Abstract
Purpose
Positional change can displace an endotracheal tube (ETT) and change the ETT cuff pressure in a tracheally intubated patient. Endotracheal tubes with different cuff shapes may lead to different cuff pressures after positional change. We hypothesized that the intracuff pressure in the TaperGuard™ ETT with a tapered-shaped cuff would be higher than that in the conventional ETT with a cylindrical-shaped cuff after a change from the supine to the lateral flank position.
Methods
Fifty-eight patients scheduled for open urological procedures in the lateral flank position were randomly allocated to receive either a TaperGuard ETT (group T) or conventional ETT (group C). The ETT cuff pressure was initially set at 20 cm H2O in the supine position and was measured after the change to the lateral flank position. The distance from the ETT tip to the carina was measured in both the supine and the lateral flank positions.
Results
Two patients, one from each group, were excluded from the data analysis. The mean (SD) ETT cuff pressure was significantly higher in group T (n = 28) than in group C (n = 28) after the change in position [31 (7) cm H2O vs 25 (4) cm H2O, respectively; mean difference, 6 cm; 95% confidence intervals [CI], 3 to 9; P < 0.001]. The mean (SD) proximal migration of the ETT tip was comparable between the two groups [8 (18) mm vs 4 (14) mm, respectively; P = 0.367].
Conclusions
After the change from the supine to the lateral flank position, the ETT cuff pressure was significantly higher in the TaperGuard ETT than in the conventional ETT, although the extent of cephalad displacement of the ETT was comparable between the two groups. This trial was registered at Clinicaltrials.gov: NCT02165319.
Résumé
Objectif
Les changements de position peuvent déplacer la sonde endotrachéale (SET) et modifier la pression du ballonnet de la SET chez un patient intubé par la trachée. Les sondes endotrachéales avec différentes formes de ballonnet peuvent entraîner des pressions de ballonnet différentes après un changement de position. Nous avons émis l’hypothèse que la pression à l’intérieur du ballonnet de la SET TaperGuard™, dont le ballonnet est conique, serait plus élevée que dans celui d’une SET traditionnelle, avec un ballonnet cylindrique, après un changement de position de décubitus dorsal à décubitus latéral.
Méthode
Cinquante-huit patients devant subir une intervention urologique ouverte en position latérale ont été aléatoirement attribués à être intubés à l’aide d’une SET TaperGuard (groupe T) ou d’une SET conventionnelle (groupe C). La pression de ballonnet de la SET a d’abord été réglée à 20 cm H2O en décubitus dorsal, puis mesurée après le déplacement en position latérale. La distance entre la pointe de la SET et la carène a été mesurée dans les deux positions.
Résultats
Deux patients, un dans chaque groupe, ont été exclus de l’analyse de données. La pression du ballonnet de la SET moyenne (ÉT) était significativement plus élevée dans le groupe T (n = 28) que dans le groupe C (n = 28) après le changement de position [31 (7) cm H2O vs 25 (4) cm H2O, respectivement; différence moyenne, 6 cm; intervalles de confiance (IC) 95 %, 3 à 9; P < 0,001]. La migration proximale moyenne (ÉT) de la pointe de la SET était comparable dans les deux groupes [8 (18) mm vs 4 (14) mm, respectivement; P = 0,367].
Conclusion
Après le changement de décubitus dorsal à une position latérale, la pression de ballonnet de la SET était significativement plus élevée avec la SET TaperGuard qu’avec la SET traditionnelle, bien que l’ampleur du déplacement vers la tête de la SET ait été comparable entre les deux groupes. Cette étude est enregistrée au ClinicalTrials.gov: NCT02165319.
