Abstract
Background
As policy responses to cannabis use and availability change internationally, the prevalence of cannabis use disorder (CUD) and the number of individuals seeking treatment for cannabis-related problems may increase.
Purpose of the Review
Our aim was to provide a narrative review of developments in the treatment of CUD over the past 5 years, including findings of a recent meta-analysis on psychosocial interventions and adjunctive pharmacotherapies for the management of cannabis withdrawal and CUD. Identification of key knowledge gaps and recommendations for further studies will also be addressed.
Recent Findings
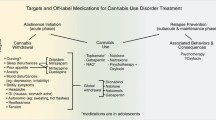
Multiple behavioral interventions, particularly those involving motivational enhancement and cognitive behavioral therapies and their combination, appear helpful for CUD. As yet, there is no evidence-based pharmacotherapy in treating cannabis withdrawal and CUD. Preliminary results for some drugs, particularly agonists, are promising but require further extensive investigation.
Summary
Despite the prevalence and impact of CUD, the evidence base for treatments is not strong, and standardization of measures and endpoints in future randomized controlled trials of psychosocial and pharmacological agents is needed.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
McKiernan A, Fleming K. Canadian Youth Perceptions on Cannabis. Ottawa: Canadian Centre on Substance Abuse; 2017.
Thompson L, Rivara FP, Whitehill JM. Prevalence of marijuana-related traffic on Twitter, 2012-2013: a content analysis. Cyberpsychol Behav Soc Netw. 2015;18(6):311–9.
Swift W, Hall W, Teesson M. Cannabis use and dependence among Australian adults: results from the National Survey of Mental Health and Wellbeing. Addiction. 2001;96(5):737–48.
United Nations Office on Drugs and Crime. World Drug Report 2015 (United Nations publication, Sales No. E.15.XI.6. Vienna; 2015.
Teesson M, Slade T, Swift W, Mills K, Memedovic S, Mewton L, et al. Prevalence, correlates and comorbidity of DSM-IV cannabis use and cannabis use disorders in Australia. Aust N Z J Psychiatry. 2012;46(12):1182–92.
Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, et al. Prevalence of marijuana use disorders in the United States between 2001-2002 and 2012-2013. JAMA Psychiatry. 2015;72(12):1235–42.
Center for Behavioral Health Statistics and Quality. Key substance use and mental health indicators in the United States: results from the 2015 national survey on drug use and health. No. SMA 16-4984, NSDUH Series H-51. 2016. Available at: http://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.htm.
European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2015. Trends and Developments. Portugal: European Monitoring of Drugs and Drugs Addiction; 2015.
Australian Institute of Health and Welfare. Alcohol and other drug treatment services in Australia 2013–14. Canberra, ACT: Australian Institute of Health and Welfare; 2013.
Degenhardt L, Ferrari AJ, Calabria B, Hall WD, Norman RE, McGrath J, et al. The global epidemiology and contribution of cannabis use and dependence to the global burden of disease: results from the GBD 2010 study. PLoS One. 2013;8(10), e76635.
Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, et al. Prevalence and correlates of DSM-5 cannabis use disorder, 2012-2013: findings from the National Epidemiologic Survey on Alcohol and Related Conditions-III. Am J Psychiatry. 2016;173(6):588–99.
Fogerty S. Cannabis addiction support centre to close doors after government cuts funding. ABC News Online. 1996 Nov. Available at: http://www.abc.net.au/news/2016-11-04/cannabis-support-centre-to-close-after-funding-cut/7994558.
Silins E, Horwood LJ, Patton GC, Fergusson DM, Olsson CA, Hutchinson DM, et al. Young adult sequelae of adolescent cannabis use: an integrative analysis. Lancet Psychiatry. 2014;1(4):286–93.
Wall MM, Mauro C, Hasin DS, Keyes KM, Cerda M, Martins SS, et al. Prevalence of marijuana use does not differentially increase among youth after states pass medical marijuana laws: commentary on and reanalysis of US National Survey on Drug Use in Households data 2002-2011. Int J Drug Policy. 2016;29:9–13.
