Abstract
Purpose
To evaluate the prevalence of bright liver echo pattern (BLP) on ultrasonography and its correlation with liver steatosis (LS), and fibrosis in patients with chronic hepatitis C. The usefulness of detecting skip areas for steatosis diagnosis has also been evaluated.
Methods
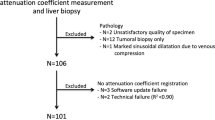
The study included 88 patients with chronic hepatitis C (55 men, 33 women, average age 45.7 ± 11.2 years). Ultrasound examination was performed in all patients before liver biopsy. The presence of BLP was assessed and graded from 1 to 3. Hypoechogenic areas (skip areas) around the gallbladder or near the portal vein were also evaluated. Hepatic fibrosis was assessed using the Ishak fibrosis score. Steatosis was graded as follows: 1, 2, 3 (<30, 30–70, >70 % of hepatocytes affected, respectively).
Results
Fifty-three of the 88 patients (60 %) showed BLP (40 grade 1, 13 grades 2 or 3). Skip areas were found in 14 patients (16 %). Histological steatosis was observed in 40 patients (45 %) and in 10 of them (25 %) was grades 2 and 3 (4 and 6 patients, respectively). As regards fibrosis, 2 patients showed F0, 34 F1, 28 F2, 20 F3, 4 F4, none of them F5 and F6. BLP of grades 2 or 3 and presence of skip areas were strongly correlated with LS (P = 0.00007 and P = 0.00003, respectively). No correlation was found between BLP and fibrosis. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy of BLP for LS were 75, 50, 56, 68 and 61 %, respectively. When BLP of grades 2 and 3 and LS of 30 % or more were correlated, the sensitivity, specificity, PPV, NPV and accuracy of BLP were 72, 96, 61, 96 and 90 %, respectively. As regards skip areas the sensitivity, specificity, PPV, NPV and accuracy for LS were 35, 100, 100, 64 and 70 %, respectively.
Conclusions
In a well-defined group of patients with chronic hepatitis C, the detection of BLP grades 2 and 3 has a good sensitivity and high specificity for high grades of steatosis. A high specificity but low sensitivity for liver steatosis was also found for skip areas, whereas mild fibrosis does not seem to correlate with the hyperechogenicity of the liver.
Riassunto
Scopo
Scopo del lavoro é stato quello di valutare la prevalenza del “bright liver echo pattern” (BLP) all’ultrasonografia e la sua correlazione con la steatosi epatica (SE) e la fibrosi in un gruppo di pazienti con epatite cronica C. E’ stata valutata anche l’utilità della determinazione delle cosiddette “aree di risparmio” per la diagnosi di steatosi.
Metodi
Lo studio ha incluso 88 pazienti con epatite cronica C (55 di sesso maschile, 33 di sesso femminile; età media 45.7 ± 11.2 anni). L’esame ultrasonografico é stato eseguito in tutti i pazienti prima di effettuare la biopsia epatica. La presenza di BLP é stata graduata da 1 a 3. É stata anche valutata la presenza o meno di aree ipoecogene (cosiddette “aree di risparmio”), adiacenti alla colecisti o in sede parailare epatica. La fibrosi epatica é stata stadiata istologicamente utilizzando la classificazione di Ishak. La steatosi epatica é stata graduata da un punto di vista istologico come segue: 1, 2, 3 (a seconda che il grado di interessamento degli epatociti era rispettivamente <30, da 30 a 70, >70 %).
Risultati
Cinquantatre degli 88 pazienti (60 %) hanno mostrato BLP (40 di grado 1, 13 di grado 2 o 3). In 14 pazienti (16 %) sono state rilevate “aree di risparmio”. Istologicamente la steatosi é stata evidenziata in 40 % dei pazienti (45 %) e in 10 di loro (25 %) era di grado 2 e 3 (4 e 6 pazienti rispettivamente). Per quanto riguarda la fibrosi, 2 pazienti hanno presentato F0, 34 F1, 28 F2, 20 F3, 4 F4, nessuno F5 e F6. BLP di grado 2 o 3 e la presenza di “aree di risparmio” era strettamente correlata con SE (P = 0.00007 a P = 0.0003, rispettivamente). Nessuna correlazione é stata trovata tra BLP e fibrosi. La sensibilità, specificità, valore predittivo positivo (VPP), valore predittivo negativo (VPN) e accuratezza della BLP per SE sono stati rispettivamente 75, 50, 56, 68 e 61 %. Quando sono state messe in correlazione BLP di grado 2 e 3 e SE di 30 % o più, sensibilità, specificità, VPP, VPN e accuratezza della BLP sono stati rispettivamente 72, 96, 61, 96 e 90 %. Per quanto riguarda le “aree di risparmio” sensibilità, specificità, VPP, VPN e accuratezza per SE sono stati rispettivamente 35, 100, 100, 64 e 70 %.
