Abstract
The Spectra Optia® automated apheresis system, indicated for red blood cell exchange in people with sickle cell disease, underwent evaluation by the National Institute for Health and Care Excellence, which uses its Medical Technologies Advisory Committee to make recommendations. The company (Terumo Medical Corporation) produced a submission making a case for adoption of its technology, which was critiqued by the Newcastle and York external assessment centre. Thirty retrospective observational studies were identified in their clinical submission. The external assessment centre considered these were of low methodological and reporting quality. Most were single-armed studies, with only six studies providing comparative data. The available data showed that, compared with manual red blood cell exchange, Spectra Optia reduces the frequency of exchange procedures as well as their duration, but increases the requirement for donor blood. However, other clinical and patient benefits were equivocal because of an absence of robust clinical evidence. The company provided a de novo model to support the economic proposition of the technology, and reported that in most scenarios Spectra Optia was cost saving, primarily through reduced requirement of chelation therapy to manage iron overload. The external assessment centre considered that although the cost-saving potential of Spectra Optia was plausible, the model and its clinical inputs were not sufficiently robust to demonstrate this. However, taking the evidence together with expert and patient advice, the Medical Technologies Advisory Committee considered Spectra Optia was likely to save costs, provide important patient benefits, and reduce inequality, and gave the technology a positive recommendation in Medical Technology Guidance 28.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The Spectra Optia® apheresis system provides automated red blood cell exchange for people with chronic symptomatic sickle cell disease. It is operationally more efficient than manual red blood cell exchange, resulting in improved clinical and patient outcomes and improved regulation of iron levels. |
The paucity of clinical evidence to support the Spectra Optia system largely reflects a lack of clinical equipoise. Limited observational evidence and expert opinion suggest the system provides long-term savings to the National Health Service, primarily through a reduction in the requirement for iron chelation therapy. |
With the correct service provision, the Spectra Optia system could also reduce geographical inequalities in the management of sickle cell disease. |
1 Introduction
The National Institute for Health and Care Excellence (NICE) provides evidence-based guidance for the National Health Service (NHS) in England and Wales with the aim of improving clinical outcomes for patients as well as delivering optimal use of finite NHS resources. The NICE Medical Technologies Evaluation Programme (MTEP) was established in 2009 and, together with the independent Medical Technologies Advisory Committee (MTAC), is responsible for the evaluation of medical technologies (interventions or diagnostics) for use within the NHS [1].
To be selected for evaluation, a technology must hold a current CE (conformité Européenne) mark or be expected to gain one within 12 months, and must be considered by the MTAC to have ‘plausible promise’ [2]. To be recommended for adoption, a technology must demonstrate equivalent benefit to patients at lower cost to the NHS, or greater benefit with equivalent costs. Once selected by the MTAC and assessment is commenced, the medical technology will usually undergo a relatively rapid guidance development process of 38 weeks. It is the responsibility of the company (that is, the manufacturer or UK distributor of the technology) to produce a submission whereby the claimed benefits of the technology to the patient and/or NHS must be demonstrated. The company’s submission is evaluated by an external assessment centre (EAC), which has the responsibility of critically assessing the clinical and cost evidence in the company’s submission, and its relevance to the decision problem defined in the evaluation scope. Finally, recommendations for adoption are made by the MTAC, who consider the evidence presented by the company and the EAC, with assistance from clinical experts and, sometimes, patient representatives. This process is facilitated from start to finish by the MTEP [3].
The Spectra Optia® automated apheresis system, manufactured and supplied by Terumo Medical Corporation, was granted a CE mark as a class IIb medical device in May 2014. It has several applications relating to the in situ separation of blood components, including automated red blood cell (RBC) exchange or depletion exchange in adults or children with sickle cell disease. Following selection of the technology in April 2015, assessment began in June 2015, with the clinical and economic evaluation conducted by the Newcastle and York EAC (Newcastle upon Tyne Hospitals NHS Foundation Trust and York Health Economics Consortium partnership). In March 2016, NICE issued final guidance on “Spectra Optia for automated RBC exchange in patients with sickle cell disease”. Full documentation of the process, supporting evidence and the final guidance is available on the NICE website [4], including the company submission [5], and the EAC’s assessment report [6]. This article provides an overview of the company’s submission of evidence, the EAC’s critique of the evidence, and the formulation of final guidance. It is one of a series of NICE Medical Technology Guidance (MTG) summaries being published in Applied Health Economics and Health Policy.
2 Background to the Condition and Technology
Sickle cell disease is a group of recessive genetic blood disorders in people who have inherited two copies of a mutated gene for haemoglobin production. The most common variant of the disease, occurring when two copies of the sickle cell gene are present (HbSS), is sickle cell anaemia, although other significant variants also occur, such as β-thalassaemia [7]. Sickle cell disease manifests as an abnormality in the haemoglobin molecule, which causes the RBCs to become rigid and deform into the eponymous sickle-like shape, with two important consequences. First, sickled cells undergo haemolysis, resulting in them having a much shorter half-life than normal RBCs (typically 10–20 days compared with 90–120 days), which can lead to severe and life-threatening anaemia. Second, the sickled deformity causes damage to blood vessels. Large vessel damage is caused by repeated endothelial damage by adherent sickle cells, complicated by vasoconstriction and nitric oxide deficiency, and leads to complications such as stroke, acute chest syndrome, and priapism. Small vessel occlusion is caused directly by sickled cells and is associated with acute episodes such as a painful crisis or more chronic damage such as avascular necrosis of the hips and renal failure. An additional complication of sickle cell disease is growth impairment in children [7].
