Abstract
Recent observations connected DNA cytosine deaminase APOBEC3B to the genetic evolution of breast cancer. We addressed whether APOBEC3B is associated with breast cancer clinical outcomes. APOBEC3B messenger RNA (mRNA) levels were related in 1,491 primary breast cancers to disease-free (DFS), metastasis-free (MFS), and overall survival (OS). For independent validation, APOBEC3B mRNA expression was associated with patient outcome data in five additional cohorts (over 3,500 breast cancer cases). In univariate Cox regression analysis, increasing APOBEC3B expression as a continuous variable was associated with worse DFS, MFS, and OS (hazard ratio [HR] = 1.20, 1.21, and 1.24, respectively; all P < .001). Also, in untreated ER-positive (ER+), but not in ER−, lymph-node-negative patients, high APOBEC3B levels were associated with a poor DFS (continuous variable: HR = 1.29, P = .001; dichotomized at the median level, HR = 1.66, P = .0002). This implies that APOBEC3B is a marker of pure prognosis in ER + disease. These findings were confirmed in the analyses of five independent patient sets. In these analyses, APOBEC3B expression dichotomized at the median level was associated with adverse outcomes (METABRIC discovery and validation, 788 and 706 ER + cases, disease-specific survival (DSS), HR = 1.77 and HR = 1.77, respectively, both P < .001; Affymetrix dataset, 754 ER + cases, DFS, HR = 1.57, P = 2.46E-04; NKI295, 181 ER + cases, DFS, HR = 1.72, P = .054; and BIG 1-98, 1,219 ER + cases, breast-cancer-free interval (BCFI), HR = 1.42, P = 0.0079). APOBEC3B is a marker of pure prognosis and poor outcomes for ER + breast cancer, which strongly suggests that genetic aberrations induced by APOBEC3B contribute to breast cancer progression.
Similar content being viewed by others
Introduction
Clinical heterogeneity is a confounding hallmark of breast cancer. This variation in disease manifestation, also true for many other cancers, is mirrored in the cancer genome with hundreds to thousands of somatic mutations in each tumor. The mutations involved are mostly base substitutions, but also include small insertions and deletions, larger-scale events such as translocations, and catastrophic events such as chromothripsis and kataegis [34, 4]. Several recent studies identified the APOBEC deaminase family as a major enzymatic source of somatic driver and passenger mutations in breast cancer. First, Sanger sequencing studies indicated a cytosine-biased mutation pattern dominated by C-to-T transition mutations [12, 33]. Second, next-generation full genome sequencing studies revealed strand-coordinated cytosine mutation clusters (called kataegis), consisting predominantly of C-to-T transitions and C-to-G transversions within 5′-TC dinucleotide motifs [20]. Third, the antiviral DNA cytosine deaminase apolipoprotein B messenger RNA (mRNA) editing enzyme catalytic polypeptide-like 3B (APOBEC3B) was shown to be overexpressed in cell lines and primary breast tumors and responsible for elevated levels of genomic uracil and mutations in cell lines. This correlated with increased mutational loads in primary tumors [2]. Fourth, APOBEC3B overexpression caused increased mutational loads, cell cycle deviations, induction of DNA damage markers, and ultimately cell death [2, 36, 30]. Finally, recent sequencing meta-analyses data have underscored the importance of APOBEC3B in causing both the dispersed and clustered mutations in breast cancer and also implicated it as a dominant mutagen in several additional cancers [3, 28, 1].
APOBEC3B is a member of a larger family of polynucleotide cytosine deaminases with diverse physiological functions in innate and adaptive immunity, lipid metabolism, and heart development [24, 7]. The APOBEC3 subfamily consists of seven members, APOBEC3A, APOBEC3B, APOBEC3C, APOBEC3D, APOBEC3F, APOBEC3G, and APOBEC3H [6, 16]. APOBEC family members are generally thought of as innate immune effectors with demonstrated single-stranded DNA cytosine to uracil (C-to-U) editing activity and the capacity to restrict the replication of a diverse array of transposons and viruses [11, 35]. APOBEC2 has not yet been demonstrated to elicit biochemical activity, but the mouse knockout suggests function in cardiovascular muscle development [38, 10, 29]. The family namesake, APOBEC1, is capable of editing both DNA and RNA cytosines, with a general role in innate immunity and a specialized role in APOB mRNA editing [24]. Finally, a last member of the APOBEC protein family, AID (activation-induced deaminase), is a DNA cytosine deaminase that targets rearranged immunoglobulin gene variables and switches region sequences to mediate the distinct processes of somatic hypermutation and class switch recombination, which are central to antibody affinity maturation and effector functions, respectively [9, 27].