Conclusioni
In un ben definito gruppo di pazienti con epatite cronica C, la determinazione di BLP di grado 2 e 3 ha mostrato una buona sensibilità ed un’alta specificità per la steatosi epatica di grado elevato. Un’alta specificità per SE, associata a bassa sensibilità, é stata anche riscontrata per le cosiddette “aree di risparmio”, mentre la fibrosi moderata non sembra correlare con l’ipercogenicità del fegato.
Similar content being viewed by others
References
Joy D, Thava VR, Scott BB (2003) Diagnosis of fatty liver disease: is biopsy necessary? Eur J Gastroenterol Hepatol 15:539–543
Gilmore IT, Burroughs A, Murray-Lyon IM, Williams R, Jenkins D, Hopkins A (1995) Indications, methods, and outcomes of percutaneous liver biopsy in England and Wales: an audit by the British Society of Gastroenterology and the Royal College of Physicians of London. Gut 36:437–441
McGill DB, Rakela J, Zinsmeister AR, Ott BJ (1990) A 21-year experience with major hemorrhage after percutaneous liver biopsy. Gastroenterology 99:1396–1400
Piccinino F, Sagnelli E, Pasquale G, Giusti G (1986) Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol 2:165–173
Wong JB, Bennett WG, Koff RS, Pauker SG (1998) Pretreatment evaluation of chronic hepatitis C: risks, benefits, and costs. JAMA 280:2088–2093
Debongnie JC, Pauls C, Fievez M, Wibin E (1981) Prospective evaluation of the diagnostic accuracy of liver ultrasonography. Gut 22:130–135
Foster KJ, Dewbury KC, Griffith AH, Wright R (1980) The accuracy of ultrasound in the detection of fatty infiltration of the liver. Br J Radiol 53:440–442
Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Guallar E, Clark JM (2011) Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology 54:1082–1090
Joseph AE, Saverymuttu SH, al-Sam S, Cook MG, Maxwell JD (1991) Comparison of liver histology with ultrasonography in assessing diffuse parenchymal liver disease. Clin Radiol 43:26–31
Mathiesen UL, Franzén LE, Aselius H, Resjö M, Jacobsson L, Foberg U, Frydén A, Bodemar G (2002) Increased liver echogenicity at ultrasound examination reflects degree of steatosis but not of fibrosis in asymptomatic patients with mild/moderate abnormalities of liver transaminases. Dig Liver Dis 34:516–522
Palmentieri B, de Sio I, La Mura V, Masarone M, Vecchione R, Bruno S, Torella R, Persico M (2006) The role of bright liver echo pattern on ultrasound B-mode examination in the diagnosis of liver steatosis. Dig Liver Dis 38:485–489
Saadeh S, Younossi ZM, Remer EM, Gramlich T, Ong JP, Hurley M, Mullen KD, Cooper JN, Sheridan MJ (2002) The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology 123:745–750
Saverymuttu SH, Joseph AE, Maxwell JD (1986) Ultrasound scanning in the detection of hepatic fibrosis and steatosis. Br Med J (Clin Res Ed) 292:13–15
Celle G, Savarino V, Picciotto A, Magnolia MR, Scalabrini P, Dodero M (1988) Is hepatic ultrasonography a valid alternative tool to liver biopsy? Report on 507 cases studied with both techniques. Dig Dis Sci 33:467–471
Chen CH, Lin ST, Yang CC, Yeh YE, Kuo CL, Nien CK (2008) The accuracy of sonography in predicting steatosis and fibrosis in chronic hepatitis C. Dig Dis Sci 53:1699–1706
Fontana RJ, Lok AS (2002) Noninvasive monitoring of patients with chronic hepatitis C. Hepatology 36:S57–S64
Hepburn MJ, Vos JA, Fillman EP, Lawitz EJ (2005) The accuracy of the report of hepatic steatosis on ultrasonography inpatients infected with hepatitis C in a clinical setting: a retrospective observational study. BMC Gastroenterol 5:14
Kutcher R, Smith GS, Sen F, Gelman SF, Mitsudo S, Thung SN, Reinus JF (1998) Comparison of sonograms and liver histologic findings in patients with chronic hepatitis C virus infection. J Ultrasound Med 17:321–325
Needleman L, Kurtz AB, Rifkin MD, Cooper HS, Pasto ME, Goldberg BB (1986) Sonography of diffuse benign liver disease: accuracy of pattern recognition and grading. AJR Am J Roentgenol 146:1011–1015
Pamilo M, Sotaniemi EA, Suramo I, Lähde S, Arranto AJ (1983) Evaluation of liver steatotic and fibrous content by computerized tomography and ultrasound. Scand J Gastroenterol 18:743–747
