Abstract
Background
Patients with Parkinson disease (PD) experience problems such as falls and freezing of gait during walking and turning in daily activities. However, few studies have examined the relationship between simultaneous turning tasks and the severity of PD.
Aim
To investigate turning characteristics in patients with PD using three-dimensional (3D) analysis during the timed up and go (TUG) test.
Methods
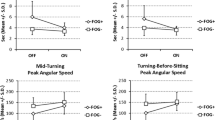
Thirty individuals performed the TUG test under 3D motion analysis: 10 patients with Hoehn and Yahr (H&Y) stages 2.5 and 3.0 PD (group I), 10 patients with H&Y stage 2.0 PD (group II), and 10 healthy older adult controls. Spatiotemporal and kinematic variables were analyzed during the TUG test with a Vicon 3-D motion analysis system.
Results
The walking speed, step length, step length asymmetry index, range of motion of the hip, knee, and shoulder joints, and foot clearance height significantly differed between patients with PD and the controls. The step length and foot clearance height were significantly different between groups I and II.
Discussion
The step length and foot clearance are different between the severity levels of PD, and the TUG test may be useful for identifying turning characteristics in patients with PD.
Conclusions
Patients with PD exhibited significant differences in all variables of interest compared to the controls. The step length and foot clearance height as well as the TUG test during the turning phase may be helpful for measuring turning in patients with different severity levels of PD.




Similar content being viewed by others
References
Camicioli R, Oken BS, Sexton G, Kaye JA, Nutt JG (1998) Verbal fluency task affects gait in Parkinson’s disease with motor freezing. J Geriatr Psychiatry Neurol 11:181–185
Morris S, Morris ME, Iansek R (2001) Reliability of measurements obtained with the Timed “Up & Go” test in people with Parkinson disease. Phys Ther 81:810–818
Crenna P, Carpinella I, Rabuffetti M, Calabrese E, Mazzoleni P, Nemni R, Ferrarin M (2007) The association between impaired turning and normal straight walking in Parkinson’s disease. Gait Posture 26:172–178. doi:10.1016/j.gaitpost.2007.04.010
Orendurff MS, Segal AD, Berge JS, Flick KC, Spanier D, Klute GK (2006) The kinematics and kinetics of turning: limb asymmetries associated with walking a circular path. Gait Posture 23:106–111. doi:10.1016/j.gaitpost.2004.12.008
Spildooren J, Vercruysse S, Meyns P Vandenbossche J, Heremans E, Desloovere K, Vandenberghe W, Niewboer A (2012) Turning and unilateral cueing in Parkinson’s disease patients with and without freezing of gait. Neuroscience 207:298–306. doi:10.1016/j.neuroscience.2012.01.024
Sedaghati P, Daneshmandi H, Karimi N, Barati AH (2016) A selective corrective exercise to decrease falling and improve functional balance in idiopathic Parkinson’s disease. Trauma Mon 21:21:e23573. doi:10.5812/traumamon.23573
Yang YR, Lee YY, Cheng SJ, Lin PY, Wang RY (2008) Relationships between gait and dynamic balance in early Parkinson’s disease. Gait Posture 27:611–615. doi:10.1016/j.gaitpost.2007.08.003
Moore ST, MacDougall HG, Gracies JM, Cohen HS, Ondo WG (2007) Long-term monitoring of gait in Parkinson’s disease. Gait Posture 26:200–207. doi:10.1016/j.gaitpost.2006.09.011
Sofuwa O, Nieuwboer A, Desloovere K, Willems AM, Chavret F, Jonkers I (2005) Quantitative gait analysis in Parkinson’s disease: comparison with a healthy control group. Arch Phys Med Rehabil 86:1007–1013. doi:10.1016/j.apmr.2004.08.012
Roiz RDM, Cacho EWA, Pazinatto MM, Pazinatto MM, Reis JG, Cliquet A Jr, Barasnevicius-Quagliato EM (2010) Gait analysis comparing Parkinson’s disease with healthy elderly subjects. Arq Neuropsiquiatr 68:81–86
Huxham F, Baker R, Morris ME, Iansek R (2008) Footstep adjustments used to turn during walking in Parkinson’s disease. Mov Disord 23:817–823. doi:10.1002/mds.21932
Snijders AH, Nijkrake MJ, Bakker M, Munneke M, Wind C, Bloem BR (2008) Clinimetrics of freezing of gait. Mov Disord 23:S468–S474. doi:10.1002/mds.22144
Hoehn MM Yahr MD (1998) Parkinsonism: onset, progression, and mortality. Neurology 50:318