Similar content being viewed by others
Maintaining an endotracheal tube (ETT) cuff pressure of 20-30 cm H2O is important to prevent cuff-related complications in a tracheally intubated patient.1-3 A cuff pressure of more than 30 cm H2O is known to cause obstruction to mucosal blood flow in the trachea.4 Partial denuding of the basement membrane was found at an ETT cuff pressure over 50 cm H2O.4 An increase in the ETT cuff pressure is associated with increased postoperative complications such as postoperative sore throat and hoarseness.2,5,6 The intracuff pressure can be affected by various factors, including environmental factors (e.g., intraoperative use of high airway pressure and nitrous oxide), patient factors (e.g., differences in the size of the trachea and the position of the intratracheal cuff), and cuff-related factors (e.g., differences in cuff compliance and diameter).7-10
Positional change and neck movement after intubation can displace an ETT in a patient’s trachea.11-18 Intratracheal migration of the ETT due to a change in patient positioning can result in a change in the ETT cuff pressure because the trachea is not cylindrical.19-22 When the ETT migrates proximally toward the vocal cords, the cuff shape may be distorted and the intracuff volume may be compressed at a narrower and less compliant upper airway space such as at the level of the cricoid cartilage. The lateral flank position combines the lateral decubitus position and flexion at the level of the umbilicus.23 The position is usually used for renal surgery such as nephrolithotomy or open nephrectomy. Investigations are currently lacking on the extent of ETT displacement and its effect on the ETT cuff pressure after a change to the lateral flank position.
The shape of the ETT cuff may affect the cuff pressure.9 A conventional ETT has a cylindrical cuff, whereas the shape of the TaperGuard™ ETT (Covidien, Athlone, Ireland) cuff tapers distally to reduce microaspiration and ventilator-associated pneumonia.24,25 The objective of our prospective randomized study was to compare the ETT cuff pressure in the TaperGuard ETT vs the conventional ETT after a change from the supine to the lateral flank position. Because of the difference in proximal intracuff width between the two ETTs, we expected that the TaperGuard ETT cuff would be more compressed at the narrow upper airway than the conventional high-volume low-pressure (HVLP) ETT cuff.
Additionally, we compared the extent of intratracheal ETT displacement by measuring the distance from the carina to the ETT tip, and we followed patients for the occurrence of postoperative airway complications. We hypothesized that the cuff pressure of both ETTs would increase after changing from the supine to the lateral flank position and that the increase in cuff pressure would be higher in the TaperGuard ETT than in the conventional ETT.
Methods
The Institutional Review Board of Seoul National University Hospital, Seoul, Korea approved this study (document number: H1405-090-576) on June 19, 2014 before the patients were enrolled. After providing written informed consent, patients scheduled for open radical nephrectomy, partial nephrectomy, or nephroureterectomy in the lateral flank position were enrolled from June 2014 to September 2014. Patients with American Society of Anesthesiologists’ physical status I-III and aged 18-80 yr were included. Patients with a history of difficult intubation and neck surgery or previous irradiation treatment of the head and/or neck were excluded. Those with limited neck movement, neck pain, poor dentition, and morbid obesity (body mass index > 40 kg·m−2) were also excluded.
For this single-blinded study, we used a parallel design with an allocation ratio of 1:1, and the data were collected in Seoul National University Hospital, Seoul, Korea. Patients were randomized into two groups, tracheal intubation with the TaperGuard ETT (group T) or tracheal intubation with a conventional ETT (Unomedical, Kedah, Malaysia) (group C) using a computer-generated randomization program accessed only by an anesthesia nurse. The randomization sequencing was performed using a mixture of blocks in sizes four and six. The assignments were concealed in envelopes and were managed by the anesthesia nurses who were not involved in the perioperative care. The group assignments were announced to the attending anesthesiologist before the surgery.
Patients arrived in the operating room without premedication. They were monitored with standard monitoring devices such as noninvasive arterial blood pressure, pulse oximetry, and three-lead electrocardiography. The patient’s head was positioned on a 6-cm high headrest. A bolus of propofol 2 mg·kg−1 and a target-controlled continuous infusion of remifentanil 4 ng·mL−1 (Orchestra® Base Primea; Fresenius Kabi, Brezins, France) were administered to induce anesthesia. Intravenous rocuronium 0.8 mg·kg−1 was injected to facilitate tracheal intubation. An ETT with a 7.5-mm internal diameter was used for male patients and an ETT with a 7.0-mm internal diameter was used for female patients. The ETT was inserted so that the vocal cords were located between the two black marks on the tube shaft, and tracheal intubation was confirmed by capnography. A catheter was inserted into the radial artery for invasive arterial monitoring. Desflurane inhalation and remifentanil continuous infusion were used for anesthetic maintenance. Neuromuscular monitoring was carried out at the adductor pollicis muscle in response to ulnar nerve stimulation. Additional doses of rocuronium 0.2 mg·kg−1 were administered to maintain a train-of-four count of 1 during the surgical procedure. Volume-controlled ventilation with a tidal volume of 8 mL·kg−1 predicted body weight and positive end-expiratory pressure of 5 cm H2O were applied to all patients.
