Abstract
Purpose
Cannabis is the most widely used illicit drug with high prevalence, especially in adolescent and psychiatric populations. Cannabis use disorder is associated with cognitive and psychosocial impairment, and the therapeutic potential of cannabis is unsupported by high-quality evidence. Importantly, cannabis use may lead to the development of psychiatric and substance use disorders and to poorer outcomes in the mentally ill. This article discusses the epidemiology and neurobiology of cannabis use and the assessment and treatment of cannabis use disorder, in mental health and addiction settings.
Findings
Evidence suggests that cannabis use has negative effects in patients with major psychiatric disorders. It is critical to better understand the endocannabinoid system and its links with mental illness.
Conclusions
Future studies should determine the potential impact of cannabis legalization on people at risk for, or with pre-existing psychiatric disorders and addictions, as well as the development of novel and more effective treatments for co-occurring cannabis use.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313:2474–83.
Henderson J. Introduction: the effects of cannabis use during adolescence. Ottawa, ON: Canadian Council on Substance Abuse (CCSA); 2015.
Research UOo. Child well-being in rich countries: a comparative overview. Florence, Italy: 2013.
Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991-1992 and 2001-2002. JAMA. 2004;291(17):2114–21.
••Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, et al. Prevalence of marijuana use disorders in the United States between 2001 and 2002 and 2012-2013. JAMA Psychiatry. 2015;72(12):1235–42 This is an important study documenting the increase in prevalence rates of marijuana use and marijuana use disorder in the US adult population between 2001-2002 and 2012-2013. The results suggest potential harm with habitual marijuana use, including risk of addiction.
Cerda M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug Alcohol Depend. 2012;120(1–3):22–7.
Thurstone C, Lieberman SA, Schmiege SJ. Medical marijuana diversion and associated problems in adolescent substance treatment. Drug Alcohol Depend. 2011;118(2–3):489–92.
(RMHIDTA) RMHIDTA. The legalization of marijuana in Colorado: the impact. Denver, CO USA: 2016 Contract No.: Preview 2015.
Hall W, Weier M. Assessing the public health impacts of legalizing recreational cannabis use in the USA. Clin Pharmacol Ther. 2015;97(6):607–15.
•Whiting PF, Wolff RF, Deshpande S, Di Nisio M, Duffy S, Hernandez AV, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456–73 In this systematic review, the authors documented the effects of cannabis and cannabinoid drugs in treating diseases and alleviating slymptoms. Further, it reviews our current understanding of the benefits and adverse events of using medical cannabinoids.
Lev-Ran S, Le Foll B, McKenzie K, George TP, Rehm J. Cannabis use and cannabis use disorders among individuals with mental illness. Compr Psychiatry. 2013;54(6):589–98.
Toftdahl NG, Nordentoft M, Hjorthoj C. Prevalence of substance use disorders in psychiatric patients: a nationwide Danish population-based study. Soc Psychiatry Psychiatr Epidemiol. 2016;51(1):129–40.
Lagerberg TV, Icick R, Andreassen OA, Ringen PA, Etain B, Aas M, et al. Cannabis use disorder is associated with greater illness severity in tobacco smoking patients with bipolar disorder. J Affect Disord. 2016;190:286–93.
Baudin G, Godin O, Lajnef M, Aouizerate B, Berna F, Brunel L, et al. Differential effects of childhood trauma and cannabis use disorders in patients suffering from schizophrenia. Schizophrenia Res. 2016.
Helle S, Ringen PA, Melle I, Larsen TK, Gjestad R, Johnsen E, et al. Cannabis use is associated with 3 years earlier onset of schizophrenia spectrum disorder in a naturalistic, multi-site sample (N = 1119). Schizophr Res. 2016;170(1):217–21.
••Di Forti M, Morgan C, Dazzan P, Pariante C, Mondelli V, Marques TR, et al. High-potency cannabis and the risk of psychosis. Br J Psychiatry. 2009;195(6):488–91 An important study supporting the hypothesis that Δ9-THC increases the risk of developing psychosis, emphasizing the concern about high concentration (potency) of Δ9-THC in marijuana preparations.
