2013;17:377–90.
Gillin JC, Sitaram N, Mendelson WB. Acetylcholine, sleep, and depression. Hum Neurobiol. 1982;1:211–9.
Riemann D, Joy D, Höchli D, Lauer C, Zulley J, Berger M. Influence of the cholinergic agonist RS 86 on normal sleep: sex and age effects. Psychiatry Res. 1988;24:137–47.
Steinberg EA, Wafford KA, Brickley SG, Franks NP, Wisden W. The role of K2p channels in anaesthesia and sleep. Pflugers Arch. 2015;467:907–16.
Yu H, Chen Z. The role of BDNF in depression on the basis of its location in the neural circuitry. Acta Pharmacol Sin. 2011;32:3–11.
Kaiser RH, Andrews-Hanna JR, Wager TD, Pizzagalli DA. Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiat. 2015;72:603–11.
Hager B, Yang AC, Brady R, Meda S, Clementz B, Pearlson GD, Sweeney JA, Tamminga C, Keshavan M. Neural complexity as a potential translational biomarker for psychosis. J Affect Disord. 2017;216:89–99.
Pijnenborg GHM, Larabi DI, Xu P, Hasson-Ohayon I, de Vos AE, Ćurčić-Blake B, Aleman A, Van der Meer L. Brain areas associated with clinical and cognitive insight in psychotic disorders: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2020;116:301–36.
Yang AC, Tsai S-J. Is mental illness complex? From behavior to brain. Prog Neuropsychopharmacol Biol Psychiatry. 2013;45:253–7.
Balu DT, Coyle JT. Neuroplasticity signaling pathways linked to the pathophysiology of schizophrenia. Neurosci Biobehav Rev. 2011;35:848–70.
Hull JV, Dokovna LB, Jacokes ZJ, Torgerson CM, Irimia A, Van Horn JD. Resting-state functional connectivity in autism spectrum disorders: a review. Front. Psychiatry. 2017;7. https://www.frontiersin.org/articles/10.3389/fpsyt.2016.00205.
Chellappa SL, Aeschbach D. Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev. 2022;61:101583.
Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, Nissen C. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. 2010;14:19–31.
Riemann D, Nissen C, Palagini L, Otte A, Perlis ML, Spiegelhalder K. The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. 2015;14:547–58.
Orff HJ. Neurobiology of insomnia as measured with FMRI. ProQuest Information & Learning. 2010.
Drummond SPA, Walker M, Almklov E, Campos M, Anderson DE, Straus LD. Neural correlates of working memory performance in primary insomnia. Sleep. 2013;36:1307–16.
Li Y, Liu L, Wang E, Zhang H, Dou S, Tong L, Cheng J, Chen C, Shi D. Abnormal neural network of primary insomnia: evidence from spatial working memory task fMRI. Eur Neurol. 2016;75:48–57.
Perrier J, Bruijel J, Naveau M, Ramautar J, Delcroix N, Coppens J, Lakbila-Kamal O, Stoffers D, Bessot N, Van Someren EJW. Functional connectivity correlates of attentional networks in insomnia disorder: a pilot study. J Sleep Res. 2022;e13796.
Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010;14:9–15.
Baglioni C, Nanovska S, Regen W, Spiegelhalder K, Feige B, Nissen C, Reynolds CF, Riemann D. Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol Bull. 2016;142:969–90.
Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. 2020;45:74–89.
Massimini M, Ferrarelli F, Esser SK, Riedner BA, Huber R, Murphy M, Peterson MJ, Tononi G. Triggering sleep slow waves by transcranial magnetic stimulation. Proc Natl Acad Sci. 2007;104:8496–501.
Eggert T, Dorn H, Sauter C, Nitsche MA, Bajbouj M, Danker-Hopfe H. No effects of slow oscillatory transcranial Direct Current Stimulation (tDCS) on sleep-dependent memory consolidation in healthy elderly subjects. Brain Stimulat. 2013;6:938–45.
Paßmann S, Külzow N, Ladenbauer J, Antonenko D, Grittner U, Tamm S, Flöel A. Boosting slow oscillatory activity using tDCS during early nocturnal slow wave sleep does not improve memory consolidation in healthy older adults. Brain Stimulat. 2016;9:730–9.
Bueno-Lopez A, Eggert T, Dorn H, Danker-Hopfe H. Slow oscillatory transcranial direct current stimulation (so-tDCS) during slow wave sleep has no effects on declarative memory in healthy young subjects. Brain Stimulat. 2019;12:948–58.
Saebipour MR, Joghataei MT, Yoonessi A, Sadeghniiat-Haghighi K, Khalighinejad N, Khademi S. Slow oscillating transcranial direct current stimulation during sleep has a sleep-stabilizing effect in chronic insomnia: a pilot study. J Sleep Res. 2015;24:518–25.
Author information
Authors and Affiliations
Contributions
G.A. and G.A. equally contributed to the composition of this work by writing the main manuscript text and preparing the figure and the table. L.P. conceived the idea for the review and supervised the writing of the manuscript. A.G. provided guidance in writing, conceptualization, planning and supervision. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
No animal or human subjects by the authors were used in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aquino, G., Alfì, G., Riemann, D. et al. Sleep is Essential for Mental Health: Potential Role of Slow Oscillations. Curr Sleep Medicine Rep 10, 13–22 (2024). https://doi.org/10.1007/s40675-024-00277-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40675-024-00277-w