Abstract
Background and Objective
Effective treatment of postoperative pain contributes to decreasing the rate of complications as well as the total cost of the operated patients. The aim of this study was to analyze the costs and the efficiency of use of continuous infusion of levobupivacaine 0.5 % with the help of an infusion pump in modified radical mastectomy.
Methods
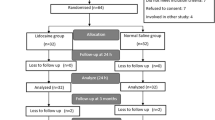
A cost calculation of the analgesic procedures (continuous infusion of levobupivacaine 0.5 % [levobupivacaine group (LG)] or saline [saline group (SG)] (2 ml/h 48 h) has been carried out based on the data of a previous clinical trial (double-blind randomized study) of patients who underwent modified radical mastectomy surgery. The measure of the effectiveness was the point reduction of pain derived from the verbal numeric rating scale (VNRS). The usual incremental cost-effectiveness ratio (ICER) was performed.
Results
Considering only the intravenous analgesia, overall costs were lower in LG, as less analgesia was used (EUR14.06 ± 7.89 vs. 27.47 ± 14.79; p < 0.001). In this study the costs of the infusion pump were not calculated as it was used by both groups and they offset each other. However, if the infusion pump costs were included, costs would be higher in the LG, (EUR91.89 ± 7.89 vs. 27.47 ± 14.79; p < 0.001) and then the ICER was −8.51, meaning that for every extra point of decrease in the pain verbal numerical rating score over the 2-day period, the cost increased by EUR8.51.
Conclusion
Infiltration of local anesthetics is an effective technique for controlling postoperative pain and the associated added costs are relatively low in relation to the total cost of mastectomy, therefore providing patients with a higher quality of care in the prevention of pain.
Clinical trials registration: clinicaltrials.gov: reference number NCT01389934. http://clinicaltrials.gov/show/NCT01389934.
Similar content being viewed by others
References
American Cancer Society. Cancer facts & figures 2015. GA: Atlanta; 2015.
Neira F, Ortega JL. Prevalencia del dolor agudo. In: Torres LM, Collado F, editors. Manejo práctico del dolor agudo. Madrid: Ergon; 2008. p. 1–40.
Ilfeld BM, Morey TE, Enneking FK. Portable infusion pumps used for continuous regional analgesia: delivery rate accuracy and consistency. Reg Anesth Pain Med. 2003;28:424–32.
Ilfeld BM, Morey TE, Enneking FK. Delivery rate accuracy of portable, bolus-capable infusion pumps used for patient-controlled continuous regional analgesia. Reg Anesth Pain Med. 2003;28:17–23.
Pacik PT, Werner C, Jackson N, Lobsitz C. Pain control in augmentation mammaplasty: the use of indwelling catheters in 200 consecutive patients. Plast Reconstr Surg. 2003;111:2090–6.
Baroody M, Tameo MN, Dabb RW. Efficacy of the pain pump catheter in immediate autologous breast reconstruction. Plast Reconstr Surg. 2004;114:895–8.
Givens VA, Lipscomb GH, Meyer NL. A randomized trial of postoperative wound irrigation with local anesthetic for pain after cesarean delivery. Am J Obstet Gynecol. 2002;186:1188–91.
Fustran N, Dalmau A, Sabaté A. Analgesia postoperatoria mediante infusión continua de anestésico local en la incisión quirúrgica tras cirugía abdominal. Revisión sistemática de la bibliografía. Rev Esp Anes. 2011;58:343–4.
Baig MK, Zmora O, Derdemezi J, Weiss EG, Nogueras JJ, Wexner SD. Use of the ON-Q pain management system is associated with decreased postoperative analgesic requirement: double blind randomized placebo pilot study. J Am Coll Surg. 2006;202:297–305.
Beaussier M, El’Ayoubi H, Schiffer E, et al. Continuous preperitoneal infusion of ropivacaine provides effective analgesia and accelerates recovery after colorectal surgery: a randomized, double-blind, placebo-controlled study. Anesthesiology. 2007;107:461–8.
Polglase AL, McMurrick PJ, Simpson PJ, et al. Continuous wound infusion of local anesthetic for the control of pain after elective abdominal colorectal surgery. Dis Colon Rectum. 2007;50:2158–67.
Forastiere E, Sofra M, Giannarelli D, Fabrizi L, Simone G. Effectiveness of continuous wound infusion of 0.5% ropivacaine by On-Q pain relief system for postoperative pain management after open nephrectomy. Br J Anaesth. 2008;101:841–7.
Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound catheters delivering local anesthetic for postoperative analgesia: a quantitative and qualitative systematic review of randomized controlled trials. J Am Coll Surg. 2006;6:914–32.