Seddon JL, Birchwood M, Copello A, Everard L, Jones PB, Fowler D, et al. Cannabis use is associated with increased psychotic symptoms and poorer psychosocial functioning in first-episode psychosis: a report from the UK national EDEN study. Schizophr Bull. 2016;42(3):619–25.
Patel R, Wilson R, Jackson R, Ball M, Shetty H, Broadbent M, et al. Association of cannabis use with hospital admission and antipsychotic treatment failure in first episode psychosis: an observational study. BMJ Open. 2016;6(3):e009888.
Lozano OM, Rojas AJ, Calderon FF. Dependence on substance users: how it impacts on their health-related quality of life? Journal of mental health (Abingdon, England). 2016:1–8.
Blanco C, Hasin DS, Wall MM, Florez-Salamanca L, Hoertel N, Wang S, et al. Cannabis use and risk of psychiatric disorders: prospective evidence from a US National Longitudinal Study. JAMA psychiatry. 2016;73(4):388–95.
Lorenzetti V, Solowij N, Yucel M. The role of cannabinoids in neuroanatomic alterations in cannabis users. Biol Psychiatry. 2016;79(7):e17–31.
Lorenzetti V, Alonso-Lana S, Youssef GJ, Verdejo-Garcia A, Suo C, Cousijn J, et al. Adolescent cannabis use: what is the evidence for functional brain alteration? Current pharmaceutical design. 2016.
Batalla A, Bhattacharyya S, Yucel M, Fusar-Poli P, Crippa JA, Nogue S, et al. Structural and functional imaging studies in chronic cannabis users: a systematic review of adolescent and adult findings. PLoS One. 2013;8(2):e55821.
•Meier MH, Hill ML, Small PJ, Luthar SS. Associations of adolescent cannabis use with academic performance and mental health: a longitudinal study of upper middle class youth. Drug Alcohol Depend. 2015;156:207–12 In this important longitudinal study of high socioeconomic status (SES) communities, the authors documented the link between cannabis use and poorer academic performace and mental health. Further, it discounts the the hypothesis that low SES may cause the link between cannabis use and poorer acedemic performance and mental health.
Toftdahl NG, Nordentoft M, Hjorthoj C. The effect of changes in cannabis exposure on psychotic symptoms in patients with comorbid cannabis use disorder. Journal of dual diagnosis. 2016;12(2):129–36.
•Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379(9810):55–70 The authors summarized data on the prevalence, links, and adverse health consequences of illicit drugs, highlighting the major adverse health effects of cannabis in causing dependence and psychiatric disorders.
Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the epidemiologic catchment area (ECA) study. JAMA. 1990;264(19):2511–8.
Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. The American journal of orthopsychiatry. 1996;66(1):17–31.
•Hartz SM, Pato CN, Medeiros H, Cavazos-Rehg P, Sobell JL, Knowles JA, et al. Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiatry. 2014;71(3):248–54 This is an important epidemiological study documenting the comorbidity of substance use disorders and severe psychotic illness. Additionaly, it suggests failure of public health efforts in reducing substance use in these vulnerable populations.
Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61(8):807–16.
Nesvag R, Knudsen GP, Bakken IJ, Hoye A, Ystrom E, Suren P, et al. Substance use disorders in schizophrenia, bipolar disorder, and depressive illness: a registry-based study. Soc Psychiatry Psychiatr Epidemiol. 2015;50(8):1267–76.
Wilson RI, Nicoll RA. Endocannabinoid signaling in the brain. Science. 2002;296(5568):678–82.
Marsicano G, Wotjak CT, Azad SC, Bisogno T, Rammes G, Cascio MG, et al. The endogenous cannabinoid system controls extinction of aversive memories. Nature. 2002;418(6897):530–4.
Haller J, Bakos N, Szirmay M, Ledent C, Freund TF. The effects of genetic and pharmacological blockade of the CB1 cannabinoid receptor on anxiety. Eur J Neurosci. 2002;16(7):1395–8.
Solinas M, Yasar S, Goldberg SR. Endocannabinoid system involvement in brain reward processes related to drug abuse. Pharmacol Res. 2007;56(5):393–405.