Australian Institute of Health and Welfare. National Drug Strategy Household Survey detailed report 2013. Series 28. Canberra, ACT: Australian Institute of Health and Welfare; 2014.
Burkinshaw P, Knight J, Anders P, Eastwood B, V, Musto, Martin White JM. An evidence review of the outcomes that can be expected of drug misuse treatment in England. London: Public Health England; 2017.
Fairman BJ. Trends in registered medical marijuana participation across 13 US states and District of Columbia. Drug Alcohol Depend. 2016;159:72–9.
Copeland J, Swift W. Cannabis use disorder: epidemiology and management. Int Rev Psychiatry. 2009;21(2):96–103.
Stephens R. S, Roffman, Roger, Simpson E. Adult marijuana users seeking treatment. J Consult Clin Psychol. 1993;61(6):1100–004.
Stinson FS, Ruan WJ, Pickering R, Grant BF. Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychol Med. 2006;36(10):1447–60.
Copeland J, Swift W, Rees V. Clinical profile of participants in a brief intervention program for cannabis use disorder. J Subst Abuse Treat. 2001;20(1):45–52.
McKetin R, Dunlop AJ, Holland RM, Sutherland RA, Baker AL, Salmon AM, et al. Treatment outcomes for methamphetamine users receiving outpatient counselling from the Stimulant Treatment Program in Australia. Drug Alcohol Rev. 2013;32(1):80–7.
• Gates PJ, Sabioni P, Copeland J, Le Foll B, Gowing L. Psychosocial interventions for cannabis use disorder. Cochrane Database Syst Rev. 2016;(5):CD005336. This is the latest meta-analysis for the Cochrane Collaboration on this topic.
Copeland J, Pokorski I. Progress toward pharmacotherapies for cannabis-use disorder: an evidence-based review. Subst Abuse Rehabil. 2016;7:41–53.
Walther L, Gantner A, Heinz A, Majić T. Evidence-based treatment options in cannabis dependency. Dtsch Arztebl Int. 2016;113(39):653–9.
Miller W, Rollnick S. Motivational interviewing: helping people change. J Healthc Qual. 2003;25(3):46.
Agerwala SM, McCance-Katz EF. Integrating screening, brief intervention, and referral to treatment (SBIRT) into clinical practice settings: a brief review. J Psychoactive Drugs;44(4):307–17.
Miller WR, Sanchez VC. Motivating young adults for treatment and lifestyle change. In: Howard G, editor. Issues in alcohol use and misuse in young adults. Notre Dame: University of Notre Dame Press; 1993.
Bray JW, Del Boca FK, McRee BG, Hayashi SW, Babor TF. Screening, Brief Intervention and Referral to Treatment (SBIRT): rationale, program overview and cross-site evaluation. Addiction. 2017;112 Suppl 2:3–11.
Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J. Screening, Brief Intervention, and Referral to Treatment (SBIRT): toward a public health approach to the management of substance abuse. Subst Abus. 2007;28(3):7–30.
Miller WR, Zweben A, Di Clemente CC, Rychtarik RG. Motivational Enhancement Therapy Manual. Project MATCH Monograph Series Editor: Mattson ME. National Institute on Alcohol Abuse and Alcoholism, US Department of Health and Human Services; 2014.
Walker DD, Stephens RS, Blevins CE, Banes KE, Matthews L, Roffman RA. Augmenting brief interventions for adolescent marijuana users: the impact of motivational check-ins. J Consult Clin Psychol. 2016;84(11):983–92.
Webb L, Bertoni M, Copeland J. 20 minutes or less: evidence of the need for a very brief intervention (VBI) for cannabis users. 2015. Available at: file:///C:/Users/z8903265/Desktop/bulletin-23_vbi.pdf.
Beck AT, Wright F, Newman C, Liese B. Cognitive therapy of substance abuse. New York: The Guilford Press; 1993.
Marlatt A, Gordon J. Relapse prevention: maintenance strategies in the treatment of addictive behaviours. New York: The Guilford Press; 1985.
