Abstract
Purpose
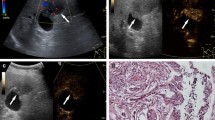
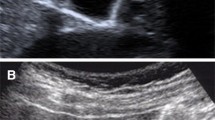
Conventional grayscale ultrasound (US) is accurate in the diagnosis of gallbladder disease (GD), but in some cases, it is not decisive. Contrast-enhanced ultrasound (CEUS) improves the diagnostic accuracy of US. The primary objective of this study is to assess the reliability of CEUS in the diagnosis of sludge; the secondary objective is to assess the ability of CEUS to diagnose cancer.
Methods
We retrospectively reviewed the US of 4137 patients positive for GD. In 43/4137 (1.04%), the use of could not discriminate between sludge and neoplasms. Then, we evaluated CEUS in only 39 of these patients, and in 4/43 (9%) cases it was not performable. After CEUS, the absence of enhancement was considered diagnostic for sludge, while contrast washout within 60 s diagnosed malignant lesions.
Results
Among the 39 patients, 16 had biliary sludge and 23 had lesions of the gallbladder wall; 9 of these were carcinomas and 14 were benign tumors. The absence of enhancement was present in 16/16 patients with sludge and in 0/23 patients with lesions of the gallbladder (sensitivity and specificity 100%). Washout was within 60 s in 9/9 gallbladder carcinomas and 2/14 benign lesions (sensitivity 100%; specificity 85%).
Conclusions
US is confirmed to be accurate in the diagnosis of GD. In doubtful cases, CEUS is very accurate in biliary sludge diagnosis. An intralesional washout at 60 s is a pattern of malignancy that can orient towards a correct diagnosis, but it is limited by the presence of false positive results, especially for smaller lesions.
Sommario
Scopo
L’ecografia convenzionale in scala dei grigi (US) è accurata nella diagnosi delle malattie colecistiche (GD) ma in alcuni casi non è decisiva. L’ecografia con mezzo di contrasto (CEUS), migliora l’affidabilità diagnostica dell’US. Obiettivo primario di questo studio è quello di determinare l’affidabilità della CEUS nella diagnosi di fango biliare; obiettivo secondario definire l’affidabilità della CEUS nella diagnosi di carcinoma della colecisti.
Metodi
Abbiamo analizzato retrospettivamente 4137 ecografie di pazienti positive per GD. In 43/4137 (1.04%) l’ecografia non era capace di discriminare tra fango e neoplasie. La CEUS era valutata in soli 39 pazienti, in 4/43 (9%) dei casi non era eseguibile. L’assenza di enhancement alla CEUS era considerato diagnostico per sludge, mentre un washout del contrasto entro 60 secondi era diagnostico per malattie maligne. L’assenza di enhancement era presente in 16/16 pazienti con fango e in 0/23 pazienti con lesioni colecistiche (sensibilità e specificità 100%). Il wash-out era presente a 60 sec in 9/9 tumori colecistiti e in 2/14 lesioni benigne (sensibilità 100%, specificità 85%).
Conclusioni
L’ecografia si conferma accurata nella diagnosi delle GD. Nei casi dubbi la CEUS è veramente accurata nella diagnosi di sludge. Un wash out intralesionale a 60 secondi è un pattern di malignità che può orientare verso una corretta diagnosi, ma è limitato dalla presenza di risultati falsi positivi, specialmente nelle lesioni più piccole.