Miller LL, Branconnier RJ. Cannabis: effects on memory and the cholinergic limbic system. Psychol Bull. 1983;93(3):441–56.
Block RI, Ghoneim MM. Effects of chronic marijuana use on human cognition. Psychopharmacology. 1993;110(1–2):219–28.
Darley CF, Tinklenberg JR, Roth WT, Atkinson RC. The nature of storage deficits and state-dependent retrieval under marihuana. Psychopharmacologia. 1974;37(4):139–49.
Howlett AC, Barth F, Bonner TI, Cabral G, Casellas P, Devane WA, et al. International Union of Pharmacology. XXVII. Classification of cannabinoid receptors. Pharmacol Rev. 2002;54(2):161–202.
Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, Griffin G, et al. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science (New York, NY). 1992;258(5090):1946–9.
Mechoulam R, Ben-Shabat S, Hanus L, Ligumsky M, Kaminski NE, Schatz AR, et al. Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem Pharmacol. 1995;50(1):83–90.
Gaoni YMR. Isolation, structure, and partial synthesis of an active constituent of hashish. J Am Chem Soc. 1964;86:2.
Herkenham M, Lynn AB, Johnson MR, Melvin LS, de Costa BR, Rice KC. Characterization and localization of cannabinoid receptors in rat brain: a quantitative in vitro autoradiographic study. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1991;11(2):563–83.
Munro S, Thomas KL, Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993;365(6441):61–5.
Walter L, Franklin A, Witting A, Wade C, Xie Y, Kunos G, et al. Nonpsychotropic cannabinoid receptors regulate microglial cell migration. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2003;23(4):1398–405.
Ramirez SH, Hasko J, Skuba A, Fan S, Dykstra H, McCormick R, et al. Activation of cannabinoid receptor 2 attenuates leukocyte-endothelial cell interactions and blood-brain barrier dysfunction under inflammatory conditions. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2012;32(12):4004–16.
Glass M, Dragunow M, Faull RL. Cannabinoid receptors in the human brain: a detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience. 1997;77(2):299–318.
Fernandez-Ruiz JJ, Berrendero F, Hernandez ML, Romero J, Ramos JA. Role of endocannabinoids in brain development. Life Sci. 1999;65(6–7):725–36.
Berrendero F, Garcia-Gil L, Hernandez ML, Romero J, Cebeira M, de Miguel R, et al. Localization of mRNA expression and activation of signal transduction mechanisms for cannabinoid receptor in rat brain during fetal development. Development (Cambridge, England). 1998;125(16):3179–88.
Galve-Roperh I, Aguado T, Palazuelos J, Guzman M. Mechanisms of control of neuron survival by the endocannabinoid system. Curr Pharm Des. 2008;14(23):2279–88.
Gao Y, Vasilyev DV, Goncalves MB, Howell FV, Hobbs C, Reisenberg M, et al. Loss of retrograde endocannabinoid signaling and reduced adult neurogenesis in diacylglycerol lipase knock-out mice. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2010;30(6):2017–24.
Nagayama T, Sinor AD, Simon RP, Chen J, Graham SH, Jin K, et al. Cannabinoids and neuroprotection in global and focal cerebral ischemia and in neuronal cultures. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1999;19(8):2987–95.
Alonso-Alconada D, Alvarez FJ, Alvarez A, Mielgo VE, Goni-de-Cerio F, Rey-Santano MC, et al. The cannabinoid receptor agonist WIN 55,212-2 reduces the initial cerebral damage after hypoxic-ischemic injury in fetal lambs. Brain Res. 2010;1362:150–9.
••Bhattacharyya S, Morrison PD, Fusar-Poli P, Martin-Santos R, Borgwardt S, Winton-Brown T, et al. Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology. 2010;35(3):764–74 This is an important functional neuroimaging study demonstrating the opposing effects of Δ-9-THC and CBD on regional brain functions in healthy men with minimal exposure to cannabis, suggesting their differential effects on symptoms and behaviours and CBD’s ability to block Δ-9-THC’s psychotogenic effects.
Gjerde H, Kinn G. Impairment in drivers due to cannabis in combination with other drugs. Forensic Sci Int. 1991;50(1):57–60.
