Abstract
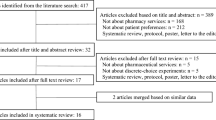
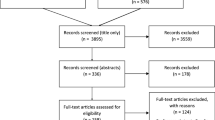
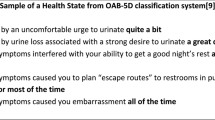
Nonadherence is a global problem undermining the cost-effectiveness of evidence-based medications. Aligning treatment choices with patient preferences may promote adherent behaviour: eliciting patient treatment preferences may help resolve the problem of nonadherence. As there is no reliable measure of nonadherent behaviour that can be used to derive preferences, stated-preference techniques offer a robust alternative. To understand patient preferences in medication nonadherence, we systematically appraised full-text English studies (from database inception to 24 February 2014) involving participants evaluating hypothetical scenarios to elicit preferences as an explicit means to understand medication nonadherence. Study characteristics (e.g. setting, disease, stated-preference method), attribute type and influence on choice were extracted. Seventeen full-text articles (4,456 patients) were included in the review, which reports stated-preference elicitation studies across a wide range of chronic and acute conditions. All studies were conducted in high-income settings. The influence of drug-related factors was predominant in patients’ preferences for treatment. Patients preferred efficacious over safe medications except when considering the duration of therapy, but dosing and cost appeared more important when contemplating adherence. Patient characteristics, particularly medication experience, significantly influenced preferences. A disparity between stated preferences for treatment and adherence was reported. When using stated-preference techniques to understand nonadherence, this manuscript highlights that there is much room for methodological development. Studies outside of high-income settings are needed, particularly in relation to chronic diseases, for which nonadherence poses a substantial economic burden to health systems and patients. To inform the problem of sustaining adherence, prospective research is needed to understand how preferences change with time. The usefulness of stated-preference techniques to inform policy and practice requires a better understanding of how stated preferences relate to actual adherence behaviour.

Similar content being viewed by others
References
Horne R, Weinman J, Barber N, Elliott R, Morgan M. Concordance, adherence and compliance in medicine taking. London: National Co-ordinating Centre for NHS Delivery and Organisation R & D (NCCSDO), London School of Hygiene and Tropical Medicine; 2005.
Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence (update of Cochrane Database Syst Rev. 2005;(4):CD000011; PMID: 16235271). Cochrane Database Syst Rev. 2008;2:CD000011. doi:10.1002/14651858.CD000011.pub3.
Lehane E, McCarthy G. An examination of the intentional and unintentional aspects of medication non-adherence in patients diagnosed with hypertension. J Clin Nurs. 2007;16(4):698–706. doi:10.1111/j.1365-2702.2005.01538.x.
Daleboudt GMN, Broadbent E, McQueen F, Kaptein AA. Intentional and unintentional treatment nonadherence in patients with systemic lupus erythematosus. Arthritis Care Res. 2011;63(3):342–50. doi:10.1002/acr.20411.
Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: how unintentional is it really? BMC Health Serv Res. 2012;12:98. doi:10.1186/1472-6963-12-98.
Goren A, Gupta S, Dibonaventura MD. Demographic and health characteristics associated with intentional and unintentional non-adherence among costly chronic conditions in the United States. Value Health. 2012;15(4):A197. doi:10.1016/j.jval.2012.03.1064.
Goren A, Isherwood G, Vietri J. Intentional and unintentional non-adherence differ across prevalent conditions in a Russian patient population. Value Health. 2012;15(7):A541. doi:10.1016/j.jval.2012.08.1903.
Goren A, Vietri J, Madi O. Intentional and unintentional non-adherence and patient characteristics associated with treatment in rheumatoid arthritis patients. Value Health. 2012;15(4):A41. doi:10.1016/j.jval.2012.03.232.
Lindquist L, Go L, Jain N, Baker D. Relationship of health literacy to intentional and unintentional non-adherence of hospital discharge instructions. J Gen Intern Med. 2010;25:S382–3. doi:10.1007/s11606-011-1886-3.
Mo PKH, Mak WWS. Intentionality of medication non-adherence among individuals living with HIV/AIDS in Hong Kong. AIDS Care. 2009;21(6):785–95. doi:10.1080/09540120802511968.