An example of a clinical pathway for the management of sickle cell disease is summarised in Fig. 1. For most people, the first-line treatment for chronic, symptomatic sickle cell disease is the anti-neoplastic drug hydroxycarbamide, which stimulates the production of foetal haemoglobin in the blood (which does not cause sickle formation). However, approximately 25% of patients are unable or unwilling to take hydroxycarbamide (because of contraindications or because they cannot tolerate it) or remain refractory to treatment. Pregnant or breastfeeding women, or people of both sexes planning to conceive, should not take hydroxycarbamide [8]. Additionally, hydroxycarbamide is not indicated as a preventative measure in patients who are at a very high risk of stroke.
For patients in whom hydroxycarbamide is not suitable, or for patients requiring primary or secondary prevention of stroke, an elective blood transfusion may be indicated. Options include simple top-up transfusion, RBC manual exchange transfusion, and automated RBC exchange transfusion. The initial choice of transfusion therapy depends on a range of factors dependent on clinical status and, in practice, local facilities.
A top-up transfusion consists of the simple transfusion of donor blood into the recipient. In general, top-up transfusions are suitable if the main purpose of treatment is to manage anaemia, and the introduction of transfusions does not pose an unacceptable increase in the risk of vaso-occlusive events, such as stroke. However, top-up transfusions are ‘iron positive’, and are associated with an unavoidable accumulation of iron in the body. Iron overload, which is characterised by an attendant increase in serum ferritin, can cause serious complications such as liver cirrhosis, heart failure, and diabetes mellitus [9]. Thus, the use of top-up transfusions will inevitably require iron chelation therapy, typically after around 20 transfusions. Iron chelation therapy is often poorly tolerated by patients, has consequent issues with non-compliance, and is expensive.
The alternative to simple top-up transfusion is RBC exchange transfusion in which blood is removed through venesection and replaced with an equal volume of donor blood. Manual exchange is the simplest method, and has the advantage of being versatile by virtue of not requiring specialist technology to be implemented [10]. In automated RBC exchange, an apheresis machine removes patient blood and extracts the RBCs through centrifugation. The non-RBC component of the blood (principally plasma and white cells), supplemented with packed donor RBC units (or, in the case of depletion exchange, an isomolar solution such as normal saline), is simultaneously returned to the patient through a second line. Both manual and automated RBC exchanges are considered to be ‘iron neutral’ because packed RBCs are used to replace the patient’s blood in an isovolaemic manner. However, in practice, owing to technical and practical limitations, manual exchange tends to lead to iron accumulation and its associated complications. In contrast, automated RBC exchange is thought to be truly iron neutral and its use is believed to avoid the need for chelation therapy [11].
The Spectra Optia device is an automated apheresis system that is indicated for the elective treatment of sickle cell disease (as well as for other indications such as plasma exchange and stem cell harvesting). In their submission to NICE, the claimed benefits for patients made by the company were as follows: reduced frequency of exchange; reduced duration of exchange; reduced iron overload, meaning a reduction or possible cessation of chelation therapy; and better compliance and efficiency resulting in improved clinical outcomes, such as a reduced incidence of stroke, painful crises, acute chest syndrome, improved outcomes following surgery, improved growth in children, and improved quality of life. Claimed benefits for the healthcare system were a reduction in the requirement for iron chelation therapy; reduced staff and staff grade; reduced complications (and consequent reduction in hospital admissions); and improved use of donor blood (through the depletion-exchange protocol) [12].
3 Decision Problem (Scope)
In their submission to NICE for assessment, companies are required to define and adhere to a decision problem, which is described in PICO (population, intervention, comparator, outcomes) terms and is consistent with the published scope of the MTG [12]. The EAC uses this as a reference during its critique of the submission.
3.1 Population
The population described by the company in the decision problem was “Sickle cell disease patients requiring a medium or long-term transfusion regime”. It was noted by the EAC that this represented a subtle, but important change from the scope that specified the requirement for exchange transfusion regime (see Sect. 3.3) [12]. The EAC also considered that the proposed addition of management of acute complications of sickle cell disease, which is the subject of a NICE clinical guideline [13], was outside the scope.
3.2 Intervention
The intervention in the MTEP scope was the “Spectra Optia apheresis device” [12]. In the decision problem, the company had modified this to include the “Cobe Spectra apheresis device”, the predecessor technology to the Spectra Optia device, to increase the size of the evaluable evidence base, as there was a paucity of evidence published on the Spectra Optia device itself. The company stated that the Spectra Optia and Cobe Spectra were “essentially equivalent devices”, and reported three head-to-head clinical studies to support this assertion [14–16]. However, following discussion with company representatives and clinical experts, the EAC was satisfied that the Spectra Optia system was likely to be technically equivalent, or superior to, the Cobe Spectra system. This was because the Spectra Optia system represents an incremental improvement, rather than a fundamental change, over the older Cobe Spectra system. The additional functionality built into the system has the potential to improve safety, operator performance, and patient experience, and has implications for resource use, but should not negatively impact on the system’s efficacy compared with the Cobe Spectra system. Therefore, the EAC considered that it was reasonable to generalise evidence reported on the Cobe Spectra system to the Spectra Optia system.