Vindenes V, Strand DH, Kristoffersen L, Boix F, Morland J. Has the intake of THC by cannabis users changed over the last decade? Evidence of increased exposure by analysis of blood THC concentrations in impaired drivers. Forensic Sci Int. 2013;226(1–3):197–201.
Ashton CH. Pharmacology and effects of cannabis: a brief review. The British journal of psychiatry : the journal of mental science. 2001;178:101–6.
Leweke FM, Piomelli D, Pahlisch F, Muhl D, Gerth CW, Hoyer C, et al. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2:e94.
Burstein S. Cannabidiol (CBD) and its analogs: a review of their effects on inflammation. Bioorg Med Chem. 2015;23(7):1377–85.
Pertwee RG. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br J Pharmacol. 2008;153(2):199–215.
Pertwee RG. The pharmacology and therapeutic potential of cannabidiol. In: Di Marzo V, editor. Cannabinoids. New York, NY: Kluwer Academic/Plenum Publishers; 2004. p. 1–52.
Tait RJ, Caldicott D, Mountain D, Hill SL, Lenton S. A systematic review of adverse events arising from the use of synthetic cannabinoids and their associated treatment. Clinical toxicology (Philadelphia, Pa). 2016;54(1):1–13.
Galve-Roperh I, Palazuelos J, Aguado T, Guzman M. The endocannabinoid system and the regulation of neural development: potential implications in psychiatric disorders. Eur Arch Psychiatry Clin Neurosci. 2009;259(7):371–82.
Vinod KY, Hungund BL. Role of the endocannabinoid system in depression and suicide. Trends Pharmacol Sci. 2006;27(10):539–45.
Herkenham M, Lynn AB, Little MD, Johnson MR, Melvin LS, de Costa BR, et al. Cannabinoid receptor localization in brain. Proc Natl Acad Sci U S A. 1990;87(5):1932–6.
Hill MN, Carrier EJ, McLaughlin RJ, Morrish AC, Meier SE, Hillard CJ, et al. Regional alterations in the endocannabinoid system in an animal model of depression: effects of concurrent antidepressant treatment. J Neurochem. 2008;106(6):2322–36.
Mangieri RA, Piomelli D. Enhancement of endocannabinoid signaling and the pharmacotherapy of depression. Pharmacol Res. 2007;56(5):360–6.
Giuffrida A, Leweke FM, Gerth CW, Schreiber D, Koethe D, Faulhaber J, et al. Cerebrospinal anandamide levels are elevated in acute schizophrenia and are inversely correlated with psychotic symptoms. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology. 2004;29(11):2108–14.
Eggan SM, Hashimoto T, Lewis DA. Reduced cortical cannabinoid 1 receptor messenger RNA and protein expression in schizophrenia. Arch Gen Psychiatry. 2008;65(7):772–84.
Yucel M, Solowij N, Respondek C, Whittle S, Fornito A, Pantelis C, et al. Regional brain abnormalities associated with long-term heavy cannabis use. Arch Gen Psychiatry. 2008;65(6):694–701.
Realini N, Rubino T, Parolaro D. Neurobiological alterations at adult age triggered by adolescent exposure to cannabinoids. Pharmacol Res. 2009;60(2):132–8.
Bava S, Tapert SF. Adolescent brain development and the risk for alcohol and other drug problems. Neuropsychol Rev. 2010;20(4):398–413.
O’Shea M, Singh ME, McGregor IS, Mallet PE. Chronic cannabinoid exposure produces lasting memory impairment and increased anxiety in adolescent but not adult rats. Journal of psychopharmacology (Oxford, England). 2004;18(4):502–8.
••D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology. 2004;29(8):1558–72 This important human laboratory study documented the psychotogenic effects of purified THC given intravenously to healthy human subjects, and assisted in our understanding of mechanisms by which THC may cause psychosis and contribute to the genesis of schizophrenia.
Andreasson S, Allebeck P, Engstrom A, Rydberg U. Cannabis and schizophrenia. A longitudinal study of Swedish conscripts. Lancet. 1987;2(8574):1483–6.