As a potential continuous source of genetic aberrations in breast cancer, we hypothesized that APOBEC3B overexpression may accelerate cancer progression and lead to poor clinical outcomes. To test this hypothesis, we quantified APOBEC3B mRNA levels using reverse-transcriptase-quantitative PCR (RT-qPCR) in a large series of primary breast tumors and asked whether expression levels correlate with disease outcome. To probe the potential link between APOBEC3B mRNA levels and pure disease prognosis, i.e., to study the relation with the natural course of the disease, primary tumors of lymph-node-negative (LNN) breast cancer patients who did not receive systemic adjuvant therapy were evaluated separately. To provide independent validation, we analyzed five additional cohorts representing three distinct platforms (Illumina, Affymetrix, Agilent) for APOBEC3B mRNA expression measured by gene-specific probes and their association with patient outcome data. The combined results indicate that high levels of APOBEC3B mRNA expression are a significant prognostic biomarker of poor breast cancer outcomes, exclusively in cases with ER-positive primary disease.
Patients and Methods
RT-qPCR Cohort (or Rotterdam Cohort)
One thousand four hundred ninety-one tumor specimens obtained at primary surgery between 1978 and 2000 were selected from our liquid nitrogen tumor bank at the Erasmus MC (Rotterdam, Netherlands). Inclusion criteria were invasive breast cancer with freshly frozen tissue available irrespective of nodal status, tumor size, and type of adjuvant systemic therapy. Major details of this cohort have been described before [32], and patient and patho-clinical characteristics are presented in Table 1. Our institution’s Medical Ethical Committee approved our protocol for studying molecular markers associated with disease recurrence in anonymized tumor tissues (MEC 02 · 953). In this study, we adhere to the Code of Conduct of the Federation of Medical Scientific Societies in the Netherlands (http://www.fmwv.nl/) and report in accordance with the REMARK criteria on clinical reporting [19] (see Supplementary file and Diagram S1).
RNA Extraction, cDNA Synthesis, and Quantification by RT-qPCR
The detailed procedure for tissue processing, RNA extraction, cDNA synthesis and quantification of APOBEC3B mRNA transcripts by RT-qPCR has been described [31] (see supplement for detailed description).
Validation Cohorts
To validate our findings, we used five published datasets that contained both microarray and clinical follow-up data. In these data sets, different primary endpoints were reported, and various systemic adjuvant therapies were applied [8, 37, 13, 26].
The Illumina HT-12 v4 microarray data sets reported by Curtis et al. [8], consisting of two independent data sets, called METABRIC discovery (n = 997) and METABRIC validation (n = 995), were used. The METABRIC clinical data includes immunohistochemistry (IHC) ER status as well as disease-specific (DSS) survival data, where all reported deaths are attributed to breast cancer and deaths from other causes are censored. Here, we analyzed ER + samples to establish a METABRIC discovery ER + sub-cohort (n = 788, events = 218) and a METABRIC validation ER + sub-cohort (n = 706, events = 214). To determine APOBEC3B mRNA expression values, microarray probe expression values were used as published [8].
For the NKI295 microarray cohort, Agilent microarray probe mRNA expression values of APOBEC3B, and patient disease-free survival (DFS) of 181 ER + cases according to IHC, were taken from Van de Vijver et al. [37]. Also, here, microarray probe expression values were used as a measure of APOBEC3B mRNA expression value. Patients who had died without evidence of disease or who were lost during follow-up were censored at last follow-up in DFS analysis.