Similar content being viewed by others
References
Hederstrom E, Forsberg L (1987) Ultrasonography in carcinoma of gallbladder: diagnostic difficults and pitfalls. Acta Radiol 28:715–718
Franquet T, Montes M, De Azua R, Jimenez FJ, Cozcolluela R (1991) Primary gallbladder carcinoma: imaging findings in 50 patients with pathologic correlation. Gastrointest Radiol 16:143–148
Pandey M, Sood BP, Shukla RC, Aryya NC, Singh S, Shukla VK (2000) Carcinoma of the gallbladder: role of sonography in diagnosis and staging. J Clin Ultrasound 28:227–232
Dalla Palma L, Rizatto G, Pozzi- Mucelli RS, Bazzocchi M (1980) Grey scale ultrasonography in the evaluation of carcinoma of the gallbladder. Br J Radiol 53:662–667
Hirooka Y, Naitoh Y, Goto H, Furukawa T, Ito A, Hayakawa T (1996) Differential diagnosis of gallbladder masses using color Doppler ultrasonography. J Gastroenterol Hepatol 11:840–846
Komatsuda T, Ishida H, Konno K et al (2000) Gallbladder carcinoma: color Doppler sonography. Abdom Imaging 25:194–197
Ueno N, Tomiyana T, Tano S, Wada S, Kimura K (1996) Diagnosis of gallbladder carcinoma with gallbladder carcinoma with color Doppler USG. Am J Gastroenterol 91:1647–1649
Pradhan S, Shukla VK, Agrawal S, Dixit VK, Sharma OP (2002) Sonographic and color Doppler morphology in gallbladder carcinoma. Indian J Cancer 39:143–148
Hattori M, Inui K (2007) Usefulness of contrast-enhanced ultrasonography in the differential diagnosis of polypoid gallbladder lesions. Nippon Shokakibyo Gakkai Zasshi 104(6):790–798
Ko CW, Sekijima JH, Lee SP (1999) Biliary sludge. Ann Intern Med 130(4):301–311
Anastasi B, Sutherland GR (1981) Biliary sludge ultrasonic appearance simulating neoplasm. Br J Radiol 54:679–681
Kuo YC, Liu JY, Sheen IS, Yang CY, Lin DY, Chang Chein CS (1990) Ultrasonographic difficulties and pitfalls in diagnosing primary carcinoma of the gallbladder. J Clin Ultrasound 18(8):639–647
Filly RA, Allen B, Minton MJ, Bernhoft R, Way LW (1980) In vitro investigation of the origin of echoes with biliary sludge. Small polypoid lesions of the gallbladder differential diagnosis and surgical indications by helical computed tomography. J Clin Ultrasound 8:193–200
Furukawa H, Kosuge T, Shimada K, Yamamoto J, Kanai Y, Mukai K, Iwata R, Ushio K (1998) Small polypoid lesions of the gallbladder differential diagnosis and surgical indications by helical computed tomography. Arch Surg 133:735–739
Rodríguez-Fernández A, Gómez-Río M, Medina-Benítez A, Moral JV, Ramos-Font C, Ramia-Angel JM, Llamas-Elvira JM, Ferrón-Orihuela JA, Lardelli-Claret P (2006) Application of modern imaging methods in diagnosis of gallbladder cancer. J Surg Oncol 93:650–664. https://doi.org/10.1002/jso.20533
Mocci G, Migaleddu V, Cabras F, Sirigu D, Scanu D, Virgilio G, Marzo M (2017) SICUS and CEUS imaging in Crohn’s disease: an update. J Ultrasound 20(1):1–9. https://doi.org/10.1007/s40477-016-0230-5
David E, Cantisani V, Grazhdani H, Di Marzo L, Venturini L, Fanelli F, Di Segni M, Di Leo N, Brunese L, Calliada F, Ciccariello M, Bottari A, Ascenti G, D’Ambrosio F (2016) What is the role of contrast-enhanced ultrasound in the evaluation of the endoleak of aortic endoprostheses? A comparison between CEUS and CT on a widespread scale. J Ultrasound 19(4):281–287. https://doi.org/10.1007/s40477-016-0222-5
Ricci P, Cantisani V, Biancari F, Drud FM, Coniglio M, Di Filippo A, Fasoli F, Passariello R (2000) Contrast-enhanced color Doppler US in malignant portal vein thrombosis. Acta Radiol 41(5):470–473
Cantisani V, Ricci P, Erturk M, Pagliara E, Drudi F, Calliada F, Mortele K, D’Ambrosio U, Marigliano C, Catalano C, Marin D, Di Seri M, Longo F, Passariello R (2010) Detection of hepatic metastases from colorectal cancer: prospective evaluation of gray scale US versus SonoVue® low mechanical index real time-enhanced US as compared with multidetector-CT or Gd-BOPTA-MRI. Ultraschall Med 31(5):500–505. https://doi.org/10.1055/s-0028-1109751
Inoue T, Kitano M, Kuto M et al (2007) Diagnosis of gallbladder diseases by contrast-enhanced phase-inversion harmonic ultrasonography. Ultrasound Med Biol 33(3):353–361. https://doi.org/10.1016/j.ultrasmedbio.2006.09.003