Fergusson DM, Horwood LJ, Swain-Campbell NR. Cannabis dependence and psychotic symptoms in young people. Psychol Med. 2003;33(1):15–21.
Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–28.
Caspi A, Moffitt TE, Cannon M, McClay J, Murray R, Harrington H, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry. 2005;57(10):1117–27.
•Di Forti M, Iyegbe C, Sallis H, Kolliakou A, Falcone MA, Paparelli A, et al. Confirmation that the AKT1 (rs2494732) genotype influences the risk of psychosis in cannabis users. Biol Psychiatry. 2012;72(10):811–6 This is an important case-control study supporting the interaction between the variation at the AKT1 rs2494732 single nucleotide polymorphism increasing the risk of developing a psychotic disorder in canabis users.
Otten R, Huizink AC, Monshouwer K, Creemers HE, Onrust S. Cannabis use and symptoms of anxiety in adolescence and the moderating effect of the serotonin transporter gene. Addiction Biol. 2016.
Feingold D, Weiser M, Rehm J, Lev-Ran S. The association between cannabis use and anxiety disorders: results from a population-based representative sample. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology. 2016;26(3):493–505.
Zvolensky MJ, Bernstein A, Sachs-Ericsson N, Schmidt NB, Buckner JD, Bonn-Miller MO. Lifetime associations between cannabis, use, abuse, and dependence and panic attacks in a representative sample. J Psychiatr Res. 2006;40(6):477–86.
Kessler RC, Andrade LH, Bijl RV, Offord DR, Demler OV, Stein DJ. The effects of co-morbidity on the onset and persistence of generalized anxiety disorder in the ICPE surveys. International consortium in psychiatric epidemiology. Psychol Med. 2002;32(7):1213–25.
Danielsson AK, Lundin A, Agardh E, Allebeck P, Forsell Y. Cannabis use, depression and anxiety: a 3-year prospective population-based study. J Affect Disord. 2016;193:103–8.
Chambers R, Krystal JH, Self DA. A neurobiological basis for substance abuse comorbidity in schizophrenia. Biol Psychiatry. 2001;50:71–83.
Steimer T. The biology of fear- and anxiety-related behaviors. Dialogues Clin Neurosci. 2002;4(3):231–49.
Sripada RK, Garfinkel SN, Liberzon I. Avoidant symptoms in PTSD predict fear circuit activation during multimodal fear extinction. Front Hum Neurosci. 2013;7:672.
Cougle JR, Bonn-Miller MO, Vujanovic AA, Zvolensky MJ, Hawkins KA. Posttraumatic stress disorder and cannabis use in a nationally representative sample. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2011;25(3):554–8.
Fraser GA. The use of a synthetic cannabinoid in the management of treatment-resistant nightmares in posttraumatic stress disorder (PTSD). CNS neuroscience & therapeutics. 2009;15(1):84–8.
Roitman P, Mechoulam R, Cooper-Kazaz R, Shalev A. Preliminary, open-label, pilot study of add-on oral delta9-tetrahydrocannabinol in chronic post-traumatic stress disorder. Clinical drug investigation. 2014;34(8):587–91.
•Neumeister A, Normandin MD, Pietrzak RH, Piomelli D, Zheng MQ, Gujarro-Anton A, et al. Elevated brain cannabinoid CB1 receptor availability in post-traumatic stress disorder: a positron emission tomography study. Mol Psychiatry. 2013;18(9):1034–40 This is an important in vivo imaging study using PET and the CB1-selective radioligand [11C]OMAR which suggests abnormalities of the CB1 receptor-mediated signing in the pathophysiology of PTSD.
Johnson MJ, Pierce JD, Mavandadi S, Klaus J, Defelice D, Ingram E, et al. Mental health symptom severity in cannabis using and non-using veterans with probable PTSD. J Affect Disord. 2016;190:439–42.
Greer GR, Grob CS, Halberstadt AL. PTSD symptom reports of patients evaluated for the New Mexico medical cannabis program. J Psychoactive Drugs. 2014;46(1):73–7.
Wilkinson ST, Radhakrishnan R, D’Souza DC. Impact of cannabis use on the development of psychotic disorders. Current addiction reports. 2014;1(2):115–28.
