Abstract
Purpose of the study
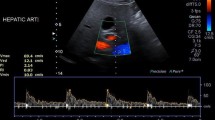
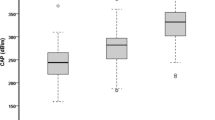
Conventional ultrasound (US) is reliable to reveal the presence of non-alcoholic fatty liver disease (NAFLD), but it is neither sensitive nor specific to reveal fibrosis clues, except in advanced stages where signs of cirrhosis are evident. NALFD fibrosis score is a non-invasive parameter that predicts well the presence of significant fibrosis, but correlations with US parameters are lacking. The aim of this study was, therefore, to compare resistive index of hepatic artery (HARI) of NAFLD patients with different severity degrees of diffuse fatty liver disease vs HARI of controls, and to compare HARI of NAFLD patients with different NAFLD fibrosis scores vs HARI of controls.
Methods
This was a spontaneous, no-profit observational study conducted in our US department between December 2013 and July 2014. Patients with NAFLD with different severity of disease and healthy controls were included. Echogenicity and size of liver and spleen, maximum portal vein velocity, RI, peak systolic velocity (PSV), and end diastolic velocity (EDV) of splenic artery, PSV, EDV, and RI of hepatic artery, and NAFLD fibrosis score were acquired and compared between groups.
Results
HARI was significantly lower in NAFLD patients than controls (p < 0.0001). A significant difference was also found between the groups of NAFLD severity (p < 0.0001). There was also a difference between HARI of NAFLD patients with different NAFLD fibrosis scores vs HARI of controls (p < 0.0001) with a positive correlation between HARI and NAFLD fibrosis score.
Conclusion and discussion
Conventional Doppler US can be helpful to detect NAFLD patients with the risk of fibrous tissue accumulation. HARI tends to exceed the range of controls for patients with NAFLD fibrosis score greater than 0.675. The detection of HARI greater than 0.9 in NAFLD patients, regardless of the US degree of severity of steatosis, might suggest the execution of biopsy to predict the risk of progression to steatohepatitis and fibrous tissue accumulation. Low values of HARI may be expression of lower risk, which does not necessitate any biopsy.
Sommario
Scopo dello studio
L’ecografia convenzionale è risultata affidabile nel rilevare la presenza di steatosi epatica, tra cui la forma non alcolica (NAFLD), ma non è né sensibile né specifica nel rivelare indizi suggestivi di fibrosi, tranne che in fase avanzata dove sono presenti segni conclamati di cirrosi. Il NALFD fibrosis score è un parametro non invasivo che predice bene la presenza di fibrosi significativa, ma non ci sono dati in letteratura riguardanti una possibile correlazione con i parametri ecografici. Lo scopo di questo studio è stato quindi quello di confrontare HARI dei pazienti con NAFLD a differente grado di severità di steatosi epatica vs l’HARI dei controlli, e di confrontare HARI dei pazienti affetti da NAFLD a differente NAFLD fibrosis score vs l’HARI dei controlli.
Metodi
Studio osservazionale spontaneo, no-profit condotto nel nostro Dipartimento tra il dicembre 2013 e il luglio 2014. Venivano inclusi i pazienti con NAFLD a differente severità di malattia e controlli sani. Venivano registrati e confrontati tra gruppi i seguenti parametri: ecogenicità, dimensioni del fegato e della milza, velocità massima della vena porta, indice di resistenza (RI), velocità di picco sistolico (PSV), velocità tele-diastolica finale (EDV) di arteria splenica, e PSV, EDV e RI dell’arteria epatica (HARI) ed il NAFLD fibrosis score.
Risultati
HARI risultava significativamente più basso nei pazienti affetti da NAFLD rispetto ai controlli (p < 0.0001). Una differenza significativa veniva trovata anche tra i gruppi a differente severità di steatosi (p < 0.0001). Veniva riscontrata anche una differenza tra HARI dei pazienti con NAFLD a differente NAFLD fibrosis score vs HARI dei controlli (p < 0.0001) con una correlazione positiva tra HARI e NAFLD fibrosis score.
Conclusione e discussione
L’ecografia Doppler può essere utile per individuare pazienti con NAFLD a rischio di evoluzione fibrotica. HARI tende a superare i valori dei controlli per i pazienti con NAFLD fibrosis score superiore a 0.675. La rilevazione di HARI superiore a 0.9 nei pazienti con NAFLD, indipendentemente dal grado di severità di steatosi, potrebbe indicare l’esecuzione della biopsia al fine di prevedere il rischio di progressione a steatoepatite e fibrosi. Bassi valori di HARI potrebbero essere invece espressione di rischio più basso che non necessiterebbero di alcuna biopsia.