The Kaplan-Meier Plotter online service (http://kmplot.com) was used to asses APOBEC3B expression as a prognostic biomarker from Affymetrix microarrays manually curated and combined from publically available Gene Expression Omnibus (GEO) cohorts [13]. GEO cohorts overlapping with our Rotterdam cohort mentioned above were excluded. In total, the assembled Affymetrix microarray cohort included in the current study contains 754 ER + samples with DFS as outcome. Microarray probe expression values were used as downloaded from the kmplot web site.
BIG 1-98 was a prospective randomized, phase III, double-blind trial of 8,010 postmenopausal women with hormone-receptor-positive early breast cancer that compares 5 years of adjuvant tamoxifen or letrozole monotherapy or sequential treatment with 2 years of one of these agents followed by 3 years of the other between 1998 and 2003 [26]. Formalin-fixed, paraffin-embedded (FFPE) tissue samples (events = 257) were obtained. Due to overall low recurrence rates in BIG 1-98, a case-cohort sampling was used, where all cases (recurrences) with available RNA materials were included, while non-recurrence cases were sampled according to stratification factors. Included RNA samples were profiled using the Illumina Whole Genome DASL protocol on the Illumina HT-12 v4 microarray. Samples were cubic spline normalized with no background correction using BeadStudio software (Illumina). Twelve hundred nineteen samples were included in the analysis. The association of the expression data with time to disease recurrence (breast-cancer-free interval, BCFI) was assessed using a weighted analysis methods (generalized Horvitz-Thompson methods) to adjust estimates and test statistics to obtain unbiased analyses [28]. The endpoint BCFI was defined as the time from randomization to the first breast cancer event including invasive breast cancer recurrence at local, regional, or distant sites or a new invasive cancer in the contralateral breast, and ignored second (non-breast) malignancies, censored at death without a prior cancer event or last follow-up visit.
Statistical Analyses
Univariate and multivariate Cox regression analysis was used to assess the association of APOBEC3B mRNA expression levels and/or established clinical-pathological factors such as nodal status, age, tumor size, grade, and hormone receptor expression with DFS, metastasis-free survival (MFS), or overall survival (OS). The Cox proportional hazards model was used to calculate the hazard ratios (HRs) and their 95 % confidence intervals (95 % CIs) of covariates in the analyses of DFS, MFS, or OS. Likelihood ratio test was performed to test whether APOBEC3B mRNA expression or other covariates were related to the hazard. Survival curves were constructed from DFS, MFS, and OS data using the Kaplan-Meier estimator for survival [14]. Log-rank test was used to test for significant differences between two survival curves. All P values are two-sided. For the Rotterdam cohort, the STATA statistical package v.11 was used; for validation, Kaplan-Meier survival analysis BioJava was used which implements the R survival package [23] with the exception for the BIG 1-98 where a weighted analysis as described above was performed.
Results
Association of APOBEC3B mRNA Expression Levels with Patient and Clinical and Pathological Characteristics
APOBEC3B mRNA expression levels were quantified in the Rotterdam cohort (n = 1,491) by RT-qPCR of total RNA samples extracted from freshly frozen tumor tissues from patients with primary breast cancer [32]. The primers used here are new but robust because they showed near-identical specificity and efficiency in comparison to previously validated APOBEC3B RT-qPCR primers [25, 3] (Supplementary Fig. S1). In this cohort, mRNA expression of APOBEC3B was positively correlated with nodal status (P = .009), tumor size (P < .001), and grade (P < .001) and negatively with both ER (P < .001) and PR (P < .001) (Table 1).
Association of APOBEC3B mRNA Expression Levels with Clinical Outcomes
To determine whether APOBEC3B mRNA expression was associated with clinical outcome in breast cancer, we related log-transformed values of APOBEC3B using Cox regression analysis with DFS, MFS, and OS. This analysis, using data from all 1,491 patients, showed that higher expression levels of APOBEC3B mRNA as a continuous variable were associated with worse DFS, MFS, and OS (HR = 1.20, 95 % CI = 1.11–1.29; HR = 1.21, 95 % CI = 1.11–1.31; and HR = 1.24, 95 % CI = 1.13–1.36; all P < .001).