Goetz CG, Poewe W, Rascol O, Sampaio C, Stebbins GT, Counsell C, Giladi N, Holloway RG, Moore CG, Wenning GK, Yahr MD, Seidi L; Movement Disorder Society Task Force on Rating Scales for Parkinson’s Disease (2004) Movement disorder society task force report on the Hoehn and Yahr staging scale: status and recommendations. Mov Dis 19:1020–1028
Papapetropoulos S, Katzen H, Schrag A, Singer C, Scanlon BK, Nation D, Guevara A, Levin B (2008) A questionnaire-based (UM-PDHQ) study of hallucinations in Parkinson’s disease. BMC Neurol 8:21. doi:10.1186/1471-2377-8-21
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56:33–39
Hughes AJ, Daniel SE, Lees AJ (2001) Improved accuracy of clinical diagnosis of Lewy body Parkinson’s disease. Neurology 57:1497–1499
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Nocera JR, Roemmich R, Elrod J, Altmann LJ, Hass CJ (2013) Effects of cognitive task on gait initiation in Parkinson disease: evidence of motor prioritization. J Rehabil Res Dev 50:699–708
Sailer A, Molnar GF, Paradiso G, Gunraj CA, Lang AE, Chen R (2003) Short and long latency afferent inhibition in Parkinson’s disease. Brain 126:1883–1894
Nanhoe-Mahabier W, Snijders AH, Delval A, Weerdesteyn V, Duysens J, Overeem S, Bloem BR (2011) Walking patterns in Parkinson’s disease with and without freezing of gait. Neuroscience 182:217–224. doi:10.1016/j.neuroscience.2011.02.061
Galna B, Murphy AT, Morris ME (2010) Obstacle crossing in people with Parkinson’s disease: foot clearance and spatiotemporal deficits. Hum Mov Sci 29:843–852. doi:10.1016/j.humov.2009.09.006
Yoon J, Park J, Park K, Jo G, Kim H, Jang W, Kim J, Youn J, Oh ES, Kim HT, Youm CH (2016) The effects of additional arm weights on arm-swing magnitude and gait patterns in Parkinson’s disease. Clin Neurophysiol 127:693–697. doi:10.1016/j.clinph.2015.06.005
Stack E, Ashburn A, Jupp K (2005) Postural instability during reaching tasks in Parkinson’s disease. Physiother Res Int 10:146–153
Yogev G, Giladi N, Peretz C, Springer S, Simon ES, Hausdorff JM (2005) Dual tasking, gait rhythmicity, and Parkinson’s disease: which aspects of gait are attention demanding? Eur J Neurosci 22:1248–1256. doi:10.1111/j.1460-9568.2005.04298.x
Campbell CM, Rowse JL, Ciol MA, Shumway-Cook A (2003) The effect of cognitive demand on timed up and go performance in older adults with and without Parkinson disease. J Neurol Phys Ther 27:2–7
Weiss A, Herman T, Plotnik M, Brozgol M, Maidan I, Giladi N, Gurevich T, Hausdorff JM (2010) Can an accelerometer enhance the utility of the Timed Up & Go Test when evaluating patients with Parkinson’s disease? Med Eng Phys 32:119–125. doi:10.1016/j.medengphy.2009.10.015
Yang WC, Hsu WL, Wu RM, Lu TW, Lin KH (2016) Motion analysis of axial rotation and gait stability during turning in people with Parkinson’s disease. Gait Posture 44:83–88. doi:10.1016/j.gaitpost.2015.10.023
Nagano H, Begg RK, Sparrow WA, Taylor S (2011) Ageing and limb dominance effects on foot-ground clearance during treadmill and overground walking. Clin Biomech (Bristol Avon) 26:962–968. doi:10.1016/j.clinbiomech.2011.05.013
Winogrodzka A, Wagenaar RC, Booij J, Wolters EC (2005) Rigidity and bradykinesia reduce interlimb coordination in Parkinsonian gait. Arch Phys Med Rehabil 86:183–189. doi:10.1016/j.apmr.2004.09.010
Huxham F, Baker R, Morris ME, Iansek R (2008) Head and trunk rotation during walking turns in Parkinson’s disease. Mov Disord 23:1391–1397. doi:10.1002/mds.21943
Bhatt H, Pieruccini-Faria F, Almeida QJ (2013) Dynamics of turning sharpness influences freezing of gait in Parkinson’s disease. Parkinsonism Relat Disord 19:181–185. doi:10.1016/j.parkreldis.2012.09.006
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
This study was supported by the Dong-A University research fund.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants in the study.
Rights and permissions
About this article
Cite this article
Son, M., Youm, C., Cheon, S. et al. Evaluation of the turning characteristics according to the severity of Parkinson disease during the timed up and go test. Aging Clin Exp Res 29, 1191–1199 (2017). https://doi.org/10.1007/s40520-016-0719-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-016-0719-y