Norton WE, Amico KR, Fisher WA, Shuper PA, Ferrer RA, Cornman DH, et al. Information-motivation-behavioral skills barriers associated with intentional versus unintentional ARV non-adherence behavior among HIV+ patients in clinical care. AIDS Care. 2010;22(8):979–87. doi:10.1080/09540121003758630.
Radcliffe EJ, Morgan M, Wolfe C. Medicines knowledge, concerns and needs among stroke patients aged 75 years and over compared with patients with other chronic conditions. Cerebrovasc Dis. 2010;29:326. doi:10.1159/000321266.
Stack RJ, Bundy CE, Eliott RA, New JP, Gibson M, Noyce PR. Intentional and unintentional non-adherence in community dwelling people with type 2 diabetes: the effect of varying numbers of medicines. Br J Diabetes Vasc Dis. 2010;10(3):148–52. doi:10.1177/1474651409357034.
Sabate E. Adherence to long term therapies: evidence for action. http://www.who.int/chronic_conditions/adherencereport/en/. Geneva: World Health Organisation; 2003.
Bowry AD, Shrank WH, Lee JL, Stedman M, Choudhry NK. A systematic review of adherence to cardiovascular medications in resource-limited settings. J Gen Intern Med. 2011;26(12):1479–91. doi:10.1007/s11606-011-1825-3.
Simons LA, Ortiz M, Calcino G. Persistence with antihypertensive medication: Australia-wide experience, 2004–2006. Med J Aust. 2008;188(4):224–7.
Yeaw J, Benner JS, Walt JG, Sian S, Smith DB. Comparing adherence and persistence across 6 chronic medication classes. J Manag Care Pharm. 2009;15(9):728–40.
Elliott R. Non-adherence to medicines: not solved but solvable. J Health Serv Res Policy. 2009;14(1):58–61. doi:10.1258/jhsrp.2008.008088.
Krueger KP, Berger BA, Felkey B. Medication adherence and persistence: a comprehensive review. Adv Ther. 2005;22(4):313–56.
Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc Sci Med. 2005;61(1):133–55. doi:10.1016/j.socscimed.2004.11.063.
Kalichman SC, Grebler T. Stress and poverty predictors of treatment adherence among people with low-literacy living with HIV/AIDS. Psychosom Med. 2010;72(8):810–6. doi:10.1097/PSY.0b013e3181f01be3.
Parashar S, Palmer AK, O’Brien N, Chan K, Shen A, Coulter S, et al. Sticking to it: the effect of maximally assisted therapy on antiretroviral treatment adherence among individuals living with HIV who are unstably housed. AIDS Behav. 2011;15(8):1612–22. doi:10.1007/s10461-011-0026-8.
Shimony A, Zahger D, Ilia R, Shalev A, Cafri C. Impact of the community’s socioeconomic status on characteristics and outcomes of patients undergoing percutaneous coronary intervention. Int J Cardiol. 2010;144(3):379–82. doi:10.1016/j.ijcard.2009.04.033.
Wong MC, Jiang JY, Griffiths SM. Factors associated with compliance to thiazide diuretics among 8551 Chinese patients. J Clin Pharm Ther. 2011;36(2):179–86. doi:10.1111/j.1365-2710.2010.01174.x.
Wu JR, Moser DK, Chung ML, Lennie TA. Predictors of medication adherence using a multidimensional adherence model in patients with heart failure. J Card Fail. 2008;14(7):603–14. doi:10.1016/j.cardfail.2008.02.011.
DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42(3):200–9.
Lemstra M, Blackburn D. Nonadherence to statin therapy: discontinuation after a single fill. Can J Cardiol. 2012;28(5):567–73. doi:10.1016/j.cjca.2012.03.018.
DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40(9):794–811. doi:10.1097/01.MLR.0000024612.61915.2D.
Golay A. Pharmacoeconomic aspects of poor adherence: can better adherence reduce healthcare costs? J Med Econ. 2011;14(5):594–608. doi:10.3111/13696998.2011.597808.
Belsey JD. Optimizing adherence in hypertension: a comparison of outcomes and costs using single tablet regimens vs individual component regimens. J Med Econ. 2012;15(5):897–905. doi:10.3111/13696998.2012.689792.
Dilokthornsakul P, Chaiyakunapruk N, Nimpitakpong P, Jeanpeerapong N, Sruamsiri R. The effects of medication supply on hospitalizations and health-care costs in patients with chronic heart failure. Value Health. 2012;15(1 Suppl):S9–14. doi:10.1016/j.jval.2011.11.019.
