Abstract
Purpose of Review
The purpose of this review is to assist clinicians in making evidence-based pharmacologic choices for treating pain in children. Pain is one of the most common reasons patients present to an Emergency Department. Determining the most appropriate way to control pain is a challenge in adults, but is even more difficult when treating infants and small children because of their increased risk of complications related to treatment. Historically, children with pain were treated less often and less aggressively than adults for a variety of reasons. Better tools for assessment and improved management guidelines have given pediatric providers the ability to apply more appropriate therapy.
Recent Findings
New options for analgesia offer safer, more effective treatment. Traditionally held ideas about safety and efficacy of many medications have recently come into question.
Summary
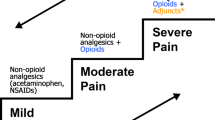
Treatment of pediatric pain begins with effective assessment. After assessing the pain level, the type and dose of pain control can be determined. Mild pain can be controlled with oral non-narcotic medications, while moderate to severe pain is often treated with a combination of non-narcotic and opiate analgesics. Venipuncture and brief procedural pain can be addressed with a variety of topical agents.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Unruh A and McGrath P: History of pain in children. In McGrath P, Stevens B, Walker S, Zempsky Z, editors. Oxford Textbook of Pediatric Pain. Oxford: Oxford University Press; 2013. Accessed on 3/21/17 at https://doi.org/10.1093/med/9780199642656.001.0001/med-9780199642656-chapter-1?print=pdf
Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997;23(3):293–7.
Voepel-Lewis T, Zanotti J, Dammeyer JA, et al. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. Am J Crit Care. 2010;19(1):55–61.
Garra G, Singer A, Taira B, et al. Validation of the Wong-Baker FACES pain rating scale in pediatric emergency department patients. Acad Emerg Med. 2009;17(1):50–4.
Motov S and Ast T. Is there a limit to the analgesic effect of pain medications? Accessed on 3/26/17 at http://www.medscape.com/viewarticle/574279.
Perrott D, Piira T, Goodenough B, et al. Efficacy and safety of acetaminophen vs ibuprofen for treating children’s pain or fever. Arch Pediatr Adolesc Med. 2004;158:521–6.
Sjoukes A, Venekamp RP, van de Pol A et al. Paracetamol (acetaminophen) or non-steroidal anti-inflammatory drugs, alone or combined, for pain relief in acute otitis media in children. Cochrane Database of Systematic Reviews December 2016; 12 accessed on 3/24/17 at http://www.cochrane.org/CD011534/ARI_pain-relievers-children-acute-middle-ear-infection
Clark E, Plint A, Correll R, et al. A randomized, controlled trial of acetaminophen, ibuprofen, and codeine for acute pain relief in children with acute musculoskeletal trauma. Pediatrics. 2006;119(3):460–7.
Hartling L, Ali A, Dryden D et al. How safe are common analgesics for the treatment of acute pain in children? A systematic review. Pain Research and Management 2016; accessed on 3/24/17 at https://doi.org/10.1155/2016/5346819.
Usyal HY, Takmaz SA, Yaman F, et al. The efficacy of intravenous paracetamol versus tramadol for postoperative analgesia after adenotonsillectomy in children. J Clin Anesth. 2011;23:52–7.
Sheehan W, Mauger D, Paul I, et al. Acetaminophen versus ibuprofen in young children with mild persistent asthma. N Engl J Med. 2016;375(7):619–30.
Dart RC, Rumack BH. Intravenous acetaminophen in the United States: iatrogenic dosing errors. Pediatrics. 2012;129(2):349–53. https://doi.org/10.1542/peds.2011-2345.
Bremerich DH, Neidhart G, Heimann K, et al. Prophylactically-administered rectal acetaminophen does not reduce postoperative requirements in infants and small children undergoing elective cleft palate repair. Anesth Analg. 2001;92:907–12.
van der Marel CD, van Lingen RA, Pluim MAL, et al. Analgesic efficacy of rectal versus oral acetaminophen in children after major craniofacial surgery. Clin Pharmacol Ther. 2001;70(1):82–90. https://doi.org/10.1067/mcp.2001.116794.
Capici F, Ingelmo P, Davidson A, et al. Randomized controlled trial of duration of analgesia following intravenous or rectalacetaminophen following tonsillectomy in children. Br J Anaesth. 2008;100(2):251–5.
Arana A, Morton N, Hansen T. Treatment with paracetamol in infants. Acta Anaesthesiol Scand. 2001;45(1):20–9. https://doi.org/10.1034/j.1399-6576.2001.450104.x.
Kennedy R, Luhmann JD. The “ouchless emergency department.” getting closer: advances in decreasing distress during painful procedures in the emergency department. Pediatr Clin N Am. 1999;46:1215–47.
Schnabel A, Reichl S, Mayer-Friebem C et al. Tramadol for postoperative pain in children. Cochrane Database Systemic Reviews 2015; accessed on 3/30/2017 at https://doi.org/10.1002/14651858.CD009574.pub2/abstract
•• Friday JH, Kanegaye JT, McCaslin I, et al. Ibuprofen provides analgesia equivalent to acetaminophen-codeine in the treatment of acute pain in children with extremity injuries a randomized controlled trial. Acad Emerg Med. 2009;16(8):711–6. Data supporting more use of NSAIDs as a superior alternative to codeine. Codeine had been for many years a go-to medication choice to treat more severe pediatric pain.