The ETT was secured at the right corner of the patient’s mouth with tape. The ETT cuff was inflated with air, and the cuff pressure was set initially at 20 cm H2O without air leakage.1,2,8,26,27 The volume of air supplied to attain the cuff pressure of 20 cm H2O was noted. The pressure was measured during an end-expiratory hold using a calibrated cuff manometer (Portex, Smiths Medical, Germany). The fractional inspired oxygen concentration remained at 1.0 throughout the investigation to prevent any desaturation. Nitrous oxide was not used in either group. After the cuff pressure was set, a single investigator measured the distance from the ETT tip to the carina at the end of expiration by performing the drawback technique by Weiss et al. 28 using a fibreoptic bronchoscope (FOB) with a 5-mm outer diameter (Olympus, Tokyo, Japan). During the measurements, 100% oxygen was supplied. The drawback technique was performed as follows: (1) When the carina was just visualized at the tip of the FOB, the first clip was placed on the shaft of the FOB at the level of the elbow connector; (2) The FOB was then withdrawn until the tip of the ETT was just visualized; (3) The second clip was placed on the shaft of the FOB using the same method as for the first clip; (4) The distance between the first and second clip was measured.
Positional change from the supine position to the lateral flank position was achieved as follows: (1) The patient was positioned laterally at 90°; (2) The kidney rest was inserted; (3) Flexion at the level of the umbilicus was performed. During the positional change, the ETT was secured by the attending anesthesiologist. The patient’s head position was kept neutral by adjusting the height of the headrest. After the positional change, the cuff pressure was recorded and readjusted to 20 cm H2O. The distance from the carina to the ETT tip was measured again using the same technique. The attending anesthesiologist performed ETT repositioning if an inadvertent endobronchial intubation or unplanned extubation was detected while using a FOB with the patient in the supine or lateral flank position.
The incidence and severity of postoperative sore throat, hoarseness, dysphagia, and cough were recorded as none, mild, moderate, or severe at zero, six, 12, and 24 hr postoperatively by an anesthesiology resident who was blinded to the group assignment. Additionally, the overall incidence of postoperative airway complications during the postoperative 24 hr was noted.
The primary endpoint was the cuff pressure after the positional change from the supine to the lateral flank position. Secondary endpoints were the distance from the carina to the ETT tip and the incidence and severity of postoperative airway complications.
Sample size calculation and statistical analysis
According to a previous study,26 the mean (SD) TaperGuard ETT cuff pressure was increased by 6.5 (3.9) cm H2O after the positional change from the supine to the lateral decubitus position. Assuming that the difference in the mean cuff pressure between the two ETTs is reduced by 50% (3.25 cm H2O), we calculated that 23 patients would be needed in each group with α = 0.05 and β = 0.20. Considering a 20% dropout rate, 29 patients per group were included. Statistical analysis was performed using SPSS® ver. 19.0 (SPSS, Inc., Chicago, IL, USA). The sample size calculation was performed using G*Power 3 software, (Heinrich-Heine University, Dusseldorf, Germany).29
After the change from the supine to the lateral flank position, the cuff pressure and the distance from the carina to the ETT were compared using the Student’s t test. The overall incidence of postoperative sore throat, hoarseness, dysphagia, and cough was compared using Fisher’s exact test. All reported P values are two sided. The severity of postoperative sore throat at each time point was compared by the Mann-Whitney U test with a P value adjustment (P < 0.012) to compensate for multiple comparisons.
