Abstract
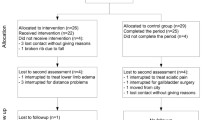
Muscle strength and joint mobility were decreased with type 1 diabetes mellitus (T1DM). However, the literature is limited about foot muscle strength, joint mobility, and structure in adolescent aged 13–17 with T1DM. The purpose of this study was to compare foot structure, muscle strength, and joint mobility of adolescents aged between 13 and 17 with T1DM to those of healthy adolescents. Cross-sectional study design including adolescents with T1DM aged 13–17 years, and healthy adolescents was used in the study. The range of motion (ROM) was measured by using a digital goniometer, and muscle strength was evaluated by using handheld-dynamometry. Footprint was used for foot structure. Assessments were performed by using the digital images, and Clarke’s angle (CA), Staheli Arch index (SAI), and Chippaux-Smirak index (CSI) were calculated by using a scientific image-analysis program, ImageJ. Forty-one T1DM and 28 healthy adolescents were included with a mean age of 15.29 ± 1.55 and 15.04 ± 1.42, respectively. The T1DM group had significantly lower dorsiflexion, inversion and eversion ROM, and lower tibialis anterior and gastrocnemius muscle test (p < 0.05, for all) compared with the control group. Statistically, significant differences were found in the right SAI and CSI between groups (p < 0.05), whereas no difference was found in CA (p > 0.05). Adolescents with T1DM have lower ankle and foot joint mobility and muscle strength and altered foot structure compared to their healthy contemporaries. This indicates that early screening of muscle strength and foot structure are important to determine and avoid various risks such as foot deformities, gait deviations, and ulcer.

Similar content being viewed by others
References
Lopez-Miranda J, Perez-Martinez P, Marin C, Fuentes F, Delgado J, Perez-Jimenez F. Dietary fat, genes and insulin sensitivity. J Mol Med (Berl). 2007;85(3):213–26.
VanBuecken D, Lord S, Greenbaum CJ. Changing the course of disease in type 1 diabetes. In: De Groot LJ, Beck-Peccoz P, Chrousos G, Dungan K, Grossman A, Hershman JM, et al., editors. Endotext. South Dartmouth: MDText.com, Inc.; 2000.
Patterson C, Guariguata L, Dahlquist G, Soltesz G, Ogle G, Silink M. Diabetes in the young—a global view and worldwide estimates of numbers of children with type 1 diabetes. Diabetes Res Clin Pract. 2014;103(2):161–75.
Sheehan AM, While AE, Coyne I. The experiences and impact of transition from child to adult healthcare services for young people with Type 1 diabetes: a systematic review. Diabet Med. 2015;32(4):440–58.
Amin N, Doupis J. Diabetic foot disease: from the evaluation of the "foot at risk" to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016;7(7):153–64.
Merashli M, Chowdhury TA, Jawad AS. Musculoskeletal manifestations of diabetes mellitus. QJM. 2015;108(11):853–7.
Andreassen CS, Jakobsen J, Ringgaard S, Ejskjaer N, Andersen H. Accelerated atrophy of lower leg and foot muscles—a follow-up study of long-term diabetic polyneuropathy using magnetic resonance imaging (MRI). Diabetologia. 2009;52(6):1182–91.
Andersen H, Nielsen S, Mogensen CE, Jakobsen J. Muscle strength in type 2 diabetes. Diabetes. 2004;53(6):1543–8.
Andersen H, Gadeberg PC, Brock B, Jakobsen J. Muscular atrophy in diabetic neuropathy: a stereological magnetic resonance imaging study. Diabetologia. 1997;40(9):1062–9.
Andersen H, Gjerstad MD, Jakobsen J. Atrophy of foot muscles: a measure of diabetic neuropathy. Diabetes Care. 2004;27(10):2382–5.
Boulton AJ. The pathogenesis of diabetic foot problems: an overview. Diabet Med. 1996;13(Suppl 1):S12–6.
Erol K, Karahan AY, Kerimoglu U, Ordahan B, Tekin L, Sahin M, et al. An important cause of pes planus: the posterior tibial tendon dysfunction. Clin Pract. 2015;5(1):699.
Allan J, Munro W, Figgins E. Foot deformities within the diabetic foot and their influence on biomechanics: a review of the literature. Prosthetics Orthot Int. 2016;40(2):182–92.
Rosenbaum AJ, Lisella J, Patel N, Phillips N. The cavus foot. Med Clin North Am. 2014;98(2):301–12.
Fernando M, Crowther R, Lazzarini P, Sangla K, Cunningham M, Buttner P, et al. Biomechanical characteristics of peripheral diabetic neuropathy: a systematic review and meta-analysis of findings from the gait cycle, muscle activity and dynamic barefoot plantar pressure. Clin Biomech (Bristol, Avon). 2013;28(8):831–45.
Toth C, Hebert V, Gougeon C, Virtanen H, Mah JK, Pacaud D. Motor unit number estimations are smaller in children with type 1 diabetes mellitus: a case-cohort study. Muscle Nerve. 2014;50(4):593–8.
Margeirsdottir HD, Larsen JR, Kummernes SJ, Brunborg C, Dahl-Jorgensen K. The establishment of a new national network leads to quality improvement in childhood diabetes: implementation of the ISPAD Guidelines. Pediatr Diabetes. 2010;11(2):88–95.
Clarkson HM. Musculoskeletal assessment: joint range of motion and manual muscle strength: Lippincott Williams & Wilkins; 2000.