Dean L. Codeine therapy and CYP4D6 genotype. Medical Genetics Summaries, accessed on 3/30/2017 at https://www.ncbi.nlm.nih.gov/books/NBK100662/
Yang YT, Chen B, Bennett C. FDA approval of extended-release oxycodone for children with severe pain. Pediatrics. 2016;137(5):e20160205. https://doi.org/10.1542/peds.2016-0205.
FDA Drug Safety Communication: Safety review update of codeine use in children; new Boxed Warning and Contraindication on use after tonsillectomy and/or adenoidectomy. http://www.fda.gov/Drugs/DrugSafety/ucm339112.htm.
Boyle K, Rosenbaum C. Oxycodone overdose in the pediatric population: case files of the University of Massachusetts Medical Toxicology Program. J Med Toxicol. 2014;10(3):280–5.
El-Tahtawy A, Kokki H, Reidenberg B. Population pharmacokinetics of oxycodone in children 6 months to 7 years old. J Clin Pharmacol. 2006;46(4):433–42. https://doi.org/10.1177/0091270006286433.
Oxycodone accessed on 3/30/17 at https://online.epocrates.com/drugs/5902/oxycodone/Peds-Dosing
Data available at http://www.epocrates.com
Saunders M, Adelgais K, Nelson D. Use of intranasal fentanyl for the relief of pediatric orthopedic trauma pain. Acad Emerg Med. 2010;17(11):1155–61. https://doi.org/10.1111/j.1553-2712.2010.00905.x.
Jain S, Hegenbarth M, Humiston S, et al. Increasing ED use of jet injection of lidocaine for IV-related pain management. Pediatrics. 2017;139(4):e20161697.
• Del Pizzo J, Callahan J. Intranasal medications in pediatric emergency medicine. Pediatric Emergency Care. 2014;30(7):496–504. Intranasal use of opiate analgesics has the potential to give children excellent pain relief without the risk and pain associated with intravenous injection, and should be used more in EDs.
Graudins A, Meek R, Egerton-Warburton D, et al. The PICHFORK (pain in children fentanyl or ketamine) Trial: a randomized controlled trial comparing intranasal ketamine and fentanyl for the relief of moderate to severe pain in children with limb injuries. Ann Emerg Med. 2015;65(3):248–54.
Acute TJ. pain management in infants. Pediatr Ann. 2014;43(7):e169–75.
Hauer J, Duncan J, Fowler Scullion B. Pediatric pain and symptom management guidelines: Dana Farber Cancer Institute/Children’s Hospital Boston. Accessed on 3/30/17 at http://www.hpccv.org/resources/Blue%20Book%202011%20(2).pdf
• Berde CB. Toxicity of local anesthetics in infants and children. Journal of Pediatrics. 1993;122:S14–20. A review of options for reducing pain of procedures for children in the ED. Many of these concepts were new and not commonly implemented at the time of publication, and although they represent the standard of care in pediatric EDs now, many community hospital general care EDs have not fully implemented these best practices.
Griffith R, Jordan V, Herd D et al. Vapocoolants (cold spray) for pain treatment during intravenous cannulation. Cochrane Database Systemic Reviews2016. Accessed on 3/28/17 at http://www.cochrane.org/CD009484/ANAESTH_vapocoolants-cold-spray-pain-treatment-during-intravenous-cannulation
Kleiber C, Sorenson M, Whiteside K, et al. Topical anesthetics for intravenous insertion in children: a randomized equivalency study. Pediatrics. 2002;110:758–61.
Eichenfield LF, Funk A, Fallon-Friedlander S, Cunningham BB. A clinical study to evaluate the efficacy of ELA-Max (4% liposomal lidocaine) as compared with eutectic mixture of local anesthetics cream for pain reduction of venipuncture in children. Pediatrics. 2002;109(6):1093–9. https://doi.org/10.1542/peds.109.6.1093.
Koh JL, Harrison D, Myers R, et al. A randomized, double-blind comparison study of EMLA and ELA-max for topical anesthesia in children undergoing intravenous insertion. Paediatr Anaesth. 2004;14:977–82.
Sawyer J, Febbraro S, Masud S, Ashburn MA, Campbell JC. Heated lidocaine/tetracaine patch (SYNERA®, Rapydan) compared with lidocaine/prilocaine cream (EMLA) for topical anaesthesia before vascular access. Br J Anaesth. 2009;102(2):210–5. https://doi.org/10.1093/bja/aen364.
Synera, Pediatric Patients. Accessed on 3/30/17 at http://www.synera.com/pediatric-patients/faq/
Singer AJ, Taira BR, Chisena EN, Gupta N, Chipley J. Warm lidocaine/tetracaine patch versus placebo before pediatric intravenous cannulation: a randomized controlled trial. Ann Emerg Med. 2008;52(1):41–7. https://doi.org/10.1016/j.annemergmed.2008.01.336.
Clark E, Plint R, Correll I et al. A randomized, controlled trial f acetaminophen, ibuprofen, and codeine for acute pain relief in children with musculoskeletal trauma. Pediatrics 2007; 119(3): 460–467, DOI: https://doi.org/10.1542/peds.2006-1347.
Charney R, Yan Y, Schootman M, et al. Oxycodone versus codeine for triage pain in children with suspected forearm fracture. Pediatr Emerg Care. 2008;24(9):595–600.
EMLA at drugs.com. Accessed on 3/28/2017 at https://www.drugs.com/pro/emla.html
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Pain Management
Rights and permissions
About this article
Cite this article
Welsh, J., Welsh, T. The Safe and Successful Management of Acute Pain in the Infant and Young Child. Curr Emerg Hosp Med Rep 6, 37–43 (2018). https://doi.org/10.1007/s40138-018-0153-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-018-0153-x