Copeland J. Marijuana brief intervention: an SBIRT approach. Center City, MN: Hazelden Publishing; 2017.
Copeland J, Swift W, Roffman R, Stephens R. A randomized controlled trial of brief cognitive-behavioral interventions for cannabis use disorder. J Subst Abuse Treat. 2001;21(2):55–64. 6.
Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68(5):898–908.
Hoch E, Noack R, Henker J, Pixa A, Höfler M, Behrendt S, et al. Efficacy of a targeted cognitive-behavioral treatment program for cannabis use disorders (CANDIS). Eur Neuropsychopharmacol. 2012;22(4):267–80.
Hoch E, Bühringer G, Pixa A, Dittmer K, Henker J, Seifert A, et al. CANDIS treatment program for cannabis use disorders: findings from a randomized multi-site translational trial. Drug Alcohol Depend. 2014;134:185–93.
Stephens RS, Roffman RA, Copeland J, Swift W. Cognitive-behavioral and motivational enhancement treatments for cannabis dependence. In: Cannabis dependence: its nature, consequences, and treatment. Cambridge: Cambridge University Press; 2006. p. 131–53.
Copeland J, Gates P, Pokorski I. A narrative review of psychological cannabis use treatments with and without pharmaceutical adjunct. Curr Pharm Des. 2016;22(42):6397–408.
Danovitch I, Gorelick DA. State of the art treatments for cannabis dependence. Psychiatr Clin North Am. 2012;35(2):309–26.
Liddle HA, Dakof GA, Turner RM, Henderson CE, Greenbaum PE. Treating adolescent drug abuse: a randomized trial comparing multidimensional family therapy and cognitive behavior therapy. Addiction. 2008;103(10):1660–70.
Dale V, Heather N, Adamson S, Coulton S, Copello A, Godfrey C, et al. Predicting drinking outcomes: evidence from the United Kingdom Alcohol Treatment Trial (UKATT). Addict Behav. 2017;71:61–7.
Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Coping skills training and contingency management treatments for marijuana dependence: exploring mechanisms of behavior change. Addiction. 2008;103(4):638–48.
Budney AJ, Stanger C, Tilford JM, Scherer EB, Brown PC, Li Z, et al. Computer-assisted behavioral therapy and contingency management for cannabis use disorder. Psychol Addict Behav. 2015;29(3):501–11.
Fletcher L, Hayes SC. Relational frame theory, acceptance and commitment therapy, and a functional analytic definition of mindfulness. J Ration Emotive Cogn Behav Ther. 2005;23(4):315–36.
Copeland J, Martin G. Web-based interventions for substance use disorders: a qualitative review. J Subst Abuse Treat. 2004;26(2):109–16.
Rooke SE, Gates PJ, Norberg MM, Copeland J. Applying technology to the treatment of cannabis use disorder: comparing telephone versus Internet delivery using data from two completed trials. J Subst Abuse Treat. 2014;46(1):78–84.
Center for Substance Abuse Treatment. Using technology-based therapeutic tools in behavioral health services. Rockville. MD; Center for Substance Abuse Treatment; 2015.
Myung S-K, McDonnell DD, Kazinets G, Seo HG, Moskowitz JM. Effects of web- and computer-based smoking cessation programs: meta-analysis of randomized controlled trials. Arch Intern Med. 2009;169(10):929–37.
Rooke S, Thorsteinsson E, Karpin A, Copeland J, Allsop D. Computer-delivered interventions for alcohol and tobacco use: a meta-analysis. Addiction. 2010;105(8):1381–90.
Wood SK, Eckley L, Hughes K, Hardcastle KA, Bellis MA, Schrooten J, et al. Computer-based programmes for the prevention and management of illicit recreational drug use: a systematic review. Addict Behav. 2014;39(1):30–8.
Newman MG, Szkodny LE, Llera SJ, Przeworski A. A review of technology-assisted self-help and minimal contact therapies for drug and alcohol abuse and smoking addiction: is human contact necessary for therapeutic efficacy? Clin Psychol Rev. 2011;31(1):178–86.
