Abstract
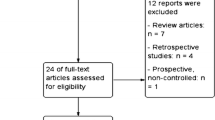
The purpose of this review was to critically evaluate literature published over the past three years regarding outcomes and costs of robotic sacrocolpopexy (RSC) versus laparoscopic sacrocolpopexy (LSC). A total of eight studies were selected that directly compared these techniques: two randomized controlled trials, one prospective trial, and five retrospective trials, with follow-ups ranging from three months to three years. RSC and LSC resulted in similar objective and subjective success rates, quality of life outcomes and overall perioperative complication rates. RSC required similar or longer operative times, caused similar or less blood loss and resulted in more short-term postoperative pain. RSC was also associated with higher costs compared to LSC, but this difference was minimal when excluding the robot purchase cost from calculations. Although complication rates were not significantly different in a majority of the studies, the largest retrospective study demonstrated that RSC resulted in a significant increase in the risk of venous thromboembolism and of a conversion to an open procedure. The ultimate choice of route and method of sacrocolpopexy should be individualized, taking into account the surgeon’s experience and the patient's history and characteristics. In conclusion, RSC is an acceptable alternative to LSC for the management of apical vaginal prolapse, but longer follow-up is needed with studies specifically powered to detect differences in costs and outcomes.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstet Gynecol. 2009;114:1278–83.
Nygaard I, Barber MD. Prevalence of symptomatic pelvic floor disorders in US Women. JAMA. 2008;300:1311–6.
Swift S, Tate SB, Nicholas J. Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol. 2003;189:372–9.
Jelovsek JE, Barber MD. Women seeking treatment for advanced pelvic organ prolapse have decreased body image and quality of life. Am J Obstet Gynecol. 2006;194:1455–61.
Hullfish KL, Trowbridge ER, Stukenborg GJ. Treatment strategies for pelvic organ prolapse: a cost-effectiveness analysis. Int Urogynecol J. 2011;22:507–15.
Cheon C, Maher C. Economics of pelvic organ prolapse surgery. Int Urogynecol J. 2013;24:1873–6.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–6.
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson FM. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123:1201–6.
Smith FJ, Holman CDJ, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116:1096–100.
Wu JM, Kawasaki A, Hundley AF, Dieter AA, Myers ER, Sung VW. Predicting the number of women who will undergo incontinence and prolapse surgery, 2010 to 2050. Am J Obstet Gynecol Elsevier. 2011;205:230.e1–5.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol. 2002;187:116–26.
Maher C, Baessler K, Glazener CM, Adams EJ, Hagen S. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. doi:10.1002/14651858.CD004014.pub3.
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G, Weber AM, et al. Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol. 2004;104:805–23.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff GW, Richter HE, Gantz M, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2014;309:2016–24. Outcomes of Colpopexy and Urinary Reduction Efforts (CARE) trial of abdominal sacrocolpopexy with or without urethropexy, with 59% (126/215) follow-up at 7 years, which found increased anatomic and subjective treatment failure and mesh erosion, between years 2 and 7 postoperatively.
Brubaker L, Nygaard I, Richter HE, Visco A, Weber AM, Cundiff GW, et al. Two-year outcomes after sacrocolpopexy with and without burch to prevent stress urinary incontinence. Obstet Gynecol. 2008;112:49–55.
Freeman RM, Pantazis K, Thomson A, Frappell J, Bombieri L, Moran P, et al. A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J. 2013;24:377–84.
Paraiso MFR, Walters MD, Rackley RR, Melek S, Hugney C. Laparoscopic and abdominal sacral colpopexies: a comparative cohort study. Am J Obstet Gynecol. 2005;192:1752–8.
Hsiao KC, Latchamsetty K, Govier FE, Kozlowski P, Kobashi KC. Comparison of laparoscopic and abdominal sacrocolpopexy for the treatment of vaginal vault prolapse. J Endourol. 2007;21:926–30.
Klauschie JL, Suozzi BA, O’Brien MM, McBride AW. A comparison of laparoscopic and abdominal sacral colpopexy: objective outcome and perioperative differences. Int Urogynecol J. 2008;20:273–9.
Ganatra AM, Rozet F, Sanchez-Salas R, Barret E, Galiano M, Cathelineau X, et al. The current status of laparoscopic sacrocolpopexy: a review. Eur Urol. 2009;55:1089–105.
Parnell BA, Matthews CA. Robot-assisted techniques and outcomes in the realm of pelvic reconstructive surgery. Clin Obstet Gynecol. 2011;54:412–9.
Li H, Sammon J, Roghmann F, Sood A, Ehlert M, Sun M, et al. Utilization and perioperative outcomes of robotic vaginal vault suspension compared to abdominal or vaginal approaches for pelvic organ prolapse. CUAJ. 2014;8:100–6.