Lev-Ran S, Le Foll B, McKenzie K, George TP, Rehm J. Bipolar disorder and co-occurring cannabis use disorders: characteristics, co-morbidities and clinical correlates. Psychiatry Res. 2013;209(3):459–65.
•Lev-Ran S, Roerecke M, Le Foll B, George TP, McKenzie K, Rehm J. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med. 2014;44(4):797–810 In this systematic review and meta-analysis of longitudinal studies, the authors report the association between cannabis use and depression. The results found evidence for the use of cannabis being associated with an increased risk of developing depressive disorder.
Kvitland LR, Melle I, Aminoff SR, Demmo C, Lagerberg TV, Andreassen OA, et al. Continued cannabis use at one year follow up is associated with elevated mood and lower global functioning in bipolar I disorder. BMC psychiatry. 2015;15:11.
Gibbs M, Winsper C, Marwaha S, Gilbert E, Broome M, Singh SP. Cannabis use and mania symptoms: a systematic review and meta-analysis. J Affect Disord. 2015;171:39–47.
Kolla NJ, van der Maas M, Toplak ME, Erickson PG, Mann RE, Seeley J, et al. Adult attention deficit hyperactivity disorder symptom profiles and concurrent problems with alcohol and cannabis: sex differences in a representative, population survey. BMC psychiatry. 2016;16:50.
Bidwell LC, Henry EA, Willcutt EG, Kinnear MK, Ito TA. Childhood and current ADHD symptom dimensions are associated with more severe cannabis outcomes in college students. Drug Alcohol Depend. 2014;135:88–94.
Fergusson DM, Boden JM. Cannabis use and adult ADHD symptoms. Drug Alcohol Depend. 2008;95(1–2):90–6.
Arias F, Szerman N, Vega P, Mesias B, Basurte I, Morant C, et al. Abuse or dependence on cannabis and other psychiatric disorders. Madrid study on dual pathology prevalence. Actas espanolas de psiquiatria. 2013;41(2):122–9.
Taylor J. Substance use disorders and cluster B personality disorders: physiological, cognitive, and environmental correlates in a college sample. The American journal of drug and alcohol abuse. 2005;31(3):515–35.
Fridberg DJ, Vollmer JM, O’Donnell BF, Skosnik PD. Cannabis users differ from non-users on measures of personality and schizotypy. Psychiatry Res. 2011;186(1):46–52.
•Agrawal A, Budney AJ, Lynskey MT. The co-occurring use and misuse of cannabis and tobacco: a review. Addiction. 2012;107(7):1221–33 This is an important review examining the co-use of cannabis and tobacco and outlining the mechanisms that link theses drugs to each other. It outline advances in our understaning of the mechanisms linking cannabis and tobacco use co-use.
Barrett SP, Darredeau C, Pihl RO. Patterns of simultaneous polysubstance use in drug using university students. Hum Psychopharmacol Clin Exp. 2006;21(4):255–63.
Philibert RA, Gunter TD, Beach SR, Brody GH, Hollenbeck N, Andersen A, et al. The role of GABRA2 on risk for alcohol, nicotine and cannabis dependence in the Iowa adoption studies. Psychiatr Genet. 2009;19(2):91.
Copersino ML, Boyd SJ, Tashkin DP, Huestis MA, Heishman SJ, Dermand JC, et al. Cannabis withdrawal among non-treatment-seeking adult cannabis users. Am J Addict. 2006;15(1):8–14.
Budney AJ, Hughes JR. The cannabis withdrawal syndrome. Curr Opin Psychiatry. 2006;19(3):233–8.
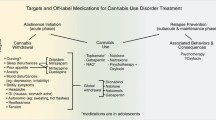
Carroll KM, Onken LS. Behavioral therapies for drug abuse. Am J Psychiatry. 2005;162(8):1452–60.
Gates PJ, Sabioni P, Copeland J, Le Foll B, Gowing L. Psychosocial interventions for cannabis use disorder. Cochrane Database Syst Rev. 2016;5:CD005336.
Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165(2):179–87.