3.3 Comparator
The comparator listed in the scope was “Manual red blood cell exchange” [12]. In their statement of the decision problem, the company proposed “Simple or ‘top up’ transfusions” as an additional comparator. This was justified by the company on the basis that the use of top-up transfusions reflects current NHS practice. Whilst recognising the reality that administering top-up transfusions (usually combined with iron chelation therapy) was a strategy that was practised in some NHS regions, the EAC disagreed that was a satisfactory reason to consider it as a valid comparator. This was because a top-up transfusion is mechanistically different to exchange transfusion and is known to be a suboptimal option for most patients, as although it effectively treats anaemia, it is less effective at preventing vaso-occlusive complications as it increases blood viscosity [7, 17]. Top-up transfusions have different indications and contraindications and different targets compared with exchange transfusions and are relatively contraindicated where iron overload is liable to be problematic [17] (which is inevitable when frequent elective top-up transfusions are performed).
3.4 Outcomes
The company’s reporting of the outcomes of the decision problem matched the scope [12], with the proposal of alloimmunisation as an additional safety outcome, which the EAC agreed should be considered. The outcomes specified in the scope were categorised as primary or secondary, and consisted of a mixture of intermediate, clinical, patient benefit, adverse events, and resource use endpoints.
One outcome, the proportion of total haemoglobin that is sickled (HbS%), is an intermediate or surrogate measure of disease severity and risk of vaso-occlusive complications, which fluctuates during treatment cycles. Usually, the target HbS% should be kept under 30% [7]. Patient haematocrit (an indicator for anaemia and target during RBC exchange transfusion), iron overload, and the associated need for chelation therapy were also listed as endpoints, although the latter was not clearly defined.
“Clinical outcomes including frequency of stroke, multi-organ failure, acute chest syndrome and pain crises” was the main clinical endpoint listed, with body mass index and growth in children listed as secondary outcomes. Quality of life was the only outcome directly related to patient benefit. Several resource use outcomes were included in the decision problem, including duration of exchange procedure; frequency of treatment; length of hospital stay; and staff time and staff group/grade.
The company identified published evidence on most of these outcomes with the exception of staff time and staff group/grade, quality of life, and body mass index and growth in children, and, importantly, clinical outcomes. The company did not attempt to extrapolate intermediate endpoints to clinical outcomes.
4 Review of Clinical Effectiveness Evidence
4.1 Company’s Review of Clinical Effectiveness Evidence
The company performed a literature search and sift using inclusion and exclusion criteria consistent with the original scope [12]. Additional studies were found by searching proceedings of annual conferences known to be relevant. Studies were also included that compared RBC exchange with top-up transfusions; the searching methodology of these studies was not described causing the potential for bias. In total, 30 studies were reported in the company submission.
Six studies compared the Spectra Optia system, or its predecessor the Cobe Spectra system, with manual RBC exchange [18–23]. These were all retrospective observational studies that did not use an experimental comparative design; three used historical controls [18, 21, 23], one was a before-and-after study [19] and two were between-centres studies [20, 22]. Only two of the studies were peer reviewed [18, 20], one was a published letter [22], and three were reported as conference abstracts [19, 21, 23].
Of the other 24 studies, 14 were single-armed studies that reported absolute or ‘before and after data’, with seven published as full peer-reviewed studies [24–30] and seven as conference abstracts [31–37]. Two were single-armed studies on manual exchange, both published as conference abstracts [38, 39]. Three studies compared technical aspects of the Spectra Optia and Cobe Spectra systems [14–16], and four studies compared automated RBC exchange with top-up transfusions [40–43]. One study was in pregnant women [44].
The company interpreted the clinical evidence as demonstrating that Spectra Optia resulted in shorter procedure times, longer intervals between procedures, and an increased use of packed RBCs compared with manual exchange. In addition, it reported that automated RBC exchange was superior to manual RBC exchange at reducing ferritin levels, and that there was general equivalence with regard to the physiological parameters of HbS% and haematocrit.
4.2 EAC Critique of Clinical Effectiveness Evidence
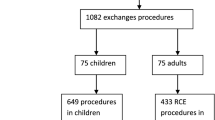
The EAC reproduced the company’s bibliographic database searches, using the details as reported in the submission. Searches were not carried out for the company search activities where insufficient information was provided to enable replication. As far as possible, the bibliographic database searches were replicated exactly as reported. The EAC also conducted its own searches to retrieve any studies that might have been missed by the company’s search strategies, and sifted these according to the scope. Results were reported using PRISMA methodology (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) [45] (Fig. 2). This identified four additional studies [46–49], but these were conference abstracts that did not help in answering the decision problem. Thus, the EAC was confident that all relevant studies were included in the submission of clinical evidence.