Similar content being viewed by others
References
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ (2012) The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 55:2005–2023
Bhala N, Jouness RI, Bugianesi E (2013) Epidemiology and natural history of patients with NAFLD. Curr Pharm Des 19:5169–5176
Clark JM (2006) The epidemiology of nonalcoholic fatty liver disease in adults. J Clin Gastroenterol 40:S5–S10
Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, Enders F, Saksena S, Burt AD, Bida JP, Lindor K, Sanderson SO, Lenzi M, Adams LA, Kench J, Therneau TM, Day CP (2007) The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology 45:846–854
McPherson S, Stewart SF, Henderson E, Burt AD, Day CP (2010) Simple non-invasive fibrosis scoring systems can reliably exclude advanced fibrosis in patients with non-alcoholic fatty liver disease. Gut 59:1265–1269
Arora A, Sharma P (2012) Non-invasive diagnosis of fibrosis in non-alcoholic fatty liver disease. J Clin Exp Hepatol 2:145–155
Mihmanli I, Kantarci F, Yilmaz MH, Gurses B, Selcuk D, Ogut G, Altug A, Uysal O (2005) Effect of diffuse fatty infiltration of the liver on hepatic artery resistance index. J Clin Ultrasound 33:95–99
Mohammadinia AR, Bakhtavar K, Ebrahimi-Daryani N, Habibollahi P, Keramati MR, Fereshtehnejad SM, Abdollahzade S (2010) Correlation of hepatic vein Doppler waveform and hepatic artery resistance index with the severity of nonalcoholic fatty liver disease. J Clin Ultrasound 38:346–352
Mohammadi A, Ghasemi-rad M, Zahedi H, Toldi G, Alinia T (2011) Effect of severity of steatosis as assessed ultrasonographically on hepatic vascular indices in non-alcoholic fatty liver disease. Med Ultrason 13:200–206
Gaiani S, Avogaro A, Bombonato GC, Bolognesi M, Amor F, Vigili de Kreutzenberg S, Guarneri G, Sacerdoti D (2009) Nonalcoholic fatty liver disease (NAFLD) in nonobese patients with diabetes: prevalence and relationships with hemodynamic alterations detected with Doppler sonography. J Ultrasound 12:1–5
Zekanovic D, Ljubicic N, Boban M, Nikolic M, Delic-Brkljacic D, Gacina P, Klarin I, Turcinov J (2010) Doppler ultrasound of hepatic and system hemodynamics in patients with alcoholic liver cirrhosis. Dig Dis Sci 55:458–466
Stål P (2015) Liver fibrosis in non-alcoholic fatty liver disease—diagnostic challenge with prognostic significance. World J Gastroenterol 21:11077–11087
Tchelepi H, Ralls PW, Radin R, Grant E (2002) Sonography of diffuse liver disease. J Ultrasound Med 21:1023–1032
Kanayama Y, Kamiyama N, Maruyama K, Sumino Y (2013) Real-time ultrasound attenuation imaging of diffuse fatty liver disease. Ultrasound Med Biol 39:692–705
Kirovski G, Schacherer D, Wobser H, Huber H, Niessen C, Beer C, Schölmerich J, Hellerbrand C (2010) Prevalence of ultrasound-diagnosed non-alcoholic fatty liver disease in a hospital cohort and its association with anthropometric, biochemical and sonographic characteristics. Int J Clin Exp Med 15:202–210
Suzuki K, Kirikoshi H, Yoneda M, Mawatari H, Fujita K, Nozaki Y, Takahashi H, Abe Y, Inamori M, Shimamura T, Kobayashi N, Kubota K, Saito S, Nakajima A (2010) Measurement of spleen volume is useful for distinguishing between simple steatosis and early-stage non-alcoholic steatohepatitis. Hepatol Res 40:693–700
Lurie Y, Webb M, Cytter-Kuint R, Shteingart S, Lederkremer GZ (2015) Non-invasive diagnosis of liver fibrosis and cirrhosis. World J Gastroenterol 21:11567–11583
Hirooka M, Koizumi Y, Miyake T et al (2015) Nonalcoholic fatty liver disease: portal hypertension due to outflow block in patients without cirrhosis. Radiology 274(2):597–604
Hizli S, Kocyigit A, Arslan N et al (2010) Hepatic artery resistance in children with obesity and fatty liver. Indian J Pediatr 77(4):407–411
Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D’Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Săftoiu A, Schaefer F, Dietrich CF, EFSUMB (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med 34:238–253
Cui XW, Friedrich-Rust M, De Molo C, Ignee A, Schreiber-Dietrich D, Dietrich CF (2013) Liver elastography, comments on EFSUMB elastography guidelines 2013. World J Gastroenterol 19:6329–6347
Fiorini E, Cipriano V, De Molo C, Righi S, Ainora ME, Arcelli A, Bertusi C, Montanari M, Bianchi G, Serra C (2012) Real-time elastography as a noninvasive technique for quantification of fibrosis in patients with chronic viral liver disease: preliminary findings. J Ultrasound 15:220–225
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Claudio Tana received a Grant from the Italian Society of Ultrasound in Medicine and Biology (SIUMB) for the best oral communication presented at the 25th SIUMB Congress.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. All patients provided written informed consent to enrolment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Human and animal studies
The study was conducted in accordance with all institutional and national guidelines for the care of humans, and did not include laboratory animals.
Additional information
This article won prize for the best oral communication at the 25th National Congress of the Italian Society of Ultrasound in Medicine and Biology (SIUMB).
Rights and permissions
About this article
Cite this article
Tana, C., Tana, M., Rossi, S. et al. Hepatic artery resistive index (HARI) and non-alcoholic fatty liver disease (NAFLD) fibrosis score in NAFLD patients: cut-off suggestive of non-alcoholic steatohepatitis (NASH) evolution. J Ultrasound 19, 183–189 (2016). https://doi.org/10.1007/s40477-016-0203-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-016-0203-8