Results
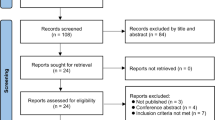
Sixty patients scheduled for open nephrectomy in the lateral flank position were enrolled. Two patients were excluded from the study (one patient met the exclusion criteria, and one refused to participate). Of the 58 patients recruited, 29 were randomized to group T and 29 to group C (Fig. 1); however, one patient in group T did not receive the intervention because of cancelled surgery, and one patient in group C withdrew from the study. Preoperative patient characteristics, ventilator settings, surgical type and time, Cormack-Lehane grade, and intubation times were comparable between the two groups (Table 1). Group T had more men (64%) than group C (39%), and correspondingly, group T had more participants managed with the larger size ETT.
The mean (SD) volume of air given to attain the ETT cuff pressure of 20 cm H2O was higher in group T than in group C [10.2 (0.4) mL vs 9.3 (0.4) mL, respectively; P < 0.001]. After the positional change from the supine to the lateral flank position, the mean (SD) ETT cuff pressure was significantly higher in group T than in group C [31 (7) cm H2O vs 25 (4) cm H2O, respectively; mean difference, 6 cm; 95% confidence intervals [CI], 3 to 9; P < 0.001] (Fig. 2). The number of patients showing a cuff pressure more than 30 cm H2O was higher in group T than in group C (15 [54%] vs 2 [7%], respectively; P < 0.001) (Table 2).
The endotracheal tube cuff pressure after changing from the supine to the lateral flank position. Group C = the conventional endotracheal tube is inserted; Group T = the TaperGuard™ endotracheal tube is inserted. The box represents the interquartile range, and a line across the box represents the median. The bars located in the top and bottom indicate the maximum and minimum values, respectively. * P < 0.001 vs group C
The extent of ETT tip displacement after the positional change from the supine position to the lateral flank position is shown in Fig. 3. The mean (SD) proximal migration of the ETT tip was 8 (18) mm in group T and 4 (14) mm in group C (P = 0.367) (Table 2). The ETT tip moved away from the carina in 21 (75%) patients in group T and in 18 (64%) patients in group C, respectively; P = 0.562. An ETT displacement > 10 mm occurred in 18 (64%) patients in group T and in 16 (57%) patients in group C (P = 0.785). In one patient in group C, the ETT needed repositioning because of endobronchial intubation. No patient in either group showed unintended extubation.
Displacement of the endotracheal tube tip after changing from the supine to the lateral flank position. The vertical axis represents the distance from the carina to the endotracheal tube (ETT) tip, in each position, for each ETT. Group C = the conventional endotracheal tube is inserted; Group T = the TaperGuard™ endotracheal tube is inserted. The extent of displacement of the endotracheal tube is comparable between the two groups. The box represents the interquartile range and a line across the box represents the median. The bars located in the top and bottom indicate the maximum and minimum values, respectively
The severity (none/mild/moderate/severe) of postoperative sore throat at the designated postoperative time points was comparable between group T and group C, respectively: time zero (24/1/2/1 vs 20/1/6/1), six hours (18/7/3/0 vs 19/6/3/0), 12 hr (20/6/2/0 vs 20/7/1/0), and 24 hr (23/5/0/0 vs 23/5/0/0). The overall incidence of postoperative airway complications during the postoperative 24 hr was comparable between group T and group C, respectively: sore throat (10 [36%] vs 12 [43%]), hoarseness (12 [43%] vs 12 [43%]), dysphagia (3 [11%] vs 6 [21%]), and cough (1 [4%] vs 0 [0%]).
Discussion
After a positional change from the supine to the lateral flank position, we showed that the cuff pressure was higher in the TaperGuard ETT than in the conventional ETT. The extent of cephalad displacement of the ETT was comparable between both ETTs after the position change.