In the opinion of the EAC, the company critically appraised the identified studies fairly and presented the results in a tabular format. However, although the company described many of the limitations of individual studies, it did not fully describe how this uncertainty might affect confidence in the overall results. The company was correct in not attempting data synthesis (meta-analysis) owing to the heterogeneous nature of the studies; instead it presented the results of each study in a tabular format and matched individual study results against the outcomes and benefits listed in the scope [12]. The company combined results from single-armed and comparative studies in its interpretation, which led to a greater volume of data on the intervention (automated RBC exchange) compared with the comparator (manual RBC exchange).
The majority of the evidence was from retrospective observational studies, which were subject to potential confounding, selection bias and reporting bias. Most of the studies were single armed and not designed to directly compare the intervention with the comparator, and the heterogeneous nature of the studies did not allow for meaningful data synthesis. The EAC noted that the quality of reporting was often poor. Only a minority of the studies were reported as full articles in peer-reviewed journals [18, 20, 24, 26–29, 35, 44]. Details of the other unpublished studies can be found in the EAC’s assessment report [6].
The EAC focussed on results from the six comparative studies with manual RBC exchange [18–23] because these provided the most useful data relevant to the decision problem, and the peer-reviewed single-armed studies of the Spectra Optia [28] and Cobe Spectra systems [24, 26, 27, 29, 30], as these studies were fully reported and provided useful supporting data. Details of these studies are summarised in Table 1.
The EAC considered that these studies provided strong evidence that, compared with manual RBC exchange, the Spectra Optia system was associated with a shorter duration of procedure (about half the time), a reduced frequency of treatments (2–3 weeks greater treatment interval), and with an increased use of packed RBCs (approximately double for Spectra Optia). The EAC considered that the evidence on achieving HbS% and haematocrit targets was equivocal, that is, the studies did not show that Spectra Optia was different compared with manual RBC exchange for these outcomes. The EAC considered that, whilst the studies indicated that automated RBC exchange was associated with a decrease or stabilisation in serum ferritin levels compared with manual RBC exchange, this effect had not been demonstrated statistically and the overall implication on iron overload and the chelation therapy requirement remained uncertain. There was no comparative evidence reported on hospital admissions. There was no meaningful comparative evidence reported on staff resources, ease of venous access, quality of life, and body mass index growth in children. Finally, there was no evidence presented to support the comparative benefit of the Spectra Optia system on clinical and complication outcomes, such as stroke, painful crises, and acute chest syndrome, and no studies provided results according to iron overload status. A summary of how the results from the identified clinical evidence addressed the outcomes specified in the decision problem and the claimed benefits is reported in Table 2.
Owing to the lack of high- or moderate-quality observational evidence on key outcomes reported in the published literature, the EAC communicated extensively with clinical experts who were experienced with the use of exchange transfusions. The EAC received qualitative feedback from six of eight clinical experts approached, who provided valuable information on the relative advantages and disadvantages of the transfusion methods under assessment. The experts were consistent in their opinions that automated RBC exchange is more effective than manual RBC exchange in reducing or maintaining ferritin levels, and had the potential to avoid the need for initiating, or allow for the cessation of, iron chelation therapy. When questioned why there was a lack of good-quality prospective studies published to compare the efficacy and safety of automated compared with manual RBC exchange, the experts cited the relative rarity of the disease (especially the subset of severe disease requiring chronic exchange transfusion), the lack of competitor products, and a general lack of funding from industry and charities to fund experimental studies as reasons. The experts were unanimous that future prospective experimental studies are unlikely because of issues with clinical equipoise; that is, it would be unethical to conduct trials as there is no clinical doubt that automated RBC exchange is at least as effective as manual RBC exchange, but it also offers clear additional patient benefits. The full communication log with the clinical experts is published during public consultation, along with all of the relevant evidence supporting the committee’s provisional recommendations [50].
5 Economic Evidence
5.1 Company’s Economic Submission
The company identified seven studies using the Cobe Spectra or Spectra Optia systems that included economic information [19, 26, 27, 29, 38, 40, 41]. However, these studies were deemed by the company to be unhelpful because they were poorly reported and were not robust; therefore, they were not considered further.
The company developed a de novo economic model to estimate the procedural and clinical costs associated with 5 years management of chronic, severe sickle cell disease using automated RBC exchange (the Spectra Optia system), manual RBC exchange, or top-up transfusions. The model described 12 scenarios with starting populations with different baseline characteristics (adults, children requiring secondary prevention of stroke, or children requiring primary prevention of stroke) and iron overload severities (none, mild, moderate, or severe). As the relative proportions of each population subgroup were not reported, this meant that an overall ‘average’ cost of management per person with sickle cell disease or overall budgetary impact was not calculated.
The company reported that, in the base case, Spectra Optia was always cost saving compared with manual RBC exchange, with savings ranging from £360 to £52,516 per patient over 5 years. In half of the scenarios (6/12), top-up transfusion was cost saving compared with automated RBC exchange (in adult or child patients with no or mild overload). Spectra Optia was associated with a greater requirement for packed RBC units than its comparators. For top-up transfusions, chelation therapy was the most important cost. Manual RBC exchange was associated with both relatively high procedural costs (through staffing requirements) and chelation therapy costs, and was therefore the most expensive option. The company conducted extensive univariate sensitivity analyses and threshold analyses on each scenario presented in the model. These were mainly based on adjusting healthcare resources and unit costs, and in general the results of the analyses favoured Spectra Optia.
