Abstract
Objective
This study aimed to elucidate the association between the adverse gastric effects of enteric-coated aspirin and the timing of its administration.
Methods
The study population comprised 572 patients (age range 45–84 years) admitted to Huaiyin Hospital between August 2012 and October 2014. Patients were administered a 100 mg enteric-coated aspirin tablet once daily: before a meal (30 min before a meal), during a meal, after a meal (30 min after a meal), or before sleep, and all patients were followed up for 6–9 months to observe for adverse gastric reactions and other side effects. Gastroscopy was performed if indicated by the patient’s condition after obtaining due consent. In addition, release tests for an enteric-coated aspirin tablet were conducted using the chromatography method.
Results
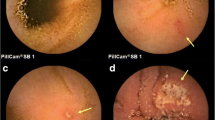
Enteric-coated aspirin tablets released completely, with a release rate of >99 % under 20–120 min at pH > 5.5. Furthermore, the number of patients with recurring adverse stomach reactions was significantly lower in the before-meal and before-sleep groups than that observed in the during-meal and after-meal groups (p < 0.05). No significant between-group differences were observed with respect to damage to other organs. Similarly, the number of patients with gastric lesions was significantly lower in the before-meal and before-sleep groups than that observed in the during-meal and after-meal groups (p < 0.05).
Conclusions
The optimal time for once-daily administration of low-dose enteric-coated aspirin tablets was before a meal or before sleep owing to the increase in pH level during and after meals.
Similar content being viewed by others
References
VanWormer JJ, Greenlee RT, McBride PE, Peppard PE, Malecki KC, Che J, et al. Aspirin for primary prevention of CVD: are the right people using it? J Fam Pract. 2012;61:525–32.
Wu IC, Hsieh HM, Yu FJ, Wu MC, Wu TS, Wu MT. A long-term risk-benefit analysis of low-dose aspirin in primary prevention. Eur J Clin Invest. 2016;46:130–40.
Sutcliffe P, Connock M, Gurung T, Freeman K, Johnson S, Kandala NB, et al. Aspirin for prophylactic use in the primary prevention of cardiovascular disease and cancer: a systematic review and overview of reviews. Health Technol Assess. 2013;17:1–253.
Sutcliffe P, Connock M, Gurung T, Freeman K, Johnson S, Ngianga-Bakwin K, et al. Aspirin in primary prevention of cardiovascular disease and cancer: a systematic review of the balance of evidence from reviews of randomized trials. PLoS One. 2013;8:e81970.
Hayden M, Pignone M, Phillips C, Mulrow C. Aspirin for the primary prevention of cardiovascular events: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;136:161–72.
Hennekens CH, Dalen JE. Aspirin in the primary prevention of cardiovascular disease: current knowledge and future research needs. Trends Cardiovasc Med. 2014;24:360–6.
Antithrombotic Trialists’ (ATT) Collaboration, Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomized trials. Lancet. 2009;373:1849–60.
Kawasaki K, Kurahara K, Yanai S, Kochi S, Fuchigami T, Matsumoto T. Low-dose aspirin and non-steroidal anti-inflammatory drugs increase the risk of bleeding in patients with gastroduodenal ulcer. Dig Dis Sci. 2015;60:1010–5.
Sugano K, Matsumoto Y, Itabashi T, Abe S, Sakaki N, Ashida K, et al. Lansoprazole for secondary prevention of gastric or duodenal ulcers associated with long-term low-dose aspirin therapy: results of a prospective, multicenter, double-blind, randomized, double-dummy, active-controlled trial. J Gastroenterol. 2011;46:724–35.
Kawamura N, Ito Y, Sasaki M, Iida A, Mizuno M, Ogasawara N, et al. Low-dose aspirin-associated upper gastric and duodenal ulcers in Japanese patients with no previous history of peptic ulcers. BMC Res Notes. 2013;6:455.
Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet. 2009;374:1449–61.
Iwakiri R, Higuchi K, Kato M, Fujishiro M, Kinoshita Y, Watanabe T, et al. Randomised clinical trial: prevention of recurrence of peptic ulcers by rabeprazole in patients taking low-dose aspirin. Aliment Pharmacol Ther. 2014;40:780–95.
Uemura N, Sugano K, Hiraishi H, Shimada K, Goto S, Uchiyama S, et al. Risk factor profiles, drug usage, and prevalence of aspirin-associated gastroduodenal injuries among high-risk cardiovascular Japanese patients: the results from the MAGIC study. J Gastroenterol. 2014;49:814–24.
Sakamoto C, Sugano K, Ota S, Takahashi S, Yoshida Y, Tsukui T, et al. Case-control study on the association of upper gastrointestinal bleeding and nonsteroidal anti-inflammatory drugs in Japan. Eur J Clin Pharmacol. 2006;62:765–72.