Because a percentage of patients from the Rotterdam cohort received adjuvant treatment, which may confound data analyses, we restricted subsequent analyses to the 829 patients with LNN disease who did not receive any (neo)adjuvant systemic therapy. Of note, this sub-cohort is relatively unbiased because patients with LNN disease at the time this retrospective cohort was collected (1978–2000) did not receive any (neo)adjuvant systemic therapy according to the guidelines in the Netherlands at that time. Thus, analysis of this sub-cohort allowed us to determine the association of APOBEC3B expression with the natural course of disease. The median mRNA expression level was used as an unbiased means to split the cohort into APOBEC3B-low and APOBEC3B-high expression groups. In addition, we stratified the cohort based on ER status because ER + (n = 633) and ER − (n = 196) breast cancers are biologically distinct diseases [22, 39].
In the 633 LNN patients with ER + disease, APOBEC3B mRNA expression split at the median level of the whole cohort was significantly associated with poor DFS (HR = 1.55, 95 % CI = 1.23–1.96, P < .001, Table 2), MFS (HR = 1.66, 95 % CI = 1.26–2.17, P < .001, Supplementary Table S2), and OS (HR = 1.68, 95 % CI = 1.25–2.24, P < .001 (Supplementary Table S3). In 196 LNN cases with ER − breast cancer, no significant association was observed with any of the endpoints. In multivariate Cox regression analysis, together with current prognostic markers such age, tumor size, and grade, steroid hormone receptors and APOBEC3B mRNA expression remained significant in ER + breast cancer in the analysis of DFS (HR = 1.32, 95 % CI = 1.02–1.69, P = .034, Table 2), MFS (HR = 1.43, 95 % CI = 1.07–1.91, P = .015, Supplementary Table S2), and OS (HR = 1.44, 95 % CI = 1.06–1.96, P = .02, Supplementary Table S3).
Kaplan-Meier analysis (Fig. 1) was used to visualize the difference in DFS, MFS, and OS of LNN patients with ER + disease as a function of low and high APOBEC3B mRNA expression levels. Patients whose tumors had high APOBEC3B mRNA expression levels clearly fared worse than those with low expression levels (log-rank P value < .001 for all three analyses).
Kaplan-Meier survival analysis for the Rotterdam cohort. Kaplan-Meier curves for disease-free survival (a), metastasis-free survival (b), and overall survival analysis (c) for all 633 lymph-node-negative patients with estrogen-receptor-positive disease who did not receive any adjuvant systemic therapy divided at the median APOBEC3B mRNA expression level. Red and blue graphs represent APOBEC3B mRNA expression below and above the median respectively. Y-axis expresses cumulative survival rate (Color figure online)
Corroborating Data from Independent Cohorts
To confirm the results presented above in independent patient cohorts, we used public data and a sub-selection of the recently profiled prospectively collected BIG 1-98 cohort (see the “Patients and Methods” section). The validation cohorts included the METABRIC discovery and validation cohorts [8], the NKI295 cohort in which the MammaPrint prognostic signature was validated [37], and other public data profiled on Affymetrix arrays and available via http://www.kmplot.com [13]. Note that, in contrast to the retrospectively collected LNN Rotterdam discovery cohort, part of these patients received (neo)adjuvant systemic therapy and that various primary endpoints were used in the analysis.
Before analyzing the expression of APOBEC3B using available gene datasets, the concordance between measuring APOBEC3B gene expression by RT-qPCR and the gene expression on U133A microarrays was assessed (Supplementary Fig. S2). For this, we had available from our cohort a total of 309 cases with both RT-qPCR and Affymetrix gene expression data from the same specimens. Overall, these independent quantitative measurements of APOBEC3B expression levels correlated strongly (Spearman r s = 0.87, P < .001) This reassured us that the Affymetrix probeset accurately quantifies APOBEC3B expression, thereby reassuring that publically available gene expression data can be used to help validate our findings.
