Abstract
Purpose
The incidence of papillary thyroid microcarcinoma is increasing. We evaluated the recurrence-free survival following total thyroidectomy and lobectomy to identify the optimal surgical choice.
Methods
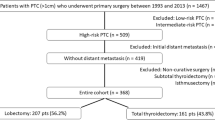
A meta-analysis was performed using the National Library of Medicine and the National Institutes of Health PubMed database to identify eligible studies. Summary 5- and 10-year RFS estimates after TT versus LT were calculated using random effects models.
Results
The literature search yielded 1117 studies (1990–2019). Nine studies met the inclusion criteria comprising 10,186 total thyroidectomy and 11,408 lobectomy patients. The 5-year recurrence-free survival was 98% [95% confidence interval (CI) 97–99%] after total thyroidectomy and 97% (95% CI 96–99%) after lobectomy, based on eight studies (9421 total thyroidectomy and 11,283 lobectomy patients); the 10-year recurrence-free survival was 95% (95% CI 92–98%) after total thyroidectomy and 92% (95% CI 86–96%) after lobectomy, based on eight studies (total thyroidectomy = 10,100, lobectomy = 11,389 patients).
Conclusion
The present meta-analysis demonstrates excellent, long-term recurrence-free survival following both total thyroidectomy and lobectomy surgery in patients with papillary thyroid microcarcinoma. The analysis also suggests that patients undergoing total thyroidectomy trended toward a slightly better long-term 10-year recurrence-free survival in comparison to patients undergoing lobectomy, a finding of potential, clinical significance in the management decision-making process.