5.2 Critique of Economic Evidence
The EAC agreed with the company that the seven identified studies in this assessment [19, 26, 27, 29, 38, 40, 41] were not of sufficient methodological quality or relevance to inform the decision problem. The EAC did not identify any further economic studies using its own literature search.
The EAC considered that the de novo model had several shortcomings. First, the model incorporated estimates of rates from clinical events which, in the opinion of the EAC, were not well supported by the evidence identified from the clinical literature. Second, capital costs and maintenance costs of the Spectra Optia device were not included in the base-case results. Third, the inclusion of 12 subgroups, which were not defined in the literature or recognised by clinical experts, required the company to make assumptions on how the modalities would perform without clinical evidence at that level of granularity. The EAC considered the sensitivity analyses performed by the company were of limited value because they did not challenge the underlying assumptions of the model or address its limitations.
The EAC undertook an additional economic analysis using the company’s model but adding the costs of the technology, as well as including revised figures for key resource use (primarily iron chelation therapy costs). The analysis suggested that, compared with manual RBC exchange, the Spectra Optia system was likely to be cost saving in patients with no or mild iron overload, but cost incurring in patients with moderate or severe iron overload (see Table 3). This analysis was subject to the same uncertainties as the company’s model.
In the opinion of the EAC, the cost-saving potential of the Spectra Optia system, compared with manual exchange, had not been demonstrated with confidence by the company’s model. However, following correspondence with clinical experts, the EAC considered that the Spectra Optia system had several economic benefits which, taken as whole, may be resource saving for the NHS. These included reduced procedure times and intervals between procedures; reduced need for chelation therapy to manage iron overload; reduced variability in clinical practice, helping to standardise local and national level practice; and improved safety and auditing of exchange procedures. Additionally, the initial capital cost of the Spectra Optia system could be offset by its use in other indications such as plasma exchange apheresis and stem cell harvesting.
6 NICE Guidance
6.1 Provisional Recommendations and Consultation
In October 2015, the MTAC convened to make provisional MTG recommendations on the Spectra Optia system, with the assistance of the EAC, three clinical expert advisors, and a patient representative. The committee considered that the available evidence indicated that automated RBC exchange procedures are shorter and have a longer-lasting clinical benefit than manual exchange, meaning that patients need the procedure less often. However, the published clinical evidence base to support other benefits of the Spectra Optia system was generally poor and, in the absence of robust published data, the committee accepted the opinion of the experts that the Spectra Optia system was the only reliable iron neutral transfusion treatment available. This was because, in contrast to automated RBC exchange, manual RBC exchange in a typical hospital setting could not achieve the level of precision needed to achieve absolute iron neutrality. Furthermore, the use of chelation therapy to reduce iron overload is poorly tolerated by patients, which causes compliance issues, as well as being expensive.
The committee further discussed issues concerning NHS resources and costs. There is currently a lack of equity in service provision in the treatment of sickle cell disease, with people living outside large cities receiving suboptimal treatment or facing significant transport issues. The cause of provision inequity is related to the uneven geographical distribution of people with sickle cell disease (prevalence) and the consequent lack of availability of specialist expertise and equipment in peripheral centres. Moreover, current levels of NHS tariff remuneration are likely to act as a disincentive to providers to adopt automated RBC exchange.
Regarding costs, the MTAC recognised that the company’s economic model employed subgroups that were not defined in practice, and that many of the inputs into the economic model were based on unsubstantiated estimates rather than empirical data. The committee heard that top-up transfusions, whilst being recognised as a suboptimal regimen, were used in practice in centres that had poor sickle cell disease treatment provision and should be considered in the analysis. Overall, the committee considered that, despite the limitations of the clinical evidence and subsequent uncertainties this caused in the economic analysis, the Spectra Optia system was likely to result in cost savings for the NHS, especially when the technology was used additionally for other indications. These cost savings would mainly result from the reduced requirement of iron chelation therapy.
Following the meeting, draft guidance was produced and released for public consultation between 13 October and 10 November, 2015. In total, 48 comments were submitted by external stakeholders. These were individually addressed during the MTAC meeting held on 17 December, 2015. The comments were mainly related to small factual inaccuracies or a lack of clarity in the draft guidance and were addressed by the MTEP. No important changes to the draft recommendations were made following consultation.
6.2 Final NICE Guidance
In March 2016, NICE made the following recommendations concerning the use of the Spectra Optia system in the management of people with chronic sickle cell disease [4]:
-
1.1
The case for adopting Spectra Optia for automated RBC exchange in patients with sickle cell disease is supported by the evidence. Spectra Optia is faster to use and needs to be done less often than manual RBC exchange.
-
1.2
Spectra Optia should be considered for automated RBC exchange in patients with sickle cell disease who need regular transfusion.
-
1.3
NICE recommends collaborative data collection to generate further clinical evidence on some outcomes of treatment with Spectra Optia. In particular, there is a need for long-term data on how automated and manual exchanges affect iron overload status and the subsequent need for chelation therapy.
-
1.4
Based on current evidence and expert advice on the anticipated benefits of the technology when used in patients with iron overload, cost modelling shows that in most cases using Spectra Optia is cost saving compared with manual RBC exchange or top-up transfusion. The savings depend on the iron overload status of the patient, and are more likely to be achieved if devices already owned by the NHS can be used to treat sickle cell disease. The estimated cost saving for adopting Spectra Optia is £18,100 per patient per year, which has the potential to save the NHS in England £12.9 million each year.