•Allsop D, Copeland J, Linteris N, Dunlop AJ, Montebello M, Sadler C, et al. Nabiximols as an agonist replacement therapy during cannabis withdrawal: a randomized clinical trial. JAMA Psychiatry. 2014;71:281–91 This is an important double-blind, randomized clinical trial examining the effects of nabiximols as a potential agonist medication for cannabis withdrawal. The results suggest important roles for use of agonist substitution therapy for cannabis withdrawal management.
Trigo J, Soliman, A, Quilty, LC, Staois, G, Fischer, B, George, TP, Rehm, J et al. Sativex associated with behavioral-relapse prevention strategy as treatment for cannabis dependence: a case series. J Addict Med. 2016.
Grall-Bronnec M, Sauvaget A. The use of repetitive transcranial magnetic stimulation for modulating craving and addictive behaviours: a critical literature review of efficacy, technical and methodological considerations. Neurosci Biobehav Rev. 2014;47:592–613.
Mason BL, Mustafa A, Filbey F, Brown ES. Novel Pharmacotherapeutic interventions for cannabis use disorder. Current Addiction Reports. 2016;3(2):214–20.
Allsop DJ, Lintzeris N, Copeland J, Dunlop A, McGregor IS. Cannabinoid replacement therapy (CRT): nabiximols (sativex) as a novel treatment for cannabis withdrawal. Clin Pharmacol Ther. 2015;97(6):571–4.
Budney AJ, Vandrey RG, Hughes JR, Moore BA, Bahrenburg B. Oral delta-9-tetrahydrocannabinol suppresses cannabis withdrawal symptoms. Drug Alcohol Depend. 2007;86(1):22–9.
•Haney M, Cooper ZD, Bedi G, Vosburg SK, Comer SD, Foltin RW. Nabilone decreases marijuana withdrawal and a laboratory measure of marijuana relapse. Neuropsychopharmacology. 2013;38(8):1557–65 This is an important placebo-controlled trial examining the effects of repeated nabilone administration in decreasing symptoms of marijuana withdrawal and marijuana relapse. The results support nabilone as a potential medication for cannabis use disorder.
Cahn W, Hulshoff Pol HE, Caspers E, van Haren NE, Schnack HG, Kahn RS. Cannabis and brain morphology in recent-onset schizophrenia. Schizophr Res. 2004;67(2–3):305–7.
Wobrock T, Sittinger H, Behrendt B, D’Amelio R, Falkai P. Comorbid substance abuse and brain morphology in recent-onset psychosis. Eur Arch Psychiatry Clin Neurosci. 2009;259(1):28–36.
Rabin RA, Zakzanis KK, George TP. The effects of cannabis use on neurocognition in schizophrenia: a meta-analysis. Schizophr Res. 2011;128(1–3):111–6.
Budney AJ, Higgins ST, Radonovich KJ, Novy PL. Adding voucher-based incentives to coping skills and motivational enhancement improves outcomes during treatment for marijuana dependence. J Consult Clin Psychol. 2000;68(6):1051–61.
Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68(5):898–908.
Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Coping skills training and contingency management treatments for marijuana dependence: exploring mechanisms of behavior change. Addiction. 2008;103(4):638–48.
Budney AJ, Stanger C, Tilford JM, Scherer EB, Brown PC, Li Z, et al. Computer-assisted behavioral therapy and contingency management for cannabis use disorder. Psychology of addictive behaviors : journal of the Society of Psychologists in Addictive Behaviors. 2015;29(3):501–11.
Stanger C, Ryan SR, Scherer EA, Norton GE, Budney AJ. Clinic- and home-based contingency management plus parent training for adolescent cannabis use disorders. J Am Acad Child Adolesc Psychiatry. 2015;54(6):445–53.e2.
Trigo JM, Lagzdins D, Rehm J, Selby P, Gamaleddin I, Fischer B, et al. Effects of fixed or self-titrated dosages of sativex on cannabis withdrawal and cravings. Drug Alcohol Depend. 2016;161:298–306.
Cornelius JR, Bukstein OG, Douaihy AB, Clark DB, Chung TA, Daley DC, et al. Double-blind fluoxetine trial in comorbid MDD-CUD youth and young adults. Drug Alcohol Depend. 2010;112(1–2):39–45.