Endotracheal tubes with different cuff shapes may lead to different cuff pressures after a position change. Results of this novel investigation showed a significantly greater increase in cuff pressure in the TaperGuard ETT than in the conventional HVLP ETT. Since there was no difference in tube migration and the ETT cuffs were considered to have similar compliance, the geometry of the ETT cuff may account for the differing cuff pressures. In the current study, the cuff pressure was significantly higher in the lateral flank position than in the supine position irrespective of the ETT type used. Such an increase in intratracheal cuff pressure after the positional change from the supine to the lateral flank position can be explained in part by displacement of the ETT. When proximal migration of the ETT occurs and the ETT cuff is placed adjacent to less compliant airway structures, such as the cricoid cartilage, the cuff volume is compressed, and the cuff pressure is elevated. This exemplifies Boyle’s law, i.e., at a constant temperature, the pressure of a gas is inversely proportional to volume. Endotracheal tube migration, either proximally or distally, can occur when a patient is repositioned; therefore, the ETT depth should be reassessed promptly after a change in patient position. In addition, ETT migration may result in a change in cuff pressure. This is seen regardless of the cuff design. Clinicians should ensure that the ETT cuff volume/pressure does not cause inspiratory leak or compromise tracheal mucosal blood flow.
A cuff pressure ranging from 20-30 cm H2O is recommended to prevent cuff-related complications such as ventilator-associated pneumonia and tracheal injury in patients receiving prolonged ventilatory care in the intensive care unit.1,3 In cases of short surgical procedures, the relatively high cuff pressure of the ETT also results in postoperative cuff-related complications, including sore throat, cough, and hoarseness.2 In the present study, the average cuff pressure was 31 cm H2O, and 54% of patients who received tracheal intubation with the TaperGuard ETT showed a cuff pressure > 30 cm H2O after the change to the lateral flank position. When the ETT cuff pressure reaches 30 cm H2O, blood flow in the tracheal mucosa begins to decrease.2,26 Moreover, one case in group T showed a cuff pressure of 60 cm H2O, an amount that is known to block the circulation of the trachea completely.4 Tracheal mucosal blood flow can be influenced by various factors such as perfusion pressure and vasomotor status. To prevent a decrease in tracheal mucosal blood flow, intraoperative blood pressure should be cautiously monitored, because intraoperative hypotension can impair tracheal mucosal blood flow by reducing perfusion pressure.
In this study, proximal migration of the ETT occurred in about 70% of patients after the positional change from the supine to the lateral flank position, and the ETT tip advanced toward the carina in 29% of patients. The extent of ETT withdrawal was comparable between the two ETTs used in this study. In general, it is well known that various positional changes and head movements can displace the ETT tube in tracheally intubated patients.11-17 Head extension can result in cephalad migration of the ETT, whereas head flexion can result in caudal displacement.12,18 Lateral rotation of the head can cause movement of the ETT tip in both directions.12 In this study, alterations in head position, such as extension and/or rotation, may be responsible in part for ETT tip migration from the carina after the change to the lateral flank position. By contrast, the slight head-down tilt position at the flank level, a component of the lateral flank position, may partly contribute to ETT movement toward the carina. The head-down tilt position can result in ETT advancement toward the carina by decreasing the distance from carina to tube tip.14,16,17
In this study, the incidences of postoperative sore throat, hoarseness, dysphagia, and cough were comparable between the two groups. Although the cuff pressure in group T was significantly elevated in the lateral flank position, in our study protocol, the increased cuff pressure was adjusted to 20 cm H2O and maintained throughout the surgical procedure. This adjustment of the cuff pressure can partly explain why there was no significant difference in the incidence of postoperative airway complications between the two groups. Nevertheless, our results regarding the incidence of postoperative airway morbidity should be interpreted cautiously because this study was not powered to detect a difference in airway morbidities. Further research is needed to examine the association between postoperative airway morbidity and the shape of the ETT cuff.
