Abstract
Background
The clinicopathological characteristics, treatment response and long-term outcome of immunoglobulin (Ig)A nephropathy with minimal change disease (MCD-IgAN) are not well defined.
Methods
Patients with biopsy-proven MCD-IgAN from the Jinling Hospital IgA nephropathy Registry were systematically reviewed and compared with those with IgA nephropathy without minimal change disease (Non-MCD-IgAN).
Results
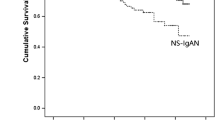
We compared data of 247 MCD-IgAN patients and 1,121 Non-MCD-IgAN patients. Compared to Non-MCD-IgAN, MCD-IgAN patients were younger,with male predominance, had higher levels of proteinuria, total cholesterol and estimated glomerular filtration rate (eGFR), lower incidence of hypertension and microhematuria, lower level of serum creatinine, and had less severe glomerular, tubulointerstitial and vascular lesions in renal pathology. In the Non-MCD-IgAN group, 157 patients (14.0 %) reached the renal endpoint and 103 patients (9.2 %) entered end-stage renal disease (ESRD). The 5-,10-, 15- and 20-year cumulative renal survival rates from ESRD, calculated by Kaplan–Meier method, were 95.0, 83.0, 72.9 and 65.4 %, respectively. In the MCD-IgAN group, no patients entered ESRD and only 4 (1.6 %) reached the renal endpoint. Patients with MCD-IgAN had a significantly better renal outcome than Non-MCD-IgAN (p < 0.01). At multivariate Cox analysis, proteinuria >1.0 g/day, hypertension, eGFR <60 ml/min/1.73 m2, hypoproteinemia and hyperuricemia were independent risk factors of renal survival for Non-MCD-IgAN patients [hazard ratio (HR) 3.43, p < 0.001; HR 1.65, p < 0.05; HR 2.61, p < 0.001; HR 2.40, p < 0.001; HR 2.27, p < 0.001, respectively), but not for patients with MCD-IgAN.
Conclusions
The long-term outcome of patients with MCD-IgAN is significantly better than that of patients with Non-MCD-IgAN.

Similar content being viewed by others
References
Koyama A, Igarashi M, Kobayashi M (1997) Natural history and risk factors for immunoglobulin A nephropathy in Japan. Research Group on Progressive Renal Diseases. Am J Kidney Dis 29:526–532
Le W, Liang S, Hu Y et al (2012) Long-term renal survival and related risk factors in patients with IgA nephropathy: results from a cohort of 1155 cases in a Chinese adult population. Nephrol Dial Transplant 27:1479–1485
Moriyama T, Itabashi M, Takei T et al (2015) High uric acid level is a risk factor for progression of IgA nephropathy with chronic kidney disease stage G3a. J Nephrol 28:451–456
Barbour SJ, Cattran DC, Kim SJ et al (2013) Individuals of Pacific Asian origin with IgA nephropathy have an increased risk of progression to end-stage renal disease. Kidney Int 84:1017–1024
Reich HN, Troyanov S, Scholey JW et al (2007) Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol 18:3177–3183
Donadio JV, Bergstralh EJ, Grande JP et al (2002) Proteinuria patterns and their association with subsequent end-stage renal disease in IgA nephropathy. Nephrol Dial Transplant 17:1197–1203
Tanaka K, Moriyama T, Iwasaki C et al (2015) Effect of hematuria on the outcome of IgA nephropathy with mild proteinuria. Clin Exp Nephrol 19:815–821
Le W, Liang S, Chen H et al (2014) Long-term outcome of IgA nephropathy patients with recurrent macroscopic hematuria. Am J Nephrol 40:43–50
Cattran DC, Coppo R, Cook HT et al (2009) The Oxford classification of IgA nephropathy: rationale, clinicopathological correlations, and classification. Kidney Int 76:534–545
Zeng CH, Le W, Ni Z et al (2012) A multicenter application and evaluation of the oxford classification of IgA nephropathy in adult chinese patients. Am J Kidney Dis 60:812–820
Barratt J, Feehally J (2005) IgA nephropathy. J Am Soc Nephrol 16:2088–2097
Lai KN, Lai FM, Ho CP et al (1986) Corticosteroid therapy in IgA nephropathy with nephrotic syndrome: a long-term controlled trial. Clin Nephrol 26:174–180
Cheng IK, Chan KW, Chan MK (1989) Mesangial IgA nephropathy with steroid-responsive nephrotic syndrome: disappearance of mesangial IgA deposits following steroid-induced remission. Am J Kidney Dis 14:361–364
Westhoff TH, Waldherr R, Loddenkemper C et al (2006) Mesangial IgA deposition in minimal change nephrotic syndrome: coincidence of different entities or variant of minimal change disease. Clin Nephrol 65:203–207
Barbiano DBG, Mazzucco G, Casanova S et al (1986) Steroid-sensitive nephrotic syndrome with mesangial IgA deposits: a separate entity? Observation of two cases. Am J Nephrol 6:141–145
Gallego N, Gonzalo A, Mampaso F et al (1988) Steroid-dependent nephrotic syndrome with minimal glomerular changes and mesangial IgA deposits. Child Nephrol Urol 9:98–100
Qin J, Yang Q, Tang X et al (2013) Clinicopathologic features and treatment response in nephrotic IgA nephropathy with minimal change disease. Clin Nephrol 79:37–44
Wang J, Juan C, Huang Q et al (2013) Corticosteroid therapy in IgA nephropathy with minimal change-like lesions: a single-centre cohort study. Nephrol Dial Transplant 28:2339–2345
Herlitz LC, Bomback AS, Stokes MB et al (2014) IgA nephropathy with minimal change disease. Clin J Am Soc Nephrol 9:1033–1039
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Waldman M, Crew RJ, Valeri A et al (2007) Adult minimal-change disease: clinical characteristics, treatment, and outcomes. Clin J Am Soc Nephrol 2:445–453
Szeto CC, Lai FM, Chow KM et al (2015) Long-term outcome of biopsy-proven minimal change nephropathy in Chinese adults. Am J Kidney Dis 65:710–718
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study formal consent is not required.
Funding
This study was funded by the National Basic Research Program of China 973 Program No.2012CB517600 (No. 2012CB517606) and the National Science Foundation of China (810-2010-8016).
Rights and permissions
About this article
Cite this article
Li, XW., Liang, SS., Le, WB. et al. Long-term outcome of IgA nephropathy with minimal change disease: a comparison between patients with and without minimal change disease. J Nephrol 29, 567–573 (2016). https://doi.org/10.1007/s40620-015-0242-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40620-015-0242-9