Xie XH, Xu HX, Xie XY et al (2010) Differential diagnosis between benign and malignant gallbladder diseases with real-time contrast-enhanced ultrasound. Eur Radiol 20:239–248. https://doi.org/10.1007/s00330-009-1538-8
Badea R, Zaro R, Opincariu I, Chiorean L (2014) Ultrasound in the examination of the gallbladder—a holistic approach: grey scale, Doppler, CEUS, elastography, and 3D. Med Ultrasonogr. https://doi.org/10.11152/mu.201.3.2066.164.rbrz
Claudon M, Cosgrove D, Albrecht T et al (2008) Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS)—update. Ultraschall Med 2008 29:28–44. https://doi.org/10.1055/s-2007-963785
Piscaglia F, Nolsøe C, Cf Dietrich et al (2012) The EFSUMB guidelines and recommendations on the clinical practice of contrast enhanced ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med 33(1):33–59. https://doi.org/10.1055/s-0031-1281676
Liu LN, Xu Hx LuMd, Xy Xie, Wang W, Hu B, Yan K, Ding H, Ss Tang, Lx Qian, Bm Luo, Yl Wen (2012) Contrast-enhanced ultrasound in the diagnosis of gallbladder diseases: a multi-center experience. PLoS One 7:e48371. https://doi.org/10.1371/journal.pone.0048371
Si Q, Qian XL, Wang F et al (2013) Real-time grey scale contrast-enhanced ultrasonography in diagnosis of gallbladder cancer. Ultrasound Med Biol 39:S86
Liu L, Zhao Y, Zhang Y, Liu J (2015) Differential diagnosis between benign and malignant gallbladder diseases with contrast-enhanced ultrasound. Ultrasound Med Biol 41:S99
Wang W, Fei Y, Wang F (2016) Meta-analysis of contrast-enhanced ultrasonography for the detection of gallbladder carcinoma. Med Ultrasonogr 18:281–287. https://doi.org/10.11152/mu.2013.2066.183.wei
Moriguchi H, Tazawa J, Hayashi Y et al (1996) Natural history of polypoid lesions in the gallbladder. Gut 39(6):860–862
Sheth S, Berford A, Chopra S (2000) Primary gallbladder cancer: recognition of risk factors and the role of prophylactic cholecystectomy. Am J Gastrenterol 95:1402–1410
Li D, Dong BW, Wu YL, Yan K (1994) Image-directed and color Doppler studies of gallbladder tumors. J Clin Ultrasound 22:551–555
Adamietz B, Wenkel E, Uder M, Meyer T, Schneider I, Dimmler A, Bautz W, Janka R (2007) Contrast enhanced sonography of the gallbladder: a tool in the diagnosis of cholecystitis? Eur J Radiol 61(2):262–266. https://doi.org/10.1016/j.ejrad.2006.09.006
Numata K, Oka H, Morimoto M et al (2007) Differential diagnosis of gallbladder diseases with contrast-enhanced harmonic gray scale ultrasonography. J Ultrasound Med 26(6):763–774. https://doi.org/10.7863/jum.2007.26.6.763
Zhuang B, Li W, Wang W et al (2017) Contrast-enhanced ultrasonography improves the diagnostic specificity for gallbladder-confined focal tumors. Abdom Radiol (NY). https://doi.org/10.1007/s00261-017-1268-3
Ricci P, Marigliano C, Cantisani V, Porfiri A, Marcantonio A, Lodise P, D’Ambrosio U, Labbadia G, Maggini E, Mancuso E, Panzironi G, Di Segni M, Furlan C, Masciangelo R, Taliani G (2013) Ultrasound evaluation of liver fibrosis: preliminary experience with acoustic structure quantification (ASQ) software. Radiol Med 118(6):995–1010. https://doi.org/10.1007/s11547-013-0940-0
Dietrich CF, Bamber J, Berzigotti A et al (2017) EFSUMB guidelines and recommendations on the clinical use of liver ultrasound elastography, update 2017 (Long Version). Ultraschall Med 38(4):e16–e47. https://doi.org/10.1055/s-0043-103952
Teber MA, Tan S, Dönmez U, İpek A, Uçar AE, Yıldırım H, Aslan A, Arslan H (2014) The use of real-time elastography in the assessment of gallbladder polyps: preliminary observations. Med Ultrasonogr 16(4):304–308. https://doi.org/10.11152/mu.201.3.2066.164.1mat
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Serra Carla, Felicani Cristina, Mazzotta Elena, Gabusi Veronica, Grasso Valentina, De Cinque Antonio, Giannitrapani Lydia and Soresi Maurizio, authors of this manuscript, declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Serra, C., Felicani, C., Mazzotta, E. et al. CEUS in the differential diagnosis between biliary sludge, benign lesions and malignant lesions. J Ultrasound 21, 119–126 (2018). https://doi.org/10.1007/s40477-018-0286-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-018-0286-5