Similar content being viewed by others
Availability of data and material
The authors confirm that the data supporting the findings of this study are publicly available without restriction; eligible studies were identified in The National Library of Medicine and the National Institutes of Health PubMed database.
References
Davies L, Welch HG (2014) Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg 140(4):317–322. https://doi.org/10.1001/jamaoto.2014.1
Kitahara CM, Sosa JA (2016) The changing incidence of thyroid cancer. Nat Rev Endocrinol 12(11):646–653. https://doi.org/10.1038/nrendo.2016.110
Lim H, Devesa SS, Sosa JA et al (2017) Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA 317(13):1338–1348. https://doi.org/10.1001/jama.2017.2719
Davies L, Welch HG (2006) Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA 295(18):2164–2167. https://doi.org/10.1001/jama.295.18.2164
Welch HG, Doherty GM (2018) Saving thyroids—overtreatment of small papillary cancers. N Engl J Med 379(4):310–312. https://doi.org/10.1056/NEJMp1804426
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1):1–133. https://doi.org/10.1089/thy.2015.0020
Loyo M, Tufano RP, Gourin CG (2013) National trends in thyroid surgery and the effect of volume on short-term outcomes. Laryngoscope 123(8):2056–2063. https://doi.org/10.1002/lary.23923
Hauch A, Al-Qurayshi Z, Randolph G et al (2014) Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol 21(12):3844–3852. https://doi.org/10.1245/s10434-014-3846-8
Macedo FI, Mittal VK (2015) Total thyroidectomy versus lobectomy as initial operation for small unilateral papillary thyroid carcinoma: a meta-analysis. Surg Oncol 24(2):117–122. https://doi.org/10.1016/j.suronc.2015.04.005
Zheng W, Li J, Lv P, Chen Z et al (2018) Treatment efficacy between total thyroidectomy and lobectomy for patients with papillary thyroid microcarcinoma: a systemic review and meta-analysis. Eur J Surg Oncol 44(11):1679–1684. https://doi.org/10.1016/j.ejso.2018.08.004
Wells GA, Shea B, O’Connell D et al (2020) The Newcastle–Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. University of Ottawa. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 13 Feb 2020
Stang A (2010) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim.1186
Ioannidis JP, Patsopoulos NA, Evangelou E (2007) Uncertainty in heterogeneity estimates in meta-analyses. BMJ 335(7626):914–916. https://doi.org/10.1136/bmj.39343.408449.80
Sterne JA, Sutton AJ, Ioannidis JP et al (2011) Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 343:d4002. https://doi.org/10.1136/bmj.d4002
Hay ID, Hutchinson ME, Gonzalez-Losada T et al (2008) Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery 144(6):980–987. https://doi.org/10.1016/j.surg.2008.08.035(discussion 7–8)
Gershinsky M, Barnett-Griness O, Stein N et al (2012) Total versus hemithyroidectomy for microscopic papillary thyroid cancer. J Endocrinol Invest 35(5):464–468. https://doi.org/10.3275/7963
Lee J, Park JH, Lee CR et al (2013) Long-term outcomes of total thyroidectomy versus thyroid lobectomy for papillary thyroid microcarcinoma: comparative analysis after propensity score matching. Thyroid 23(11):1408–1415. https://doi.org/10.1089/thy.2012.0463
Donatini G, Castagnet M, Desurmont T et al (2016) Partial thyroidectomy for papillary thyroid microcarcinoma: is completion total thyroidectomy indicated? World J Surg 40(3):510–515. https://doi.org/10.1007/s00268-015-3327-7
Dobrinja C, Pastoricchio M, Troian M et al (2017) Partial thyroidectomy for papillary thyroid microcarcinoma: is completion total thyroidectomy indicated? Int J Surg 41(Suppl 1):S34–S39. https://doi.org/10.1016/j.ijsu.2017.02.012
Kim SK, Park I, Woo JW et al (2017) Total thyroidectomy versus lobectomy in conventional papillary thyroid microcarcinoma: analysis of 8,676 patients at a single institution. Surgery 161(2):485–492. https://doi.org/10.1016/j.surg.2016.07.037
Kwon H, Jeon MJ, Kim WG et al (2017) A comparison of lobectomy and total thyroidectomy in patients with papillary thyroid microcarcinoma: a retrospective individual risk factor-matched cohort study. Eur J Endocrinol 176(4):371–378. https://doi.org/10.1530/EJE-16-0845
Choi JB, Lee WK, Lee SG et al (2018) Long-term oncologic outcomes of papillary thyroid microcarcinoma according to the presence of clinically apparent lymph node metastasis: a large retrospective analysis of 5,348 patients. Cancer Manag Res 10:2883–2891. https://doi.org/10.2147/CMAR.S173853
Xu Y, Xu L, Wang J (2018) Clinical predictors of lymph node metastasis and survival rate in papillary thyroid microcarcinoma: analysis of 3607 patients at a single institution. J Surg Res 221:128–134. https://doi.org/10.1016/j.jss.2017.08.007
Tuttle RM, Fagin JA, Minkowitz G et al (2017) Natural history and tumor volume kinetics of papillary thyroid cancers during active surveillance. JAMA Otolaryngol Head Neck Surg 143(10):1015–1020. https://doi.org/10.1001/jamaoto.2017.1442
Sakai T, Sugitani I, Ebina A et al (2019) Active surveillance for T1bN0M0 papillary thyroid carcinoma. Thyroid 29(1):59–63. https://doi.org/10.1089/thy.2018.0462
Ito Y, Miyauchi A, Oda H (2018) Low-risk papillary microcarcinoma of the thyroid: a review of active surveillance trials. Eur J Surg Oncol 44:307–315. https://doi.org/10.1016/j.ejso.2017.03.004
Leboulleux S, Tuttle RM, Pacini F et al (2016) Papillary thyroid microcarcinoma: time to shift from surgery to active surveillance? Lancet Diabetes Endocrinol 4(11):933–942. https://doi.org/10.1016/S2213-8587(16)30180-2
Molinaro E, Campopiano MC, Pieruzzi L et al (2020) Active surveillance in papillary thyroid microcarcinomas is feasible and safe: experience at a single Italian center. J Clin Endocrinol Metab 105(3):dgz113. https://doi.org/10.1210/clinem/dgz113
Tuttle RM, Haugen B, Perrier ND (2017) Updated American joint committee on cancer/tumor-node-metastasis staging system for differentiated and anaplastic thyroid cancer (eighth edition): what changed and why? Thyroid 27(6):751–756. https://doi.org/10.1089/thy.2017.0102
Mehanna H, Al-Maqbili T, Carter B et al (2014) Differences in the recurrence and mortality outcomes rates of incidental and nonincidental papillary thyroid microcarcinoma: a systematic review and meta-analysis of 21,329 person-years of follow-up. J Clin Endocrinol Metab 99(8):2834–2843. https://doi.org/10.1210/jc.2013-2118
Niemeier LA, Kuffner Akatsu H, Song C et al (2012) A combined molecular-pathologic score improves risk stratification of thyroid papillary microcarcinoma. Cancer 118(8):2069–2077. https://doi.org/10.1002/cncr.26425
Hu G, Zhu W, Yang W et al (2016) The effectiveness of radioactive iodine remnant ablation for papillary thyroid microcarcinoma: a systematic review and meta-analysis. World J Surg 40(1):100–109. https://doi.org/10.1007/s00268-015-3346-4
Kwon H, Jeon MJ, Kim WG et al (2017) Lack of efficacy of radioiodine remnant ablation for papillary thyroid microcarcinoma: verification using inverse probability of treatment weighting. Ann Surg Oncol 24(9):2596–2602. https://doi.org/10.1245/s10434-017-5910-7
Acknowledgements
The reported results in this manuscript were presented at the 89th Annual Meeting of the American Thyroid Association (2019).
Funding
This work was partially supported by a private donation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

40618_2020_1342_MOESM1_ESM.png
Supplementary file1 Supplementary figure 1: Funnel plot 5-year recurrence free survival- Total thyroidectomy (PNG 32 kb)


40618_2020_1342_MOESM3_ESM.png
Supplementary file3 Supplementary figure 3: Funnel plot 10-year recurrence free survival- Total thyroidectomy (PNG 30 kb)

Rights and permissions
About this article
Cite this article
van Gerwen, M., Alsen, M., Lee, E. et al. Recurrence-free survival after total thyroidectomy and lobectomy in patients with papillary thyroid microcarcinoma. J Endocrinol Invest 44, 725–734 (2021). https://doi.org/10.1007/s40618-020-01342-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40618-020-01342-1