This study had several limitations. First, it was impossible to blind the attending anesthesiologist to group assignment, a situation that may be a source of bias. Second, the postoperative sore throat evaluated in this study is a subjective symptom. We did not evaluate actual injury to the trachea by direct visualization or histology. Moreover, the comparison between the two ETTs regarding potential postoperative airway complications was restricted because of the readjustments to the cuff pressure. Third, pulmonary complications such as atelectasis, pneumonia, and hypoxemia were not investigated; therefore, the association between the intraoperative ETT cuff pressure and pulmonary complications is not known. Fourth, this study was conducted in an only Asian population; therefore, there may be a limitation in extrapolating our results to other ethnic populations because of potential differences in airway anatomy between races. A recent study indicated that the intraluminal dimensions of the subglottis and upper trachea differed between Indian and Western populations.30 Also, a previous study showed that obstructive sleep apnea syndrome developed at a lower body mass index level in Asian populations than in Western populations because of Asian cephalometric characteristics such as a smaller maxilla and mandible, retrognathia, and a shorter and steeper anterior cranial base.31 Finally, all subjects in our study underwent open renal surgery. Because patients undergoing laparoscopic- or robotic-assisted renal surgery were excluded, the effect of pneumoperitoneum on tube displacement and change in cuff pressure was not investigated in our study.
In conclusion, after the change from the supine to the lateral flank position, the tip of both the TaperGuard and the conventional ETTs moved cephalad and cuff pressure increased in the majority of cases. The increase in cuff pressure was more dramatic in the TaperGuard ETT than in the conventional ETT, suggesting the need to monitor cuff pressure after positional change, irrespective of the shape of the ETT cuff.
References
American Thoracic Society, Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005; 171: 388-416.
Liu J, Zhang X, Gong W, et al. Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicenter study. Anesth Analg 2010; 111: 1133-7.
Lorente L, Blot S, Rello J. Evidence on measures for the prevention of ventilator-associated pneumonia. Eur Respir J 2007; 30: 1193-207.
Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Br Med J (Clin Res Ed) 1984; 288: 965-8.
Geng G, Hu J, Huang S. The effect of endotracheal tube cuff pressure change during gynecological laparoscopic surgery on postoperative sore throat: a control study. J Clin Monit Comput 2015; 29: 141-4.
Yildirim ZB, Uzunkoy A, Cigdem A, Ganidagli S, Ozgonul A. Changes in cuff pressure of endotracheal tube during laparoscopic and open abdominal surgery. Surg Endosc 2012; 26: 398-401.
Tsuboi S, Miyashita T, Yamaguchi Y, Yamamoto Y, Sakamaki K, Goto T. The TaperGuard™ endotracheal tube intracuff pressure increase is less than that of the Hi-Lo™ tube during nitrous oxide exposure: a model trachea study. Anesth Analg 2013; 116: 609-12.
Combes X, Schauvliege F, Peyrouset O, et al. Intracuff pressure and tracheal morbidity: influence of filling with saline during nitrous oxide anesthesia. Anesthesiology 2001; 95: 1120-4.
Bernhard WN, Yost L, Joynes D, Cothalis S, Turndorf H. Intracuff pressures in endotracheal and tracheostomy tubes. Related cuff physical characteristics. Chest 1985; 87: 720-5.
Guyton D, Banner MJ, Kirby RR. High-volume, low-pressure cuffs. Are they always low pressure? Chest 1991; 100: 1076-81.
Wu CY, Yeh YC, Wang MC, Lai CH, Fan SZ. Changes in endotracheal tube cuff pressure during laparoscopic surgery in head-up or head-down position. BMC Anesthesiol 2014; 14: 75.
Kim JT, Kim HJ, Ahn W, et al. Head rotation, flexion, and extension alter endotracheal tube position in adults and children. Can J Anesth 2009; 56: 751-6.
Minonishi T, Kinoshita H, Hirayama M, et al. The supine-to-prone position change induces modification of endotracheal tube cuff pressure accompanied by tube displacement. J Clin Anesth 2013; 25: 28-31.
Ezri T, Hazin V, Warters D, Szmuk P, Weinbroum AA. The endotracheal tube moves more often in obese patients undergoing laparoscopy compared with open abdominal surgery. Anesth Analg 2003; 96: 278-82.
Rigini N, Boaz M, Ezri T, et al. Prompt correction of endotracheal tube positioning after intubation prevents further inappropriate positions. J Clin Anesth 2011; 23: 367-71.