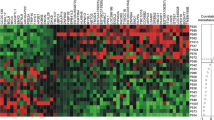
Retrospective analysis in five additional independent patient sets including one prospectively collected cohort of patients that received adjuvant therapy (BIG 1-98) confirmed the relation of APOBEC3B expression dichotomized at the median level with adverse outcome in ER + breast cancer (METABRIC discovery, 788 ER + cases OS, HR = 1.77, 95 % CI = 1.35–2.32, P < .0001; METABRIC validation, 706 ER + cases OS, HR = 1.77, 95 % CI = 1.34–2.33, P < .0001; NKI295, 181 ER + cases, HR = 1.72, 95 % CI = 0.98–3.02, P = .054; assembled Affymetrix microarray cohort, 754 ER + cases, DFS, HR = 1.57, 95 % CI = 1.23–2.01, P = .0002; and BIG 1-98, 1,219 ER + cases, BCFI, HR = 1.42, 95 % CI = 1.16–1.73, P = 0008). For the assembled Affymetrix microarray cohort, we further confirmed that APOBEC3B expression for ER − cases was not associated with outcome (122 cases, DFS, HR = 0.96, 95 % CI = 0.58–1.61, P = .89). Kaplan-Meier plots for the ER + cases of all five cohorts using the median APOBEC3B mRNA expression level as an unbiased cutoff are presented in Fig. 2.
Kaplan-Meier survival analysis of validation cohorts including only cases with estrogen-receptor-positive disease. Kaplan-Meier curves for DSS in the METABRIC discovery (a) and METABRIC validation cohort (b), for DFS in the NKI cohort (c) and for DFS in a combined cohort including publically available Affymetrix datasets (d), and for BCFI in the prospective collected BIG 1-98 cohort (e). All cohorts were divided using the median APOBEC3B mRNA expression level. Red and blue graphs represent APOBEC3B mRNA expression below and above the median respectively. Y-axis expresses cumulative survival rate (Color figure online)
Discussion
The innate immune DNA cytosine deaminase APOBEC3B was recently identified as a predominant source of context dependent cytosine base substitution mutations in breast cancer [12, 33, 2, 36, 30]. This exciting finding provided a rationale for the progressive gain of passenger and potentially also driver mutations over time. This consideration lets us hypothesize that levels of APOBEC3B might contribute to cancer progression as mutations acquired over time would likely be APOBEC3B level dependent. Our results indeed show that patients with high APOBEC3B mRNA levels in their primary tumor more rapidly experience disease relapse. This observation was made using a retrospective cohort of patients who did not receive any systemic (neo)adjuvant treatment, which suggests that APOBEC3B is indeed a marker of pure prognosis and a direct contributor to breast cancer progression. However, also in patients receiving various types of adjuvant endocrine and/or chemotherapy, the analysis came out as significant, suggesting that overall, the APOBEC3B enzyme contributes to breast cancer progression. The prognostic value of APOBEC3B was especially prominent in ER + disease, suggesting that particularly in this subclass of breast cancer levels of APOBEC3B may contribute to cancer progression. A clear negative link between ER and APOBEC3B expression suggests that estrogens down-regulate this gene. However, we found no evidence for such a regulation in multiple breast cancer cell lines (Burns, Leonard, and Harris, data not shown). Why APOBEC3B expression would only be prognostic in ER + and not in ER − breast cancer is unclear, especially because expression is higher in ER − disease. Possibly, the mutator phenotype induced by APOBEC3B overexpression is not rate limiting in ER − disease, a so called C class cancer, which is often high grade, TP53 mutant, and characterized by many copy number aberrations [5]. In line with this is our observation of a HR of 1.57 for APOBEC3B overexpression in luminal A breast cancer (Supplementary analysis), which is considered an M class cancer driven by mutations rather than copy number aberrations [5].