Recommendation 1.4 was based on additional work performed by the NICE adoption and impact team [51].
7 Key Challenges and Learning Points
The Spectra Optia system ultimately received a positive recommendation in the published guidance (MTG 28) [4]. During its evaluation of the technology, the EAC faced several challenges, as did the MTAC during their deliberation of guidance recommendations. As is often observed with medical devices [52], there was a paucity of high-quality clinical evidence, particularly from comparative trials, for the EAC to assess the efficacy of Spectra Optia and for the company to provide support for its claims. An additional, and also familiar challenge, was the assessment of evidence on multiple versions of the device [52]. In the case of Spectra Optia, the absence of prospective comparative evidence could be ascribed to a lack of clinical equipoise, which also means that there is little prospect of a randomised controlled trial to directly address the decision problem. The EAC were therefore heavily reliant on the opinion of clinical experts to establish the efficacy of the device. However, although experts were able to provide qualitative evidence in support of Spectra Optia, they were unable to provide the quantitative evidence necessary to adequately inform the economic evidence, thus there remains a large degree of uncertainty concerning the cost-saving potential of the technology. This led the MTAC to recommend the future collection of data, particularly on iron overload status, to address this uncertainty [4].
Although it has been modelled that the Spectra Optia device would lead to cost savings for the NHS as a whole in the longer term (primarily through reduced iron chelation therapy requirements), there are barriers to implementation resulting from reimbursement that must be overcome for these to be realised. As the MTAC recognised, a potential problem is that, at present, the tariff reimbursement for plasma exchange is several times greater than it is for RBC exchange [53], which incentivises providers to use Spectra Optia for the former. Another barrier is that whilst hospital trusts would be required to provide the initial capital outlay for Spectra Optia, they would not directly recoup most this money from the expected reduction in iron overload, as chelation drugs are currently provided by clinical commissioning groups.
As acknowledged by the MTAC, currently, there is a high level of geographical inequity with the provision of automated RBC exchange, with services being absent outside of major cities, and patients from these areas having the prospect of suboptimal treatment or facing the inconvenience and cost of travelling to specialist centres elsewhere [54]. The Spectra Optia system may have the potential to standardise clinical practice at a national level. There may be the possibility that these patients could access Spectra Optia through a specialised care service such as one of six regional NHS Blood and Transplant Therapeutic Apheresis Services [55], and therefore it is possible these inequalities could be addressed through this or similar mechanisms.
8 Conclusion
Automated RBC exchange using the Spectra Optia system has been recommended by NICE for elective use in people with sickle cell disease in MTG 28. There is a lack of prospective comparative evidence of clinical efficacy and safety on Spectra Optia and currently the economic evidence to support cost savings is not robust. Prospective comparative research is not expected in the future owing to a lack of clinical equipoise. However, expert opinion, supported by limited observational data, is unanimous that the Spectra Optia system offers the potential to improve technical efficiency and thereby clinical endpoints, the most important of which is reducing or preventing iron overload. A reduced requirement for iron chelation therapy from automated RBC exchange should result in material cost savings to the NHS. Additionally, the widespread adoption of Spectra Optia could reduce current inequalities concerning the provision of treatment for sickle cell disease.
References
Campbell B. The NICE Medical Technologies Advisory Committee and medical technologies guidance. Heart. 2011;97(8):674–5.
Campbell B. How to judge the value of innovation. BMJ. 2012;344:e1457.
National Institute for Health and Clinical Excellence. Medical Technologies Evaluation Programme: Process Guide. London: National Institute for Health and Clinical Excellence; 2011.
National Institute for Health and Care Excellence. Spectra Optia for automated red blood cell exchange in patients with sickle cell disease. 2016. Available from: https://www.nice.org.uk/guidance/indevelopment/gid-mt271. Accessed 8 Apr 2016.
Cedar Healthcare Technology Research Centre. Spectra Optia apheresis system for automated red blood cell exchange in patients with sickle cell disease. 2015. Available from: https://www.nice.org.uk/guidance/MTG28/documents/submission-of-evidence-by-sponsor-4. Accessed 13 Apr 2016.
Willits I, Cole H, Arber M, et al. Spectra Optia apheresis system for automated red blood cell exchange in patients with sickle cell disease (assessment report). 2015. Available from: https://www.nice.org.uk/guidance/MTG28/documents/assessment-report. Accessed 13 Apr 2016.
Sickle Cell Society. Standards for the clinical care of adults with sickle cell disease in the UK. London. 2008. Available from http://sicklecellsociety.org/wp-content/uploads/2016/02/Standards-for-the-Clinical-Care-of-Adults-with-Sickle-Cell-Disease-in-the-UK.pdf. Accessed 14 Dec 2016.
Andemariam B, Browning SL. Current management of sickle cell disease in pregnancy. Clin Lab Med. 2013;33(2):293–310.
Porter JB. Practical management of iron overload. Br J Haematol. 2001;115(2):239–52.
Swerdlow PS. Red cell exchange in sickle cell disease. Hematol Am Soc Hematol Educ Program. 2006:48–53.