Tait RJ, Spijkerman R, Riper H. Internet and computer based interventions for cannabis use: a meta-analysis. Drug Alcohol Depend. 2013;133(2):295–304.
Gates P, Albertella L. The effectiveness of telephone counselling in the treatment of illicit drug and alcohol use concerns. J Telemed Telecare. 2016;22(2):67–85.
Gates PJ, Norberg MM, Copeland J, Digiusto E. Randomized controlled trial of a novel cannabis use intervention delivered by telephone. Addiction. 2012;107(12):2149–58.
Balter RE, Cooper ZD, Haney M. Novel pharmacologic approaches to treating cannabis use disorder. Curr Addict Rep. 2014;1(2):137–43.
Allsop DJ, Copeland J, Norberg MM, Fu S, Molnar A, Lewis J, et al. Quantifying the clinical significance of cannabis withdrawal. PLoS One. 2012;7(9):e44864.
Haney M, Bedi G, Cooper ZD, Glass A, Vosburg SK, Comer SD, et al. Predictors of marijuana relapse in the human laboratory: robust impact of tobacco cigarette smoking status. Biol Psychiatry. 2013;73(3):242–8.
Marshall K, Gowing L, Ali R, Le Foll B. Pharmacotherapies for cannabis dependence. Cochrane Database Syst Rev. 2014;12:CD008940.
Levin FR, Mariani J, Brooks DJ, Pavlicova M, Nunes EV, Agosti V, et al. A randomized double-blind, placebo-controlled trial of venlafaxine-extended release for co-occurring cannabis dependence and depressive disorders. Addiction. 2013;108(6):1084–94.
Allsop DJ, Copeland J, Lintzeris N, Dunlop AJ, Montebello M, Sadler C, et al. Nabiximols as an agonist replacement therapy during cannabis withdrawal: a randomized clinical trial. JAMA Psychiatry. 2014;71(3):281–91.
Trigo JM, Lagzdins D, Rehm J, Selby P, Gamaleddin I, Fischer B, et al. Effects of fixed or self-titrated dosages of Sativex on cannabis withdrawal and cravings. Drug Alcohol Depend. 2016;161:298–306.
Crippa JAS, Hallak JEC, Machado-De-Sousa JP, Queiroz RHC, Bergamaschi M, Chagas MHN, et al. Cannabidiol for the treatment of cannabis withdrawal syndrome: a case report. J Clin Pharm Ther. 2013;38(2):162–4.
Pierre JM, Gandal M, Son M. Cannabis-induced psychosis associated with high potency “wax dabs”. Schizophr Res. 2016;172(1–3):211–2.
Ninnemann AL, Lechner WV, Borges A, Lejuez CW. Synthetic cannabinoids to avoid urine drug screens: implications for contingency management and other treatments for drug dependence. Addict Behav. 2016;63:72–3.
Karila L, Benyamina A, Blecha L, Cottencin O, Billieux J. The synthetic cannabinoids phenomenon. Curr Pharm Des. 2016;22(42):6420–5.
Cooper ZD. Adverse effects of synthetic cannabinoids: management of acute toxicity and withdrawal. Curr Psychiatry Rep. 2016;18(5):52.
Schauer GL, Rosenberry ZR, Peters EN. Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: a systematic literature review. Addict Behav. 2016;64:200–11.
Acknowledgments
The National Cannabis Prevention and Information Centre was funded by the Australian Government Department of Health 2007–2016.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
Izabella Pokorski and Lisa Gibson declare that they have no conflicts of interest. Jan Copeland declares grants from the National Cannabis Prevention and Information Centre. She received in-kind contribution of Sativex from GW Pharmaceuticals for a National Health and Medical Research Council-funded clinical trial.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cannabis
Rights and permissions
About this article
Cite this article
Copeland, J., Pokorski, I. & Gibson, L. Overview of Current State-of-the-Art Treatments for Cannabis Use Disorders, and Future Directions. Curr Addict Rep 4, 82–89 (2017). https://doi.org/10.1007/s40429-017-0151-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-017-0151-1