Earlier work analyzed the germline DNA of breast cancer cases versus healthy controls and reported that a deletion allele of APOBEC3B may be related to a higher incidence of developing breast cancer [15, 40, 18]. At first glance, this observation seems counterintuitive to the results presented here. However, incidence and progression are two clearly distinct issues. Higher incidence may be explained by the likelihood that APOBEC3B null cells are predicted to be more susceptible to viral infection and insertional mutagenesis by endogenous elements, which this protein normally serves to suppress. Our studies strongly suggest a direct role for APOBEC3B in cancer mutagenesis beyond tumor onset. Such a link with progression may also be relevant for other cancer types in which APOBEC3B is implicated in generating mutational diversity, such as bladder, lung, head and neck, and cervical cancer; however, this remains to be explored [3, 28].
Our work indicates that APOBEC3B and its associated mutator phenotype associate with poor prognosis. This result contrasts with the consequences of a different mutator phenotype in some colorectal cancers. The hereditary non-polyposis colorectal carcinoma (HNPCC) subclass of colorectal cancers typically has a germline mutation in a mismatch repair gene that results in a strong mutator phenotype (microsatellite instability) and is known to increase the incidence of cancer, but clinically results in better long-term prognosis. The main difference may be the overall level of mutation. HNPCC tumors may be more genetically “brittle” in that, while they are more likely to form, they are also unable to modulate the level of mutation once the tumor is established, making them susceptible to lethal hypermutation assisted by therapeutic intervention. HNPCC tumors cannot easily restore genetic stability because it is difficult to revert a chromosomal mutation (often germline). In contrast, APOBEC3B-elevated mutagenesis in breast cancer is more modest, appearing to occur gradually after the initial tumor has formed [40]. In our working model, the mutator phenotype provides cancer with a measure of sub-lethal genetic plasticity that contributes to diversifying the tumor cell population. Elevated APOBEC3B expression appears to be at the transcriptional level, which, depending on the tumor environment, may be up- or down-modulated. The heterogeneous population resulting from moderately elevated APOBEC3B expression may then yield more aggressive and drug resisting tumor cells that result in poor clinical outcomes.
Our data suggest that more aggressive treatments of ER + tumors could be considered particularly in those having high APOBEC3B. Long-lived APOBEC3B-high tumor cells, even when still dormant, will have more opportunities to accumulate mutations, evolve, escape the dormant state, outgrow, metastasize, and potentially acquire resistance during additional rounds of therapy. Stronger postoperative treatments to eradicate APOBEC3B-high, ER + cells may be effective. In addition, although still in the early stages of development [17, 21], small-molecule inhibition of APOBEC3B activity as a secondary adjuvant therapy is an attractive prospect.
References
Alexandrov LB, Nik-Zainal S, Wedge DC, Aparicio SA, Behjati S, Biankin AV, Bignell GR et al (2013) Signatures of mutational processes in human cancer. Nature 500(7463):415–421
Burns MB, Lackey L, Carpenter MA, Rathore A, Land AM, Leonard B, Refsland EW et al (2013) APOBEC3B is an enzymatic source of mutation in breast cancer. Nature 494(7437):366–370
Burns MB, Temiz NA, Harris RS (2013) Evidence for APOBEC3B mutagenesis in multiple human cancers. Nat Genet 45(9):977–983
Cancer Genome Atlas, Network (2012) Comprehensive molecular portraits of human breast tumours. Nature 490(7418):61–70
Ciriello G, Miller ML, Aksoy BA, Senbabaoglu Y, Schultz N, Sander C (2013) Emerging landscape of oncogenic signatures across human cancers. Nat Genet 45(10):1127–1133