Porter J, Garbowski M. Consequences and management of iron overload in sickle cell disease. Hematol Am Soc Hematol Educ Program. 2013;2013:447–56.
National Instiute for Health and Clinical Excellence. Spectra Optia apheresis system for automated red blood cell exchange in patients with sickle cell disease: scoping document. 2015. Available from: https://www.nice.org.uk/guidance/MTG28/documents/final-scope. Accessed 12 Apr 2016.
National Institute for Health and Care Excellence. Sickle cell disease: managing acute painful episodes in hospital. 2012. Available from: https://www.nice.org.uk/guidance/cg143. Accessed 12 Apr 2016.
Perseghin P, Incontri A, Capra M. Erythrocyte-exchange in sickle-cell disease patients: a comparison between Caridian COBE Spectra and Optia cell separators. Transfus Apher Sci. 2013;48(2):177.
Poullin P, Sanderson F, Bernit E, Brun M. Red blood cell depletion/exchange procedure in patients with sickle cell disease: comparison between spectra Optia and COBE spectra separators. J Clin Apher. 2014;29(1):22.
Turhan FT, Karagun BS, Acipayam C, et al. Comparison of cobe spectra and spectra optia cell separators for red blood cell exchange in sickle cell disease patients. J Clin Apher. 2013;28(2):89–90.
Howell C, Douglas K, Cho G, et al. Guideline on the clinical use of apheresis procedures for the treatment of patients and collection of cellular therapy products: British Committee for Standards in Haematology. Transfus Med. 2015;25(2):57–78.
Cabibbo S, Fidone C, Garozzo G, et al. Chronic red blood cell exchange to prevent clinical complications in sickle cell disease. Transfus Apher Sci. 2005;32(3):315–21.
Dedeken L, Le PQ, Rozen L, et al. Clinical benefit and costs’ evaluation of erythocytapheresis compared to manual exchange transfusion for children with sickle cell disease: a single center experience. Blood. 2014;124(21):4091.
Duclos C, Merlin E, Paillard C, et al. Long-term red blood cell exchange in children with sickle cell disease: manual or automatic? Transfus Apher Sci. 2013;48(2):219–22.
Fasano R, Kaushal M, Leong T, et al. Efficacy of red cell exchange, partial manual exchange, and simple transfusion, concurrently with iron chelation therapy, in reducing iron overload in chronically transfused sickle cell patients. Pediatr Blood Cancer. 2015;62:23.
Kuo KH, Ward R, Kaya B, et al. A comparison of chronic manual and automated red blood cell exchange transfusion in sickle cell disease patients. Br J Haematol. 2015;170(3):425–8.
Woods D, Hayashi RJ, Fields ME, Hulbert ML. Chronic manual exchange transfusions compared with erythrocytapheresis in children and teens with sickle cell disease. Blood. 2014;124(21):4927.
Bavle A, Raj A, Kong M, Bertolone S. Impact of long-term erythrocytapheresis on growth and peak height velocity of children with sickle cell disease. Pediatr Blood Cancer. 2014;61(11):2024–30.
Billard M, Combet S, Hequet O, et al. Short-term femoral catheter insertion: a promising alternative to consistently allow long-term erythrocytapheresis therapy in children with sickle cell anemia. J Pediatr. 2013;162(2):423–6.
Kalff A, Dowsing C, Grigg A. The impact of a regular erythrocytapheresis programme on the acute and chronic complications of sickle cell disease in adults. Br J Haematol. 2010;149(5):768–74.
Masera N, Tavecchia L, Pozzi L, et al. Periodic erythroexchange is an effective strategy for high risk paediatric patients with sickle-cell disease. Transfus Apher Sci. 2007;37(3):241–7.
Quirolo K, Bertolone S, Hassell K, et al. The evaluation of a new apheresis device for automated red blood cell exchange procedures in patients with sickle cell disease. Transfusion. 2015;55(4):775–81.
Sarode R, Matevosyan K, Rogers ZR, et al. Advantages of isovolemic hemodilution-red cell exchange therapy to prevent recurrent stroke in sickle cell anemia patients. J Clin Apher. 2011;26(4):200–7.
Shrestha A, Jawa Z, Koch KL, et al. Use of a dual lumen port for automated red cell exchange in adults with sickle cell disease. J Clin Apher. 2015;30(6):353–8.
Kuo KHM, Barth D. A comparison of automated red blood cell depletion/exchange to automated red cell blood exchange in sickle cell patients. Blood. 2012;120(21):2281.
Sturgeon JP, Mayhew MA, Campbell J, Willis FM. Automated erythrocytapheresis in sickle cell disease: impact on hospital admission rate and iron loading. Blood. 2009;114(22):1522.
Todd S, Quinn J, Calvey A, et al. Review of regular automated red cell exchange transfusions and the associated risk of iron overload in patients with sickle cell disease. Br J Haematol. 2015;169:22–3.
Baker D, Strahlendorf C. Pediatric red blood cell exchange on the spectra optia. J Clin Apher. 2013;28(2):106.
Willis R, Manis J, Sloan S, et al. Chronic red blood cell exchange in patients with iron overload. J Clin Apher. 2011;26(2):76–7.