Siddiqui NY, Geller EJ, Visco AG. Symptomatic and anatomic 1-year outcomes after robotic and abdominal sacrocolpopexy. Am J Obstet Gynecol. 2012;206:435.e1–5.
Hoyte L, Rabbanifard R, Mezzich J, Bassaly R, Downes K. Cost analysis of open versus robotic-assisted sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2012;18:335–9.
Geller EJ, Siddiqui NY, Wu JM, Visco AG. Short-term outcomes of robotic sacrocolpopexy compared with abdominal sacrocolpopexy. Obstet Gynecol. 2008;112:1201–6.
Geller EJ, Parnell BA, Dunivan GC. Robotic vs abdominal sacrocolpopexy: 44-month pelvic floor outcomes. Urology. 2012;79:532–6.
Anand M, Woelk JL, Weaver AL, Trabuco EC, Klingele CJ, Gebhart JB. Perioperative complications of robotic sacrocolpopexy for post-hysterectomy vaginal vault prolapse. Int Urogynecol J. 2014;1–8.
Linder BJ, Elliott DS. Robotic sacrocolpopexy: how does it compare with other prolapse repair techniques? Curr Urol Rep. 2013;14:235–9.
Visco AG, Advincula AP. Robotic gynecologic surgery. Obstet Gynecol. 2008;112:1369–84.
Barber MD, Maher C. Apical prolapse. Int Urogynecol J. 2013;24:1815–33.
Sung HH, Park BH, Ryu DS, Lee KS. Recent advances in robotic surgery in female urology. Int J Urol. 2013;20:1154–62.
Liu H, Lu D, Wang L, Shi G, Song H, Clarke J. Robotic surgery for benign gynaecological disease. Cochrane Database Syst Rev. 2012;1–3.
Gurusamy KS, Samraj K, Fusai G, Davidson BR. Robot assistant versus human or another robot assistant in patients undergoing laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2012;1–28.
Paraiso MFR, Jelovsek JE, Frick A, Chen CCG, Barber MD. Laparoscopic compared with robotic sacrocolpopexy for vaginal prolapse. Obstet Gynecol. 2011;118:1005–13. RCT of 35 RSC and 35 LSC post-hysterectomy patients, which found increased cost, operating time, and postoperative pain with RSC; no difference in complications, anatomic or subjective success at 1 year.
Anger JT, Mueller ER, Tarnay C, Smith B, Stroupe K, Rosenman A, et al. Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2014;123:5–12. RCT of 40 RSC and 38 LSC, which found increased cost, operating time, and postoperative pain with RSC; no difference in complications, anatomic or subjective success at 6 months.
Seror J, Yates DR, Seringe E, Vaessen C, Bitker M-O, Chartier-Kastler E, et al. Prospective comparison of short-term functional outcomes obtained after pure laparoscopic and robot-assisted laparoscopic sacrocolpopexy. World J Urol. 2011;30:393–8.
Nosti PA, Umoh Andy U, Kane S, White DE, Harvie HS, Lowenstein L, et al. Outcomes of abdominal and minimally invasive sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2014;20:33–7. Retrospective cohort study of 589 ASC, 262 RSC, and 273 LSC, which found increased operative time, conversion to open and risk of VTE with RSC; no difference in anatomic success at 8 months.
Antosh DD, Grotzke SA, McDonald MA, Shveiky D, Park AJ, Gutman RE, et al. Short-term outcomes of robotic versus conventional laparoscopic sacral colpopexy. Female Pelvic Med Reconstr Surg. 2012;18:158–61.
Awad N, Mustafa S, Amit A, Deutsch M, Eldor-Itskovitz J, Lowenstein L. Implementation of a new procedure: laparoscopic versus robotic sacrocolpopexy. Arch Gynecol Obstet. 2012;287:1181–6.
Chan S, Pang S, Cheung TH, Cheung R, Chung T. Laparoscopic sacrocolpopexy for the treatment of vaginal vault prolapse: with or without robotic assistance. Hong Kong Med J. 2011;17:54–60.
Tan-Kim J, Menefee SA, Luber KM, Nager CW, Lukacz ES. Robotic-assisted and laparoscopic sacrocolpopexy: comparing operative times, costs and outcomes. Female Pelvic Med Reconstr Surg. 2011;17:44–9. Retrospective cohort study of 43 RSC and 61 LSC post-hysterectomy patients, increased operating time and surgical costs with RSC; no difference in complications, anatomic success, or satisfaction at 29 months.