Conticello SG (2008) The AID/APOBEC family of nucleic acid mutators. Genome Biol 9(6):229
Conticello SG (2012) Creative deaminases, self-inflicted damage, and genome evolution. Ann N Y Acad Sci 1267:79–85
Curtis C, Shah SP, Chin SF, Turashvili G, Rueda OM, Dunning MJ, Speed D et al (2012) The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 486(7403):346–352
Di Noia JM, Neuberger MS (2007) Molecular mechanisms of antibody somatic hypermutation. Annu Rev Biochem 76:1–22
Etard C, Roostalu U, Strahle U (2010) Lack of Apobec2-related proteins causes a dystrophic muscle phenotype in zebrafish embryos. J Cell Biol 189(3):527–539
Gotoh T, Aoyama K (1990) The method of total heminephroureterectomy–application of mucolysis. Nihon Hinyokika Gakkai Zasshi 81(1):14–18
Greenman C, Stephens P, Smith R, Dalgliesh GL, Hunter C, Bignell G, Davies H et al (2007) Patterns of somatic mutation in human cancer genomes. Nature 446(7132):153–158
Gyorffy B, Lanczky A, Szallasi Z (2012) Implementing an online tool for genome-wide validation of survival-associated biomarkers in ovarian-cancer using microarray data from 1287 patients. Endocr Relat Cancer 19(2):197–208
Kaplan EL, Meier P (1958) Non-parametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Komatsu A, Nagasaki K, Fujimori M, Amano J, Miki Y (2008) Identification of novel deletion polymorphisms in breast cancer. Int J Oncol 33(2):261–270
LaRue RS, Andresdottir V, Blanchard Y, Conticello SG, Derse D, Emerman M, Greene WC et al (2009) Guidelines for naming nonprimate APOBEC3 genes and proteins. J Virol 83(2):494–497
Li M, Shandilya SM, Carpenter MA, Rathore A, Brown WL, Perkins AL, Harki DA et al (2012) First-in-class small molecule inhibitors of the single-strand DNA cytosine deaminase APOBEC3G. ACS Chem Biol 7(3):506–517
Long J, Delahanty RJ, Li G, Gao YT, Lu W, Cai Q, Xiang YB et al (2013) A common deletion in the APOBEC3 genes and breast cancer risk. J Natl Cancer Inst 105(8):573–579
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM, N. C. I. EORTC Working Group on Cancer Diagnostics Statistics (2005) Reporting recommendations for tumor marker prognostic studies (REMARK). J Natl Cancer Inst 97(16)):1180–1184
Nik-Zainal S, Alexandrov LB, Wedge DC, Van Loo P, Greenman CD, Raine K, Jones D et al (2012) Mutational processes molding the genomes of 21 breast cancers. Cell 149(5):979–993
Olson ME, Li M, Harris RS, Harki DA (2013) Small-molecule APOBEC3G DNA cytosine deaminase inhibitors based on a 4-amino-1,2,4-triazole-3-thiol scaffold. ChemMedChem 8(1):112–117
Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR et al (2000) Molecular portraits of human breast tumours. Nature 406(6797):747–752
Prlic A, Yates A, Bliven SE, Rose PW, Jacobsen J, Troshin PV, Chapman M et al (2012) BioJava: an open-source framework for bioinformatics in 2012. Bioinformatics 28(20):2693–2695
Refsland EW, Harris RS (2013) The APOBEC3 family of retroelement restriction factors. Curr Top Microbiol Immunol 371:1–27
Refsland EW, Stenglein MD, Shindo K, Albin JS, Brown WL, Harris RS (2010) Quantitative profiling of the full APOBEC3 mRNA repertoire in lymphocytes and tissues: implications for HIV-1 restriction. Nucleic Acids Res 38(13):4274–4284
Regan MM, Neven P, Giobbie-Hurder A, Goldhirsch A, Ejlertsen B, Mauriac L, Forbes JF et al (2011) Assessment of letrozole and tamoxifen alone and in sequence for postmenopausal women with steroid hormone receptor-positive breast cancer: the BIG 1-98 randomised clinical trial at 8.1 years median follow-up. Lancet Oncol 12(12):1101–1108
Robbiani DF, Nussenzweig MC (2013) Chromosome translocation, B cell lymphoma, and activation-induced cytidine deaminase. Annu Rev Pathol 8:79–103
Roberts SA, Lawrence MS, Klimczak LJ, Grimm SA, Fargo D, Stojanov P, Kiezun A et al (2013) An APOBEC cytidine deaminase mutagenesis pattern is widespread in human cancers. Nat Genet 45(9):970–976