•Levin FR, Mariani J, Brooks DJ, Pavlicova M, Nunes EV, Agosti V, et al. A randomized double-blind, placebo-controlled trial of venlafaxine-extended release for co-occurring cannabis dependence and depressive disorders. Addiction. 2013;108(6):1084–94 This is an important double-blind, placebo-controlled trial evaluating venlafaxine-extended release (VEN-XR) as a treatment for cannabis use disorder and concurrent depressive disorder. The results found that VEN-XR was not effective at reducing depression and may lead to an increase in cannabis use in depressed, cannabis-dependent patients.
Weinstein AM, Miller H, Bluvstein I, Rapoport E, Schreiber S, Bar-Hamburger R, et al. Treatment of cannabis dependence using escitalopram in combination with cognitive-behavior therapy: a double-blind placebo-controlled study. The American journal of drug and alcohol abuse. 2014;40(1):16–22.
Carpenter KM, McDowell D, Brooks DJ, Cheng WY, Levin FR. A preliminary trial: double-blind comparison of nefazodone, bupropion-SR, and placebo in the treatment of cannabis dependence. The American journal on addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2009;18(1):53–64.
Penetar DM, Looby AR, Ryan ET, Maywalt MA, Lukas SE. Bupropion reduces some of the symptoms of marihuana withdrawal in chronic marihuana users: a pilot study. Substance abuse : research and treatment. 2012;6:63–71.
Haney M, Hart CL, Vosburg SK, Comer SD, Reed SC, Cooper ZD, et al. Effects of baclofen and mirtazapine on a laboratory model of marijuana withdrawal and relapse. Psychopharmacology. 2010;211(2):233–44.
Winstock AR, Lea T, Copeland J. Lithium carbonate in the management of cannabis withdrawal in humans: an open-label study. Journal of psychopharmacology (Oxford, England). 2009;23(1):84–93.
McRae-Clark AL, Carter RE, Killeen TK, Carpenter MJ, Wahlquist AE, Simpson SA, et al. A placebo-controlled trial of buspirone for the treatment of marijuana dependence. Drug Alcohol Depend. 2009;105(1–2):132–8.
Mariani JJ, Pavlicova M, Mamczur AK, Bisaga A, Nunes EV, Levin FR. Open-label pilot study of quetiapine treatment for cannabis dependence. The American journal of drug and alcohol abuse. 2014;40(4):280–4.
Schnell T, Koethe D, Krasnianski A, Gairing S, Schnell K, Daumann J, et al. Ziprasidone versus clozapine in the treatment of dually diagnosed (DD) patients with schizophrenia and cannabis use disorders: a randomized study. The American journal on addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2014;23(3):308–12.
•Mason BJ, Crean R, Goodell V, Light JM, Quello S, Shadan F, et al. A proof-of-concept randomized controlled study of gabapentin: effects on cannabis use, withdrawal and executive function deficits in cannabis-dependent adults. Neuropsychopharmacology. 2012;37(7):1689–98 In this important phase IIa proof-of-concept pilot study, the authors examined gabapentin for the treatment of cannabis dependence. The results provide preliminary support for safety and efficacy of gabapentin for treatment of cannabis dependence and further assists in our understanding for the treatment of cannabis use disorder.
Acknowledgments
This work was supported in part by Canadian Institutes of Health Research (CIHR) grant MOP no. 115145 (to TPG) and Brain and Behavior Research Young Investigator Award (to MSB) and a Science Without Borders (SWB) scholarship grant no. 211629/2014-6 (to MPH) from the Brazilian National Council for Scientific and Technological Development (CNPq, Brazil).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mariana P. Halah, Michelle P. Zochniak, Dr. Mera S. Barr, and Dr. Tony P. George declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cannabis
Rights and permissions
About this article
Cite this article
Halah, M.P., Zochniak, M.P., Barr, M.S. et al. Cannabis Use and Psychiatric Disorders: Implications for Mental Health and Addiction Treatment. Curr Addict Rep 3, 450–462 (2016). https://doi.org/10.1007/s40429-016-0128-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-016-0128-5