Caturelli E, Squillante MM, Andriulli A, Cedrone A, Cellerino C, Pompili M, Rapaccini GL, Livraghi T (1992) Hypoechoic lesions in the ‘bright liver’: a reliable indicator of fatty change. A prospective study. J Gastroenterol Hepatol 7:469–472
Ishak K, Baptista A, Bianchi L, Callea F, De Groote J, Gudat F, Denk H, Desmet V, Korb G, MacSween RNM, Phillips MJ, Portmann BG, Poulsen H, Scheuer PJ, Schmid M, Thaler H (1995) Histological grading and staging of chronic hepatitis. J Hepatol 22:696–699
Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, Lok AS (2003) A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology 38:518–526
Hourigan LF, Macdonald GA, Purdie D, Whitehall VH, Shorthouse C, Clouston A, Powell EE (1999) Fibrosis in chronic hepatitis C correlates significantly with body mass index and steatosis. Hepatology 29:1215–1219
Sanyal AJ, American Gastroenterological Association (2002) AGA technical review on nonalcoholic fatty liver disease. Gastroenterology 123:1705–1725
Joseph AE, Dewbury KC, McGuire PG (1979) Ultrasound in the detection of chronic liver disease (the “bright liver”). Br J Radiol 52:184–188
Bach N, Thung SN, Schaffner F (1992) The histological features of chronic hepatitis C and autoimmune chronic hepatitis: a comparative analysis. Hepatology 15:572–577
Lefkowitch JH, Schiff ER, Davis GL, Perrillo RP, Lindsay K, Bodenheimer HC Jr, Balart LA, Ortego TJ, Payne J, Dienstag JL et al (1993) Pathological diagnosis of chronic hepatitis C: a multicenter comparative study with chronic hepatitis B. The Hepatitis Interventional Therapy Group. Gastroenterology 104:595–603
Scheuer PJ, Ashrafzadeh P, Sherlock S, Brown D, Dusheiko GM (1992) The pathology of hepatitis C. Hepatology 15:567–571
Adinolfi LE, Gambardella M, Andreana A, Tripodi MF, Utili R, Ruggiero G (2001) Steatosis accelerates the progression of liver damage of chronic hepatitis C patients and correlates with specific HCV genotype and visceral obesity. Hepatology 33:1354–1364
Castéra L, Hézode C, Roudot-Thoraval F, Bastie A, Zafrani ES, Pawlotsky JM, Dhumeaux D (2003) Worsening of steatosis is an independent factor of fibrosis progression in untreated patients with chronic hepatitis C and paired liver biopsies. Gut 52:288–292
Fartoux L, Chazouillères O, Wendum D, Poupon R, Serfaty L (2005) Impact of steatosis on progression of fibrosis in patients with mild hepatitis C. Hepatology 41:82–87
Serfaty L, Poujol-Robert A, Carbonell N, Chazouillères O, Poupon RE, Poupon R (2002) Effect of the interaction between steatosis and alcohol intake on liver fibrosis progression in chronic hepatitis C. Am J Gastroenterol 97:1807–1812
Westin J, Nordlinder H, Lagging M, Norkrans G, Wejstål R (2002) Steatosis accelerates fibrosis development over time in hepatitis C virus genotype 3 infected patients. J Hepatol 37:837–842
Ramalho F (2003) Hepatitis C virus infection and liver steatosis. Antivir Res 60:125–127
Rubbia-Brandt L, Quadri R, Abid K, Giostra E, Malé PJ, Mentha G, Spahr L, Zarski JP, Borisch B, Hadengue A, Negro F (2000) Hepatocyte steatosis is a cytopathic effect of hepatitis C virus genotype 3. J Hepatol 33:106–115
Hézode C, Roudot-Thoraval F, Zafrani ES, Dhumeaux D, Pawlotsky JM (2004) Different mechanisms of steatosis in hepatitis C virus genotypes 1 and 3 infections. J Viral Hepat 11:455–458
Hirche TO, Ignee A, Hirche H, Schneider A, Dietrich CF (2007) Evaluation of hepatic steatosis by ultrasound in patient with chronic hepatitis C virus infection. Liver Int 27:748–757
Conflict of interest
Maurizio Loy, Giancarlo Serra, Luchino Chessa declare that they have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). All patients provided written informed consent to enrolment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Human and animal studies
The study was conducted in accordance with all institutional and national guidelines for the care and use of laboratory animals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Loy, M., Serra, G. & Chessa, L. The prevalence of bright liver echo pattern in patients with chronic hepatitis C: correlation with steatosis and fibrosis. J Ultrasound 19, 91–98 (2016). https://doi.org/10.1007/s40477-014-0114-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-014-0114-5