Nakashima S, Arai S, Mizuno Y, Yoshino K, Ando S, Nakamura Y, et al. A clinical study of Japanese patients with ulcer induced by low-dose aspirin and other non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther. 2005;21:60–6.
Mo C, Sun G, Lu ML, Zhang L, Wang YZ, Sun X, et al. Proton pump inhibitors in prevention of low-dose aspirin-associated upper gastrointestinal injuries. World J Gastroenterol. 2015;21:5382–92.
Sugano K. Prevention of upper gastrointestinal ulcer and complications in low-dose aspirin users. Curr Pharm Des. 2015;21:5082–8.
Nagata N, Niikura R, Aoki T, Sakurai T, Moriyasu S, Shimbo T, et al. Effect of proton-pump inhibitors on the risk of lower gastrointestinal bleeding associated with NSAIDs, aspirin, clopidogrel, and warfarin. J Gastroenterol. 2015;50:1079–86.
Mashita Y, Taniguchi M, Yokota A, Tanaka A, Takeuchi K. Oral but not parenteral aspirin upregulates COX-2 expression in rat stomachs. a relationship between COX-2 expression and PG deficiency. Digestion. 2006;73(2–3):124–32.
Gudis K, Sakamoto C. The role of cyclooxygenase in gastric mucosal protection. Dig Dis Sci. 2005;50(Suppl 1):S16–23.
Brzozowski T, Konturek PC, Sliwowski Z, Kwiecień S, Drozdowicz D, Pawlik M, et al. Interaction of nonsteroidal anti-inflammatory drugs (NSAID) with Helicobacter pylori in the stomach of humans and experimental animals. J Physiol Pharmacol. 2006;57(Suppl 3):67–79.
Iwamoto J, Saito Y, Honda A, Matsuzaki Y. Clinical features of gastroduodenal injury associated with long-term low-dose aspirin therapy. World J Gastroenterol. 2013;19(11):1673–82.
Venerito M, Treiber G, Wex T, Kuester D, Roessner A, Di Mario F, et al. Effects of low-dose aspirin on gastric erosions, cyclooxygenase expression and mucosal prostaglandin-E2 do not depend on Helicobacter pylori infection. Aliment Pharmacol Ther. 2006;23(8):1225–33.
Venerito M, Treiber G, Wex T, Kuester D, Roessner A, Mönkemüller K, et al. Short-term/low-dose aspirin-induced duodenal erosions are not dependent on Helicobacter pylori infection, cyclooxygenase expression and prostaglandin E2 levels. Scand J Gastroenterol. 2008;43(7):801–9.
Wang RQ, Xu SC. Changes of endogastric pH in 24 hours in patients with duodenal ulcer. Henan J Diagn Ther. 2002;16:249–50.
ASGE Standards of Practice Committee, Early DS, Ben-Menachem T, et al. Appropriate use of GI endoscopy. Gastrointest Endosc. 2012;75(6):1127–31.
Nakanishi T, Tamai I. Interaction of drug or food with drug transporters in intestine and liver. Curr Drug Metab. 2015;16:753–64.
Xu CH, Cheng G, Liu Y, Tian Y, Yan J, Zou MJ. Effect of the timing of food intake on the absorption and bioavailability of carbamazepine immediate-release tablets in beagle dogs. Biopharm Drug Dispos. 2012;33:30–8.
Ying XL. Oral administration of enteric-coated tablets of aspirin are two days comparison gastric responses. Chin Med Mod Distance Educ China. 2010;9:230.
Lian XF, Xiang DC. Influence of administration time of enteric-coated tablets of aspirin on gastric adverse effects. Chin J Coal Ind Med. 2005;8:457–8.
Maree AO, Curtin RJ, Dooley M, Conroy RM, Crean P, Cox D, et al. Platelet response to low-dose enteric-coated aspirin in patients with stable cardiovascular disease. J Am Coll Cardiol. 2005;46:1258–63.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Weijun Guo, Wenlin Lu, Yujun Xu, Liansheng Wang, Qin Wei and Qingyun Zhao have no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee at Huaiyin Hospital (Number HYYY201207080) and the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Written informed consent was obtained from all patients prior to their enrollment in the study.
Funding
This study was funded by grants from the Huaiyin Hospital.
Rights and permissions
About this article
Cite this article
Guo, W., Lu, W., Xu, Y. et al. Relationship between Adverse Gastric Reactions and the Timing of Enteric-Coated Aspirin Administration. Clin Drug Investig 37, 187–193 (2017). https://doi.org/10.1007/s40261-016-0474-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-016-0474-z