Ferreira Laso L, Lopez-Picado A, Lamata L, Ceballos Garcia M, Ibañez López C, Pipaon Ruilope L, Lamata Hernandez F, Antoñanzas Villar F, Valero Martinez C, Aizpuru F, Hernanz Chaves R. Postoperative analgesia by infusion of local anesthetic into the surgical wound after modified radical mastectomy: a randomized clinical trial. Plast Reconstr Surg. 2014;134(6):862e–70e. doi:10.1097/PRS.0000000000000762
Ribera H, Esteve N, Garrido JP. La transición de dolor agudo postoperatorio a crónico: ¿Qué sabemos? Rev Soc Esp Dolor. 2012;19(4):197–208.
Wallace MS, Wallace AM, Lee J, Dobke MK. Pain after breast surgery: a survey of 282 women. Pain. 1996;66(2–3):195–205.
Miaskowski C, Cleary J, Burney R, Coyne P, Finley R, Foster R, et al. Guideline for the management of cancer pain in adults and children, vol. 3. Glenview (IL): American Pain Society (APS); 2005. p. 166.
Morrison JE Jr, Jacobs VR. Reduction or elimination of postoperative pain medication after mastectomy through use of a temporarily placed local anesthetic pump vs. control group. Zentralbl Gynakol. 2003;125(1):17–22.
Legeby M, Jurell G, Beausang-Linder M, Olofsson C. Placebo-controlled trial of local anaesthesia for treatment of pain after breast reconstruction. Scand J Plast Reconstr Surg Hand Surg. 2009;43(6):315–9.
Heller L, Kowalski AM, Wei C, Butler CE. Prospective, randomized, double-blind trial of local anesthetic infusion and intravenous narcotic patient-controlled anesthesia pump for pain management after free TRAM flap breast reconstruction. Plast Reconstr Surg. 2008;122:1010–8.
Turan Z, Sandelin K. Local infiltration of anaesthesia with subpectoral indwelling catheters after immediate breast reconstruction with implants: a pilot study. Scand J Plast Reconstr Surg Hand Surg. 2006;40:136–9.
Losken A, Parris JJ, Douglas TD, Corner MA. Use of the infusion pain pump following transverse rectus abdominis muscle flap breast reconstruction. Ann Plast Surg. 2005;54:479–82.
Hernández Garcia D, Lara Vila I, Caba Barrientos F, Ramos Curado P, Núñez García A, Echevarría Moreno M. Análisis coste-efectividad de la PCA postoperatoria frente a la infusión continua elastomérica de tramadol y metamizol. Rev Esp Anes. 2007;54:213–20.
Gonado C, Leitgeb U, Sitzwohl C, Ihra G, Weinstal C, Kettner SC. Spinal versus general anesthesia for orthopedic surgery: anesthesia drug and supply costs. Anesth Analg. 2006;102(2):524–9.
Shuster M, Gottschalk A, Berger J, Standl T. A restrospective comparison of costs for regional and general anesthesia techniques. Anesth Analg. 2005;100(3):786–94.
Carreras Coderch L, Nieto Martin-Bejarano J, Saenz Cusi A, Coya Viña J, Martin Comin JM, Antoñanzas FJ, et al. Análisis coste-efectividad de samario-153 (Quadramet) en el tratamiento del dolor en pacientes con cáncer de próstata y metástasis óseas. Clin Transl Oncol. 2005;7:198–204.
Fodale V, Praticó C, Tescione M, Lucanto T, Tanania S, Santamaria LB. Comparative cost-analysis of a propofol-cisatracurium-based anesthesia with remifentanil or fentanyl for laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2005;15:149–52.
Beers RA, Calimlim JR, Uddoh E, Esposito BF, Camporesi EM. A comparison of the cost-effectiveness of remifentanil versus fentanyl as an adjuvant to general anesthesia for outpatient gynecologic surgery. Anesth Analg. 2000;91:1420–5.
Mahabir RC, Peterson BD, Williamson JS, Valnicek SM, Williamson DG, East WE. Locally administered ketorolac and bupivacaine for control of postoperative pain in breast augmentation patients. Plast Reconstr Surg. 2004;114(7):1910–6.
Ranta PO, Ala-Kokko TI, Kukkonen JE, Ohtonen PP, Raudaskoski TH, Reponen PK, Rawal N. Incisional and epidural analgesia after caesarean delivery: a prospective, placebo-controlled, randomised clinical study. Int J Obstet Anesth. 2006;15(3):189–94.
Prithvi Raj P, Abrams BM, Benzon HT, Hahn MB, Heavner JE, Niv D. Tratamiento práctico del dolor. Economia sanitaria. Madrid: Harcourt; 2002. p. 929–33.