Trompeter S, Huntley N, Porter JB, et al. Red cell depletion in automated red cell exchange: a safe and effective method of exchange transfusion whilst reducing blood usage. Br J Haematol. 2015;169:91–2.
Ma L, Afenyi Annan A, Redding-Lallinger R, Badarenko N. Comparison of automated red blood cell exchange transfusion by apheresis with and without isovolemic hemodilution for the management of sickle cell disease. J Clin Apher. 2005;20:3–4.
Carrara P, Balocco M, Pinto V, et al. Manual erythro exchange for chronic transfusion therapy in patients with sickle cell syndromes unresponsive to hydroxyurea: a long-term follow-up. Am J Hematol. 2010;85(12):974.
Webb J, Le N, Hall NE, et al. Challenges and outcomes in applying pediatric stroke prophylaxis guidelines to adult sickle cell patients. Transfusion. 2014;54:182A–3A.
Adams DM, Schultz WH, Ware RE, Kinney TR. Erythrocytapheresis can reduce iron overload and prevent the need for chelation therapy in chronically transfused pediatric patients. J Pediatr Hematol Oncol. 1996;18(1):46–50.
Hilliard LM, Williams BF, Lounsbury AE, Howard TH. Erythrocytapheresis limits iron accumulation in chronically transfused sickle cell patients. Am J Hematol. 1998;59(1):28–35.
Kaushal M, Meier E, Miles M, et al. Efficacy of chronic red cell exchange in reducing iron overload in chronically transfused sickle cell disease patients. Pediatr Blood Cancer. 2013;60:S23–4.
Singer ST, Quirolo K, Nishi K, et al. Erythrocytapheresis for chronically transfused children with sickle cell disease: an effective method for maintaining a low hemoglobin S level and reducing iron overload. J Clin Apher. 1999;14(3):122–5.
Asma S, Kozanoglu I, Tarim E, et al. Prophylactic red blood cell exchange may be beneficial in the management of sickle cell disease in pregnancy. Transfusion. 2015;55(1):36–44.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Anwar F, Abdelaal M, Jastaniah W, et al. Minimizing red cells exposure to SCD patients by depletion-followed-by-exchange approach. American Society for Apheresis. 2015 conference, San Antonio, Texas.
Anwar F, Abdelaal MA, Khalil MM, et al. Red cell depletion followed by exchange transfusion in sickle cell disease patients using a new apheresis platform. Transfusion. 2010;50:85A.
Bahrani AAL, Al-Anazi K, Al-Amri A, et al. Developing evidence based automated red cell exchange programme in the Eastern Province of Saudi Arabia. Vox Sang. 2011;101:293.
Kinney S, Schmidt A, Nord B, Lammers K. An initial single-center experience with red cell exchange transitioning from Cobe Spectra apheresis system to Spectra Optia apheresis system. American Society for Apheresis. 2015 conference, San Antonio, Texas.
National Institute for Health and Care Excellence. Spectra Optia apheresis device for automatic red blood cell exchange in patients with sickle cell disease: communication log. 2015. Available from: https://www.nice.org.uk/guidance/MTG28/documents/correspondence-with-eac. Accessed 7 Sept 2016.
Excellence NIfHaC. Resource impact report: Spectra Optia for automated red blood cell exchange in patients with sickle cell disease (MTG28). 2016. Available from: https://www.nice.org.uk/guidance/mtg28/resources/resource-impact-report-2366729245. Accessed 15 Apr 2016.
Campbell B, Campbell M. NICE medical technologies guidance: a novel and rigorous methodology to address a new health technology assessment challenge. Appl Health Econ Health Policy. 2012;10(5):295–7.
NHS England. Guide to the enhanced tariff option for 2015/16. 2016. Available from: https://www.england.nhs.uk/resources/pay-syst/tariff-guide/. Accessed 22 Apr 2016.
Foster M. Sickle cell reports. National Haemoglobinopathy Registry: report 2013/2014; 2014.
Therapeutic Apheresis Services. 2015. Available from: http://hospital.blood.co.uk/patient-services/therapeutic-apheresis-services/. Accessed 22 Apr 2016.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Author contributions
All authors contributed to the original assessment report. This summary was prepared by Iain Willits with editorial contributions from all co-authors. The guarantor for the overall content is Andrew Sims.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Newcastle upon Tyne Hospitals and York Health Economics Consortium are funded by NICE to act as an EAC for the Medical Technologies Evaluation Programme. The evaluation of sponsor-provided medical technology submissions is part of the remit of the EAC.
Conflict of interest
Four of the authors (Iain Willits, Helen Cole, Roseanne Jones and Andrew Sims) are NHS employees; the NHS has a financial interest in the guidance issued by NICE as a result of this work. Michelle Jenks, Joyce Craig and Mick Arber work for the EAC but otherwise have no conflicts of interest. Kimberley Carter is an employee of NICE. This summary has been reviewed by NICE but has not been externally peer reviewed by Applied Health Economics and Health Policy.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s40258-017-0322-1.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Willits, I., Cole, H., Jones, R. et al. Spectra Optia® for Automated Red Blood Cell Exchange in Patients with Sickle Cell Disease: A NICE Medical Technology Guidance. Appl Health Econ Health Policy 15, 455–468 (2017). https://doi.org/10.1007/s40258-016-0302-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-016-0302-x