Abstract
Background
Sleep complaints and the consumption of medications for sleep are common in older adults. Falls are also a significant concern for older adults and sedative use has been identified as a risk factor for falls. Sleep quality is a potential confounder in studies evaluating the relationship between sleep medication use and falls. However, very few studies have assessed the combined impact of sleep medication use and sleep quality on the risk of falls.
Objective
The objective of this study was to evaluate the association between sleep medication use, poor sleep quality, and falls in community-dwelling older adults.
Methods
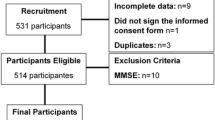
This was a multicenter, 6-month prospective cohort study conducted in senior housings settings in central Virginia, USA. Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) and a medication review was conducted. Data regarding falls were collected over 6 months by use of a diary. Logistic regression modeling was used to examine the effects of poor sleep quality, sleep medication use, and both, on the risk of falls.
Results
Among 113 independently living older adults (mean age ± standard deviation 81.1 ± 8.6), 46.9 % fell at least once during a 6-month period; 62.8 % (n = 71) had poor sleep quality, and 44.2 % (n = 50) used medications or treatments to aid sleep. Compared with participants reporting good sleep quality and no sleep medication use, those who reported poor sleep quality and sleep medication use had an increased risk of falls after adjusting for covariates (odds ratio 3.23, 95 % confidence interval 1.05–9.91). The group with good sleep quality and sleep medication use, as well as the group with poor sleep quality and no sleep medication use had no significantly greater risk for falls compared with the group with good sleep quality and no sleep medication use.
Conclusion
A combined effect of sleep quality and sleep medication use on the risk of falls suggests that medication effectiveness may be an important factor to consider in understanding the risk of falls associated with sedative medications.

Similar content being viewed by others
References
Inouye SK, Brown CJ, Tinetti ME. Medicare nonpayment, hospital falls, and unintended consequences. N Engl J Med. 2009;360(23):2390–3.
Van Nieuwenhuizen RC, van Dijk N, van Breda FG, et al. Assessing the prevalence of modifiable risk factors in older patients visiting an ED due to a fall using the CAREFALL Triage Instrument. Am J Emerg Med. 2010;28(9):994–1001.
Fabre JM, Ellis R, Kosma M, et al. Falls risk factors and a compendium of falls risk screening instruments. J Geriatr Phys Ther. 2010;33(4):184–97.
Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952–60.
Bloch F, Thibaud M, Dugué B, et al. Psychotropic drugs and falls in the elderly people: updated literature review and meta-analysis. J Aging Health. 2011;23(2):329–46.
Ray WA. Psychotropic drugs and injuries among the elderly: a review. J Clin Psychopharmacol. 1992;12(6):386–96.
Cummings SR, Rubin SM, Black D. The future of hip fractures in the United States. Numbers, costs, and potential effects of postmenopausal estrogen. Clin Orthop Relat Res. 1990;252:163–6.
Ford GA, Hoffman BB, Blaschke TF. Effect of temazepam on blood pressure regulation in healthy elderly subjects. Br J Clin Pharmacol. 1990;29(1):61–7.
Allain H, Bentue-Ferrer D, Polard E, et al. Postural instability and consequent falls and hip fractures associated with use of hypnotics in the elderly: a comparative review. Drugs Aging. 2005;22(9):749–65.
Foley DJ, Monjan AA, Brown SL, et al. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18(6):425–32.
Foley D, Ancoli-Israel S, Britz P, et al. Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America Survey. J Psychosom Res. 2004;56(5):497–502.
Janssens JP, Pautex S, Hilleret H, et al. Sleep disordered breathing in the elderly. Aging (Milano). 2000;12(6):417–29.
Grunstein R. Insomnia. Diagnosis and management. Aust Fam Physician. 2002;31(11):995–1000.
Avidan AY, Fries BE, James ML, et al. Insomnia and hypnotic use, recorded in the minimum data set, as predictors of falls and hip fractures in Michigan nursing homes. J Am Geriatr Soc. 2005;53(6):955–62.
Brassington GS, King AC, Bliwise DL. Sleep problems as a risk factor for falls in a sample of community-dwelling adults aged 64–99 years. J Am Geriatr Soc. 2000;48(10):1234–40.
Helbig AK, Döring A, Heier M, et al. Association between sleep disturbances and falls among the elderly: Results from the German Cooperative Health Research in the Region of Augsburg-Age Study. Sleep Med. 2013;14(12):1356–63.
Teo JS, Briffa NK, Devine A, et al. Do sleep problems or urinary incontinence predict falls in elderly women? Aust J Physiother. 2006;52(1):19–24.
Mesas AE, Lopez-Garcia E, Rodriguez-Artalejo F. Self-reported sleep duration and falls in older adults. J Sleep Res. 2011;20(1 Pt 1):21–7.
Kuo HK, Yang CCH, Yu YH, et al. Gender-specific association between self-reported sleep duration and falls in high-functioning older adults. J Gerontol A Biol Sci Med Sci. 2010;65A(2):190–6.
Jonker C, Geerlings MI, Schmand B. Are memory complaints predictive for dementia? A review of clinical and population-based studies. Int J Geriatr Psychiatry. 2000;15(11):983–91.
Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Cole JC, Dubois D, Kosinski M. Use of patient-reported sleep measures in clinical trials of pain treatment: a literature review and synthesis of current sleep measures and a conceptual model of sleep disturbance in pain. Clin Ther. 2007;29(Suppl):2580–8.
Russell MA, Hill KD, Blackberry I, et al. The reliability and predictive accuracy of the falls risk for older people in the community assessment (FROP-Com) tool. Age Ageing. 2008;37(6):634–9.
World Health Organization. WHO global report on falls prevention in older age. Available at: www.who.int/ageing/publications/Falls_prevention7March.pdf. Accessed 14 Sept 2014.
American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4):616–31.
Gooneratne NS, Tavaria A, Patel N, et al. Perceived effectiveness of diverse sleep treatments in older adults. J Am Geriatr Soc. 2011;59(2):297–303.
Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–7.
Tinetti M, Baker D, McAvay G, et al. A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med. 1994;331(13):821–7.
Acknowledgments
The authors gratefully acknowledge the participants in this study.
Authors’ contributions
Dr. Min was involved in the study design, IRB submission, subject recruitment, data collection, data analysis and interpretation, and manuscript writing; Dr. Kirkwood was involved in approving the study methodology, and manuscript review; Dr. Mays was involved in approving the study analysis plan and manuscript review; and Dr. Slattum was involved in approving the design and implementation of the study, IRB submission, data analysis plan, and manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yaena Min, Cynthia K. Kirkwood, Darcy P. Mays, and Patricia W. Slattum declare that they have no conflicts of interest.
Funding
None.
Ethical approval and informed consent
This study was reviewed and approved by the Virginia Commonwealth University IRB. Written informed consent was obtained from all study participants prior to enrollment in the study.
Rights and permissions
About this article
Cite this article
Min, Y., Kirkwood, C.K., Mays, D.P. et al. The Effect of Sleep Medication Use and Poor Sleep Quality on Risk of Falls in Community-Dwelling Older Adults in the US: A Prospective Cohort Study. Drugs Aging 33, 151–158 (2016). https://doi.org/10.1007/s40266-015-0339-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-015-0339-9