Sato Y, Probst HC, Tatsumi R, Ikeuchi Y, Neuberger MS, Rada C (2010) Deficiency in APOBEC2 leads to a shift in muscle fiber type, diminished body mass, and myopathy. J Biol Chem 285(10):7111–7118
Shinohara M, Io K, Shindo K, Matsui M, Sakamoto T, Tada K, Kobayashi M, Kadowaki N, Takaori-Kondo A (2012) APOBEC3B can impair genomic stability by inducing base substitutions in genomic DNA in human cells. Sci Rep 2:806
Sieuwerts AM, Meijer-van Gelder ME, Timmermans M, Trapman AM, Garcia RR, Arnold M, Goedheer AJ, Portengen H, Klijn JG, Foekens JA (2005) How ADAM-9 and ADAM-11 differentially from estrogen receptor predict response to tamoxifen treatment in patients with recurrent breast cancer: a retrospective study. Clin Cancer Res 11(20):7311–7321
Sieuwerts AM, Usher PA, Meijer-van Gelder ME, Timmermans M, Martens JW, Brunner N, Klijn JG, Offenberg H, Foekens JA (2007) Concentrations of TIMP1 mRNA splice variants and TIMP-1 protein are differentially associated with prognosis in primary breast cancer. Clin Chem 53(7):1280–1288
Stephens P, Edkins S, Davies H, Greenman C, Cox C, Hunter C, Bignell G et al (2005) A screen of the complete protein kinase gene family identifies diverse patterns of somatic mutations in human breast cancer. Nat Genet 37(6):590–592
Stephens PJ, McBride DJ, Lin ML, Varela I, Pleasance ED, Simpson JT, Stebbings LA et al (2009) Complex landscapes of somatic rearrangement in human breast cancer genomes. Nature 462(7276):1005–1010
Strebel K, Luban J, Jeang KT (2009) Human cellular restriction factors that target HIV-1 replication. BMC Med 7:48
Taylor BJ, Nik-Zainal S, Wu YL, Stebbings LA, Raine K, Campbell PJ, Rada C, Stratton MR, Neuberger MS (2013) DNA deaminases induce break-associated mutation showers with implication of APOBEC3B and 3A in breast cancer kataegis. Elife 2:e00534
van de Vijver MJ, He YD, van't Veer LJ, Dai H, Hart AA, Voskuil DW, Schreiber GJ et al (2002) A gene-expression signature as a predictor of survival in breast cancer. N Engl J Med 347(25):1999–2009
Vonica A, Rosa A, Arduini BL, Brivanlou AH (2011) APOBEC2, a selective inhibitor of TGFbeta signaling, regulates left-right axis specification during early embryogenesis. Dev Biol 350(1):13–23
Wang Y, Klijn JG, Zhang Y, Sieuwerts AM, Look MP, Yang F, Talantov D et al (2005) Gene-expression profiles to predict distant metastasis of lymph-node-negative primary breast cancer. Lancet 365(9460):671–679
Xuan D, Li G, Cai Q, Deming-Halverson S, Shrubsole MJ, Shu XO, Kelley MC, Zheng W, Long J (2013) APOBEC3 deletion polymorphism is associated with breast cancer risk among women of European ancestry. Carcinogenesis 34(10):2240–2243
Acknowledgments
Funding for the BIG 1-98 trial was provided by the International Breast Cancer Study Group through grants from Susan G. Komen for the Cure Promise Grant (KG080081) and United States National Cancer Institute (CA-75362). M.B.B. was supported by a Department of Defense Breast Cancer Research Program Predoctoral Fellowship (BC101124). Harris laboratory operational support for these studies was provided by a seed grant from the University of Minnesota Clinical and Translational Science Institute (supported by NIH 1UL1RR033183) and a Translational Research Grant from the Jimmy V Foundation. A.M.S. was supported by Cancer Genomics Netherlands funded by the Netherlands Organisation for Scientific Research (NWO).
Conflict of interest
R.S.H. is co-founder of ApoGen Biotechnologies L.L.C. None the other author have anything to disclaim.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 293 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Sieuwerts, A.M., Willis, S., Burns, M.B. et al. Elevated APOBEC3B Correlates with Poor Outcomes for Estrogen-Receptor-Positive Breast Cancers. HORM CANC 5, 405–413 (2014). https://doi.org/10.1007/s12672-014-0196-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12672-014-0196-8