Abstract
Background and Objectives
The probiotic bacterium Escherichia coli strain Nissle 1917 has previously been shown to alter the pharmacokinetics of amiodarone. The aim of this study was to determine whether the probiotic bacterium Lactobacillus casei produces similar alterations in amiodarone disposition.
Methods
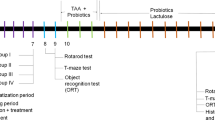
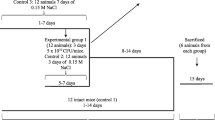
A suspension of live probiotic bacteria L. casei strain DN-114 001 (1.5 × 109 CFU/dose; probiotic pre-treated group) or a saline solution (control group) was administered directly into the stomach of male Wistar rats (N = 30 in each group) by oral gavage daily for 7 consecutive days. On the eighth day, all rats (N = 60) were given a single oral dose of an amiodarone hydrochloride suspension (model drug; 50 mg/kg). The concentrations of amiodarone and of its main metabolite N-desethylamiodarone were determined in rat plasma by high-performance liquid chromatography.
Results
Comparison of the pharmacokinetics of amiodarone in the control group and probiotic pre-treated group revealed that the peak plasma concentration of amiodarone was delayed by >2 h in the probiotic pre-treated group. The plasma level of N-desethylamiodarone was unchanged in the probiotic pre-medicated group and its pharmacokinetic parameters were not altered.
Conclusions
The slower absorption of amiodarone in the probiotic pre-treated rats compared to the control ones and the unchanged pharmacokinetics of its main metabolite suggest that the probiotic strain of L. casei DN-114 001 has probably no clinical consequences as the difference was not statistically significant.


Similar content being viewed by others
References
Bailey DG, Malcolm J, Arnold O, Spence JD. Grapefruit juice-drug interactions. Brit J Clin Pharmacol. 1998;46:101–10.
Ernst E. Herb–drug interactions: potentially important but woefully under-researched. Eur J Clin Pharmacol. 2000;56(8):523–4.
Savai J, Varghese A, Pandita N, Chintamaneni M. Investigation of CYP3A4 nad CYP2D6 interactions of Withania somnifera and Centella asiatica in human liver microsomes. Phytother Res. 2015;29:785–90.
Zhao Y, Hellum BH, Liang A, Nilsen OG. Inhibitory mechanisms of human CYPs by three alkaloids isolated from traditional chinese herbs. Phytother Res. 2015;29:825–34.
Food and Agriculture Organization/World Health Organization (FAO/WHO). Guidelines for the evaluation of probiotics in food. FAO/WHO, London; 2002.
Al-Salami H, Butt G, Fawcett JP, Tucker IG, Golocorbin-Kon S, Mikov M. Probiotic treatment reduces blood glucose levels and increases systemic absorption of gliclazide in diabetic rats. Eur J Drug Metab Pharmacokinet. 2008;33(2):101–6.
Al-Salami H, Pharmacy PD, Butt G, Tucker I, Skrbic R, Golocorbin-Kon S, Pharmacy M, Mikov M. Probiotic pre-treatment reduces gliclazide permeation (ex vivo) in healthy rats but increases it in diabetic rats to the level seen in untreated healthy rats. Arch Drug Inf. 2008;1:35–41.
Pavlova I, Danova S, Naidenski H, Tropcheva R, Milanova A. Effect of probiotics on enrofloxacin disposition in gastrointestinal tract of poultry. J Vet Pharmacol Ther. 2015; 38(6):549–555.
Zimetbaum P, Kowey PR, Michelson EL. Antiarrhythmic drugs. In: Frishman WH, Sica DA, editors. Cardiovascular pharmacotherapeutics. 3rd ed. Minneapolis: Cardiotext Publishing, 2011. p. 227–56.
Naccarelli GV, Sager PT, Singh BN. Antiarrhythmic drugs. In: Podrid PJ, Kowey PR, editors. Cardiac arrhythmia: mechanisms, diagnostics, and management. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2001. p. 265–302.
Siddoway LA. Amiodarone: guidelines for use and monitoring. Am Fam Physician. 2003;68(11):2189–96.
Elsherbiny ME, El-Kadi AOS, Brocks DR. The metabolism of amiodarone by various CYP isoenzymes of human and rat, and the inhibitory influence of ketoconazole. J Pharm Pharm Sci. 2008;11(1):147–59.
Ohyama K, Nakajima M, Nakamura S, Shimada N, Yamazaki H, Yokoi T. A significant role of human cytochrome P450 2C8 in amiodarone N-deethylation: an approach to predict the contribution with relative activity factor. Drug Metab Dispos. 2000;28:1303–10.
Matuskova Z, Anzenbacherova E, Vecera R, Tlaskalova-Hogenova H, Kolar M, Anzenbacher P. Administration of a probiotic can change drug pharmacokinetics: effect of E. coli Nissle 1917 on amidarone absorption in rats. PLoS One. 2014;9(2):e87150.
Jun AS, Brocks DR. High-performance liquid chromatographic assay of amiodarone in rat plasma. J Pharm Sci. 2001;4(3):263–8.
Neely MN, van Guilder MG, Yamada WM, Schumitzky A, Jelliffe RW. Accurate detection of outliers and subpopulations with pmetrics, a nonparametric and parametric pharmacometric modeling and simulation package for R. Ther Drug Monit. 2012;34(4):467–76.
Chapot-Chartier M-P, Kulakauskas S. Cell wall structure and function in lactic acid bacteria. Microb Cell Fact. 2014;13[Suppl 1]:S9. doi:10.1186/1475-2859-13-S1-S9.
Saksena S, Goyal S, Raheja G, Singh V, Akhtar M, Nazir TM, Alrefai WA, Gill RK, Dudeja PK. Upregulation of P-glycoprotein by probiotics in intestinal epithelial cells and in the dextran sulfate sodium model of colitis in mice. Am J Physiol Gastrointest Liver Physio. 2011;300:G1115–23.
Stojančević M, Bojić G, Al-Salami H, Mikov M. The influence of intestinal tract and probiotics on the fate of orally administered drugs. Curr Issues Mol Biol. 2013;16:55–68.
Sharom FJ. The P-glycoprotein efflux pump: how does it transport drugs? J Membr Biol. 1997;160:161–75.
Silva R, Vilas-Boas V, Carmo H, Dinis-Oliveira RJ, Carvalho F, de Lourdes Bastos M, Remiäo F. Modulation of P-glycoprotein efflux pump: induction and activation as a therapeutic strategy. Pharmacol Ther. 2015;149:1–123.
Acknowledgments
Financial support from the Grant Agency of the Czech Republic P303/12/0535 to Pavel Anzenbacher, Eva Anzenbacherova, Zuzana Matuskova, and Helena Tlaskalova-Hogenova, as well as from the infrastructural projects NPU I (LO1304) and POSTUP II (CZ.1.07/2.3.00/30.0041) of the faculty, which enabled us to conduct the study described here, is gratefully acknowledged.
Compliance with Ethical Standards
All procedures performed in studies involving animals are in accordance with the ethical standards of the Czech Republic Act No. 359/2012 Coll. on the protection of animals and were approved by the Ethics Committee, Ministry of Education, Czech Republic.
Conflict of interest
All authors participating in this paper declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matuskova, Z., Anzenbacher, P., Vecera, R. et al. Effect of Lactobacillus casei on the Pharmacokinetics of Amiodarone in Male Wistar Rats. Eur J Drug Metab Pharmacokinet 42, 29–36 (2017). https://doi.org/10.1007/s13318-015-0315-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13318-015-0315-0