Hebert LJ, Maltais DB, Lepage C, Saulnier J, Crete M, Perron M. Isometric muscle strength in youth assessed by hand-held dynamometry: a feasibility, reliability, and validity study. Pediatr Phys Ther. 2011;23(3):289–99.
Wever A, Schickenberg-Werrij BG, Willems J, Schaper NC, Schott DA. Prevalence and awareness of functional and structural foot abnormalities in children and adolescents with type 1 diabetes. J Pediatr Endocrinol Metab. 2016; doi:10.1515/jpem-2015-0455.
Stark T, Walker B, Phillips JK, Fejer R, Beck R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: a systematic review. PM R. 2011;3(5):472–9.
Escolar DM, Henricson EK, Mayhew J, Florence J, Leshner R, Patel KM, et al. Clinical evaluator reliability for quantitative and manual muscle testing measures of strength in children. Muscle Nerve. 2001;24(6):787–93.
Clarke HH. An objective method of measuring the height of the longitudinal arch in foot examinations. Research Quarterly American Physical Education Association. 1933;4(3):99–107.
Razeghi M, Batt ME. Foot type classification: a critical review of current methods. Gait & posture. 2002;15(3):282–91.
Chen KC, Yeh CJ, Kuo JF, Hsieh CL, Yang SF, Wang CH. Footprint analysis of flatfoot in preschool-aged children. Eur J Pediatr. 2011;170(5):611–7.
Staheli LT, Chew DE, Corbett M. The longitudinal arch. A survey of eight hundred and eighty-two feet in normal children and adults. J Bone Joint Surg Am. 1987;69(3):426–8.
Forriol F, Pascual J. Footprint analysis between three and seventeen years of age. Foot Ankle. 1990;11(2):101–4.
Queen RM, Mall NA, Hardaker WM, Nunley II. JA. Describing the medial longitudinal arch using footprint indices and a clinical grading system. Foot & ankle international. 2007;28(4):456–62.
Echarri JJ, Forriol F. The development in footprint morphology in 1851 Congolese children from urban and rural areas, and the relationship between this and wearing shoes. J Pediatr Orthop B. 2003;12(2):141–6.
Rosenbloom AL. Limited joint mobility in childhood diabetes: discovery, description, and decline. J Clin Endocrinol Metab. 2013;98(2):466–73.
Francia P, Seghieri G, Gulisano M, De Bellis A, Toni S, Tedeschi A, et al. The role of joint mobility in evaluating and monitoring the risk of diabetic foot ulcer. Diabetes Res Clin Pract. 2015;108(3):398–404.
Nagesh VS, Kalra S. Type 1 diabetes: syndromes in resource-challenged settings. J Pak Med Assoc. 2015;65(6):681–5.
Greenman RL, Khaodhiar L, Lima C, Dinh T, Giurini JM, Veves A. Foot small muscle atrophy is present before the detection of clinical neuropathy. Diabetes Care. 2005;28(6):1425–30.
Barnett SJ, Shield JP, Potter MJ, Baum JD. Foot pathology in insulin dependent diabetes. Arch Dis Child. 1995;73(2):151–3.
van Schie CH, Vermigli C, Carrington AL, Boulton A. Muscle weakness and foot deformities in diabetes: relationship to neuropathy and foot ulceration in caucasian diabetic men. Diabetes Care. 2004;27(7):1668–73.
Cheuy VA, Hastings MK, Commean PK, Mueller MJ. Muscle and joint factors associated with forefoot deformity in the diabetic neuropathic foot. Foot & ankle international. 2015; doi:10.1177/1071100715621544.
Kothari A, Bhuva S, Stebbins J, Zavatsky AB, Theologis T. An investigation into the aetiology of flexible flat feet: the role of subtalar joint morphology. Bone Joint J. 2016;98-b(4):564–8.
Aggarwal N, Garg C, Bawa H. Comparison of foot posture in runners (sprinters) and non runners in Indian population. The Physiotherapy Post. 6(1):268–71.
Riddiford-Harland DL, Steele JR, Storlien LH. Does obesity influence foot structure in prepubescent children? International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 2000;24(5):541–4.
Pita-Fernandez S, Gonzalez-Martin C, Seoane-Pillado T, Lopez-Calvino B, Pertega-Diaz S, Gil-Guillen V. Validity of footprint analysis to determine flatfoot using clinical diagnosis as the gold standard in a random sample aged 40 years and older. Journal of epidemiology. 2015;25(2):148–54.
Villarroya MA, Esquivel JM, Tomas C, Moreno LA, Buenafe A, Bueno G. Assessment of the medial longitudinal arch in children and adolescents with obesity: footprints and radiographic study. Eur J Pediatr. 2009;168(5):559–67.
Francia P, Anichini R, De Bellis A, Seghieri G, Lazzeri R, Paternostro F, et al. Diabetic foot prevention: the role of exercise therapy in the treatment of limited joint mobility, muscle weakness and reduced gait speed. Ital J Anat Embryol. 2015;120(1):21–32.
Singla R, Gupta Y, Kalra S. Musculoskeletal effects of diabetes mellitus. J Pak Med Assoc. 2015;65(9):1024–7.
Acknowledgments
We thank all the participants involved in the survey. The help of ……..Omer Inan from …….Bandirma Onyedi Eylul University for the English review of the manuscript is very much acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
There is no financial support or other benefits from commercial sources for the work.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Kaya Mutlu, E., Unver, B., Taskiran, H. et al. An investigation of the foot ankle joint mobility, muscle strength, and foot structure in adolescent with type 1 diabetes. Int J Diabetes Dev Ctries 38, 108–114 (2018). https://doi.org/10.1007/s13410-017-0556-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-017-0556-3