Sherrill B, Halpern M, Khan S, Zhang J, Panjabi S. Single-pill vs free-equivalent combination therapies for hypertension: a meta-analysis of health care costs and adherence. J Clin Hypertens (Greenwich). 2011;13(12):898–909. doi:10.1111/j.1751-7176.2011.00550.x.
Bosworth HB, Granger BB, Mendys P, Brindis R, Burkholder R, Czajkowski SM, et al. Medication adherence: a call for action. Am Heart J. 2011;162(3):412–24. doi:10.1016/j.ahj.2011.06.007.
Jha AK, Aubert RE, Yao J, Teagarden JR, Epstein RS. Greater adherence to diabetes drugs is linked to less hospital use and could save nearly $5 billion annually. Health Aff. 2012;31(8):1836–46. doi:10.1377/hlthaff.2011.1198.
Bridges JF, Hauber AB, Marshall D, Lloyd A, Prosser LA, Regier DA, et al. Conjoint analysis applications in health—a checklist: a report of the ISPOR Good Research Practices for Conjoint Analysis Task Force. Value Health. 2011;14(4):403–13. doi:10.1016/j.jval.2010.11.013.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–77.
Louviere JJ, Lancsar E. Choice experiments in health: the good, the bad, the ugly and toward a brighter future. Health Econ Policy Law. 2009;4(Pt 4):527–46. doi:10.1017/S1744133109990193.
Ryan M. A role for conjoint analysis in technology assessment in health care? Int J Technol Assess Health Care. 1999;15(3):443–57.
Marshall D, Bridges JFP, Hauber B, Cameron R, Donnalley L, Fyie K, et al. Conjoint analysis applications in health––how are studies being designed and reported? An update on current practice in the published literature between 2005 and 2008. Patient Patient Cent Outcomes Res. 2010;3(4):249–56. doi:10.2165/11539650-000000000-00000.
Osterberg L, Blaschke T. Adherence to medication. New Engl J Med. 2005;353(5):487–97. doi:10.1056/NEJMra050100.
de Bekker-Grob EW, Essink-Bot ML, Meerding WJ, Pols HA, Koes BW, Steyerberg EW. Patients’ preferences for osteoporosis drug treatment: a discrete choice experiment. Osteoporos Int. 2008;19(7):1029–37. doi:10.1007/s00198-007-0535-5.
Hodgkins P, Swinburn P, Solomon D, Yen L, Dewilde S, Lloyd A. Patient preferences for first-line oral treatment for mild-to-moderate ulcerative colitis: a discrete-choice experiment. Patient. 2012;5(1):33–44. doi:10.2165/11595390-000000000-00000.
Johnson FR, Ozdemir S, Manjunath R, Hauber AB, Burch SP, Thompson TR. Factors that affect adherence to bipolar disorder treatments: a stated-preference approach. Med Care. 2007;45(6):545–52. doi:10.1097/MLR.0b013e318040ad90.
Kellett N, West F, Finlay AY. Conjoint analysis: a novel, rigorous tool for determining patient preferences for topical antibiotic treatment for acne. A randomised controlled trial. Br J Dermatol. 2006;154(3):524–32. doi:10.1111/j.1365-2133.2005.07047.x.
King MT, Hall J, Lancsar E, Fiebig D, Hossain I, Louviere J, et al. Patient preferences for managing asthma: results from a discrete choice experiment. Health Econ. 2007;16(7):703–17. doi:10.1002/hec.1193.
Laba TL, Brien JA, Fransen M, Jan S. Patient preferences for adherence to treatment for osteoarthritis: the MEdication Decisions in Osteoarthritis Study (MEDOS). BMC Musculoskelet Disord. 2013;14:160. doi:10.1186/1471-2474-14-160.
Laba TL, Brien JA, Jan S. Understanding rational non-adherence to medications. A discrete choice experiment in a community sample in Australia. BMC Fam Pract. 2012;13:61. doi:10.1186/1471-2296-13-61.
Lancsar EJ, Hall JP, King M, Kenny P, Louviere JJ, Fiebig DG, et al. Using discrete choice experiments to investigate subject preferences for preventive asthma medication. Respirology. 2007;12(1):127–36. doi:10.1111/j.1440-1843.2006.01005.x.