Wong GY, Schroeder DR, Carns PE, et al. Effect of neurolytic celiac plexus block on pain relief, quality of life, and survival in patients with unresectable pancreatic cancer: a randomized controlled trial. JAMA. 2004;291(9):1092–9.
Patrick DL, Deyo RA, Atlas SJ, Singer DE, Chapin A, Keller RB. Assessing health-related quality of life in patients with sciatica. Spine. 1995;20(17):1899–908.
Carli F, Mayo N, Klubien K, Schricker T, Trudel J, Belliveau P. Epidural analgesia enhances functional exercise capacity and health-related quality of life after colonic surgery: results of a randomized trial. Anesthesiology. 2002;97(3):540–9.
Ikenberg R, Hertel N, Andrew Moore R, et al. Cost-effectiveness of tapentadol prolonged release compared with oxycodone controlled release in the UK in patients with severe non-malignant chronic pain who failed 1st line treatment with morphine. J Med Econ. 2012;15(4):724–36.
Díez F, Marcos JM, Baticón PM, Montes A, Bermejo JC, Merino M. Concordancia entre la escala verbal numérica y la escala visual analógica en el seguimiento del dolor agudo postoperatorio. Rev Esp Anestesiol Reanim. 2001;58:279–82.
Coluzzi F, Ruggeri M. Clinical and economic evaluation of tapentadol extended release and oxycodone/naloxone extended release in comparison with controlled release oxycodone in musculoskeletal pain. Curr Med Res Opin. 2014;30(6):1139–51.
Dunlop W, Uhl R, Khan I, Taylor A, Barton G. Quality of life benefits and cost impact of prolonged release oxycodone/naloxone versus prolonged release oxycodone in patients with moderate to severe non-malignant pain and opioid-induced constipation: a UK cost-utility analysis. J Med Econ. 2012;15:564–75.
Frei A, Andersen S, Hole P, Jensen N. A one year health economic model comparing transdermal fentanyl with sustained-release morphine in the treatment of chronic non cancer pain. J Pain Palliat Care Pharmacother. 2003;17(2):5–26.
Primer on Cost-Effectiveness Analysis. http://www.acponline.org/clinical_information/journals_publications/ecp/sepoct00/primer.htm. Accessed on 24 Nov 2011.
Schell SR. Patient analgesia alter axillary lymph node dissection (ALND): outcomes in pain management using long-term continuous local anesthesia delivery. J Surg Res. 2003;114(2):243–4.
Lu L, Fine NA. The efficacy of continuous local anesthetic infiltration in breast surgery: reduction mammaplasty and reconstruction. Plast Reconstr Surg. 2005;115(7):1927–34.
Talbot H, Hutchinson SP, Edbrooke DL, Wrench I, Kohlhardt SR. Evaluation of a local anaesthesia regimen following mastectomy. Anaesthesia. 2004;59(7):664–7.
Holmgren RT, Tarpila E. Intermittent injection of bupivacaine into the margin or the cavity after reduction mammaplasty. J Plast Surg Hand Surg. 2005;39(4):218–21.
Sidiropoulou T, Bounomo O, Fabbi E, Silvi MB, Kostopanagiotou G, Sabato AF, et al. A prospective comparison of continuous wound infiltration with ropivacaine versus single-injection paravertebral block after modified radical mastectomy. Anesth Analg. 2008;106(3):997–1001.
Pacik PT, Nelson CE, Werner C. Pain control in augmentation mammaplasty: safety and efficacy of indwelling catheters in 644 consecutive patients. Aesthet Surg J. 2008;28(3):279–284. doi:10.1016/j.asj.2008.02.001
Rawal N, Gupta A, Helsing M, Grell K, Allvin R. Pain relief following breast augmentation surgery: a comparison between incisional patient-controlled regional analgesia and traditional oral analgesia. Eur J Anaesthesiol. 2006;23(12):1010–7.
Dagtekin O, Hotz A, Kampe S, Auweiler M, Warm M. Postoperative analgesia and flap perfusion after pedicled TRAM flap reconstruction—continuous wound instillation with ropivacaine 0.2%. A pilot study. J Plast Reconstr Aesthet Surg. 2009;62(5):618–25.
Acknowledgments
We thank the Departments of Anesthesiology and Gynecology, the Pharmacy and the Research Unit of Txagorritxu Hospital for their help in this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest to declare.
Funding
No external funding was received for this study.
Rights and permissions
About this article
Cite this article
Ferreira Laso, L., López Picado, A., Antoñanzas Villar, F. et al. Cost-Effectiveness Analysis of Levobupivacaine 0.5 %, a Local Anesthetic, Infusion in the Surgical Wound After Modified Radical Mastectomy. Clin Drug Investig 35, 575–582 (2015). https://doi.org/10.1007/s40261-015-0316-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-015-0316-4