Elterman DS, Chughtai BI, Vertosick E, Maschino A, Eastham JA, Sandhu JS. Changes in pelvic organ prolapse surgery in the last decade among United States Urologists. J Urol. 2014;191:1022–7.
Serati M, Bogani G, Sorice P, Braga A, Torella M, Salvatore S, et al. Robot-assisted Sacrocolpopexy for Pelvic Organ Prolapse: A Systematic Review and Meta-analysis of Comparative Studies. Eur Urol Eur Assoc Urol. 2014;1–16.
Tan-Kim J, Menefee SA, Luber KM, Nager CW, Lukacz ES. Prevalence and risk factors for mesh erosion after laparoscopic-assisted sacrocolpopexy. Int Urogynecol J. 2010;22:205–12.
Lee RK, Mottrie A, Payne CK, Waltregny D. A review of the current status of laparoscopic and robot-assisted sacrocolpopexy for pelvic organ prolapse. Eur Urol Eur Assoc Urol. 2014;65:1128–37.
U.S. Food and Drug Administration. Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy: FDA Safety Communication. Silver Spring MD; 2014;1–5. Available at: http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm393576.htm. Retrieved August 10, 2014.
The American College of Obstetricians and Gynecologists. Power Morcellation and Occult Malignancy in Gynecologic Surgery. Washington D.C; 2014;1–6. Available at: http://www.acog.org/Resources-And-Publications/Task-Force-and-Work-Group-Reports/Power-Morcellation-and-Occult-Malignancy-in-Gynecologic-Surgery. Retrieved August 10, 2014.
The American Urogynecologic Society. AUGS Position Statement: Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy. Washington D.C; 2014;1–1. Available at: www.augs.org/d/do/2872. Retrieved August 10, 2014.
AAGL Advancing Minimally Invasive Gynecology Worldwide. AAGL position statement: robotic-assisted laparoscopic surgery in benign gynecology. J Minim Invasive Gynecol. 2013;20:2–9. Available at: http://www.aagl.org/wp-content/uploads/2013/03/aagl-robotic-position-statement.pdf.; Retrieved August 10, 2014.
Barbash G, Glied S. New technology and health care costs - the case of robot-assisted surgery. N Engl J Med. 2010;363:701–4.
Nieboer TE, Aarts J. Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial- comment. Obstet Gynecol. 2014;123:1357–8.
Mueller ER, Kenton K, Tarnay C, Brubaker L, Rosenman A, Smith B, et al. Abdominal Colpopexy: Comparison of Endoscopic Surgical Strategies (ACCESS). Contemp Clin Trials. 2012;33:1011–8.
Elliott CS, Hsieh MH, Sokol ER, Comiter CV, Payne CK, Chen B. Robot-assisted versus open sacrocolpopexy: a cost- minimization analysis. J Urol. 2012;187:638–43.
Judd JP, Siddiqui NY, Barnett JC, Visco AG, Havrilesky LJ, Wu JM. Cost-minimization analysis of robotic-assisted, laparoscopic, and abdominal sacrocolpopexy. J Minim Invasive Gynecol. 2010;17:493–9.
Geller EJA, Lin FCB, Matthews CAA. Analysis of robotic performance times to improve operative efficiency. J Minim Invasive Gynecol. 2013;20:43–8.
Akl MN, Long JB, Giles DL, Cornella JL, Pettit PD, Chen AH, et al. Robotic-assisted sacrocolpopexy: technique and learning curve. Surg Endosc. 2009;23:2390–4.
Claerhout F, Verguts J, Werbrouck E, Veldman J, Lewi P, Deprest J. Analysis of the learning process for laparoscopic sacrocolpopexy: identification of challenging steps. Int Urogynecol. 2014;1–7.
Mustafa S, Amit A, Filmar S, Deutsch M, Netzer I, Itskovitz-Eldor J, et al. Implementation of laparoscopic sacrocolpopexy: establishment of a learning curve and short-term outcomes. Arch Gynecol Obstet. 2012;286:983–8.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Maher C, editor. Cochrane Database Syst Rev. 2013;4:CD004014.
Acknowledgements
The authors would like to thank Twinkle Parekh, a visiting medical student from the All India Institute of Medical Sciences in New Delhi, India, for her contributions.
Compliance with Ethics Guidelines
ᅟ
Conflict of Interest
Dr. Jennifer L. Hallock, Dr. Jocelyn Fitzgerald and Dr. Chi Chiung Grace Chen each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hallock, J.L., Fitzgerald, J. & Chen, C.C.G. Update on Robotic Versus Laparoscopic Sacrocolpopexy: Outcomes and Costs. Curr Obstet Gynecol Rep 3, 252–264 (2014). https://doi.org/10.1007/s13669-014-0099-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-014-0099-2