Mahadevia PJ, Shah S, Leibman C, Kleinman L, O’Dowd L. Patient preferences for sensory attributes of intranasal corticosteroids and willingness to adhere to prescribed therapy for allergic rhinitis: a conjoint analysis. Ann Allergy Asthma Immunol. 2004;93(4):345–50. doi:10.1016/S1081-1206(10)61393-2.
Schaarschmidt ML, Schmieder A, Umar N, Terris D, Goebeler M, Goerdt S, et al. Patient preferences for psoriasis treatments: process characteristics can outweigh outcome attributes. Arch Dermatol. 2011;147(11):1285–94. doi:10.1001/archdermatol.2011.309.
Schmieder A, Schaarschmidt ML, Umar N, Terris DD, Goebeler M, Goerdt S, et al. Comorbidities significantly impact patients’ preferences for psoriasis treatments. J Am Acad Dermatol. 2012;67(3):363–72. doi:10.1016/j.jaad.2011.08.023.
Schackman BR, Teixeira PA, Weitzman G, Mushlin AI, Jacobson IM. Quality-of-life tradeoffs for hepatitis C treatment: do patients and providers agree? Med Decis Mak. 2008;28(2):233–42. doi:10.1177/0272989X07311753.
Gueylard Chenevier D, LeLorier J. A willingness-to-pay assessment of parents’ preference for shorter duration treatment of acute otitis media in children. Pharmacoeconomics. 2005;23(12):1243–55. http://link.springer.com/journal/volumesAndIssues/40273.
Brett Hauber A, Gonzalez JM, Coombs J, Sirulnik A, Palacios D, Scherzer N. Patient preferences for reducing toxicities of treatments for gastrointestinal stromal tumor (GIST). Patient Prefer Adher. 2011;5:307–14. doi:10.2147/PPA.S20445.
Brett Hauber A, Mohamed AF, Beam C, Medjedovic J, Mauskopf J. Patient preferences and assessment of likely adherence to hepatitis C virus treatment. J Viral Hepat. 2011;18(9):619–27. doi:10.1111/j.1365-2893.2010.01343.x.
Hauber AB, Han S, Yang JC, Gantz I, Tunceli K, Gonzalez JM, et al. Effect of pill burden on dosing preferences, willingness to pay, and likely adherence among patients with type 2 diabetes. Patient Prefer Adher. 2013;7:937–49. doi:10.2147/PPA.S43465.
Hauber AB, Mohamed AF, Johnson FR, Falvey H. Treatment preferences and medication adherence of people with type 2 diabetes using oral glucose-lowering agents. Diabet Med. 2009;26(4):416–24. doi:10.1111/j.1464-5491.2009.02696.x.
Thom S, Poulter N, Field J, Patel A, Prabhakaran D, Stanton A, et al. Effects of a fixed-dose combination strategy on adherence and risk factors in patients with or at high risk of CVD: the UMPIRE randomized clinical trial. JAMA. 2013;310(9):918–29. doi:10.1001/jama.2013.277064.
Laba TL. Medication adherence in chronic disease. Ph.D. thesis. Sydney: Faculty of Pharmacy, University of Sydney; 2013. http://hdl.handle.net/2123/9546.
Jan S, Usherwood T, Brien JA, Peiris D, Rose J, Hayman N, et al. What determines adherence to treatment in cardiovascular disease prevention? Protocol for a mixed methods preference study. BMJ Open. 2011;1(2). doi:10.1136/bmjopen-2011-000372.
Acknowledgements
There are no conflicts of interest, including nonfinancial, to declare by TL, BE, MK or SJ.
TL is funded by a National Health and Medical Research Council (NHMRC) Health Economics capacity building grant (application no. 57132). BE is funded by an NHMRC Sidney Sax Public Health Early Career Fellowship. SJ is funded by a NHMRC Senior Research Fellowship.
TL led the design, data collection and analysis, wrote the first draft, coordinated the subsequent revisions and is the guarantor of this manuscript. BE, MK and SJ contributed to the design and analysis, and to the writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Laba, TL., Essue, B., Kimman, M. et al. Understanding Patient Preferences in Medication Nonadherence: A Review of Stated Preference Data. Patient 8, 385–395 (2015). https://doi.org/10.1007/s40271-014-0099-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-014-0099-3