Kim JH, Hong DM, Oh AY, Han SH. Tracheal shortening during laparoscopic gynecologic surgery. Acta Anaesthesiol Scand 2007; 51: 235-8.
Chang CH, Lee HK, Nam SH. The displacement of the tracheal tube during robot-assisted radical prostatectomy. Eur J Anaesthesiol 2010; 27: 478-80.
Kim D, Jeon B, Son JS, Lee JR, Ko S, Lim H. The changes of endotracheal tube cuff pressure by the position changes from supine to prone and the flexion and extension of head. Korean J Anesthesiol 2015; 68: 27-31.
Vock P, Spiegel T, Fram EK, Effmann EL. CT assessment of the adult intrathoracic cross section of the trachea. J Comput Assist Tomogr 1984; 8: 1076-82.
Otoch JP, Minamoto H, Perini M, Carneiro FO, de Almeida Artifon EL. Is there a correlation between right bronchus length and diameter with age? J Thorac Dis 2013; 5: 306-9.
Abramson ZR, Susarla S, Tagoni JR, Kaban L. Three-dimensional computed tomographic analysis of airway anatomy. J Oral Maxillofac Surg 2010; 68: 363-71.
Brown BM, Oshita AK, Castellino RA. CT assessment of the adult extrathoracic trachea. J Comput Assist Tomogr 1983; 7: 415-8.
Altinel M, Akinci S, Gunes ZE, Olcucuoglu E, Gonenc F, Yazicioglu AH. Open versus laparoscopic donor nephrectomy: perioperative parameters and graft functions. Transplant Proc 2011; 43: 781-6.
Dave MH, Frotzler A, Spielmann N, Madjdpour C, Weiss M. Effect of tracheal tube cuff shape on fluid leakage across the cuff: an in vitro study. Br J Anaesth 2010; 105: 538-43.
Zanella A, Scaravilli V, Isgro S, et al. Fluid leakage across tracheal tube cuff, effect of different cuff material, shape, and positive expiratory pressure: a bench-top study. Intensive Care Med 2011; 37: 343-7.
Lizy C, Swinnen W, Labeau S, et al. Cuff pressure of endotracheal tubes after changes in body position in critically ill patients treated with mechanical ventilation. Am J Crit Care 2014; 23: e1-8.
Ryu JH, Han SS, Do SH, Lee JM, Lee SC, Choi ES. Effect of adjusted cuff pressure of endotracheal tube during thyroidectomy on postoperative airway complications: prospective, randomized, and controlled trial. World J Surg 2013; 37: 786-91.
Weiss M, Gerber AC, Dullenkopf A. Appropriate placement of intubation depth marks in a new cuffed paediatric tracheal tube. Br J Anaesth 2005; 94: 80-7.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007; 39: 175-91.
Prasanna Kumar S, Ravikumar A. Biometric study of the internal dimensions of subglottis and upper trachea in adult Indian population. Indian J Otolaryngol Head Neck Surg 2014; 66(Suppl 1): 261-6.
Lee RW, Vasudavan S, Hui DS, et al. Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep 2010; 33: 1075-80.
Acknowledgement
The authors sincerely thank Dr. Jung-Su Kim for his help with data collection.
Funding
None.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Hyun-Chang Kim, Yong-Hun Lee, Eugene Kim, and Eun-Ah Oh helped collect the data. Hyun-Chang Kim and Hee-Pyoung Park helped analyze the data and write the manuscript. Hyun-Chang Kim, Yong-Hun Lee, Eugene Kim, Eun-Ah Oh, Young-Tae Jeon, and Hee-Pyoung Park helped design the study.
Rights and permissions
About this article
Cite this article
Kim, HC., Lee, YH., Kim, E. et al. Comparison of the endotracheal tube cuff pressure between a tapered- versus a cylindrical-shaped cuff after changing from the supine to the lateral flank position. Can J Anesth/J Can Anesth 62, 1063–1070 (2015). https://doi.org/10.1007/s12630-015-0394-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-015-0394-z