Abstract
Purpose
Successful resuscitation of a pregnant woman undergoing cardiac arrest and survival of the fetus require prompt, high-quality cardiopulmonary resuscitation. The objective of this observational study was to assess management of maternal cardiac arrest by anesthesia residents using high-fidelity simulation and compare subsequent performance following either didactic teaching or electronic learning (e-learning).
Methods
Twenty anesthesia residents were randomized to receive either didactic teaching (Didactic group, n = 10) or e-learning (Electronic group, n = 10) on maternal cardiac arrest. Baseline management skills were tested using high-fidelity simulation, with repeat simulation testing one month after their teaching intervention. The time from cardiac arrest to start of perimortem Cesarean delivery (PMCD) was measured, and the technical and nontechnical skills scores between the two teaching groups were compared.
Results
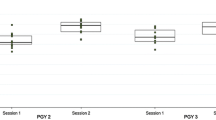
The median [interquartile range] time to PMCD decreased after teaching, from 4.5 min [3.4 to 5.1 min] to 3.5 min [2.5 to 4.0 min] (P = 0.03), although the change within each group was not statistically significant (Didactic group 4.9 to 3.8 min, P = 0.2; Electronic group 3.9 to 2.5 min, P = 0.07; Didactic group vs Electronic group, P = 1.0). Even after teaching, only 65% of participants started PMCD within four minutes. Technical and nontechnical skills scores improved after teaching in both groups, and there were no differences between the groups.
Conclusion
There are gaps in the knowledge and implementation of resuscitation protocols and the recommended modifications for pregnancy among residents. Teaching can improve performance during management of maternal cardiac arrest. Electronic learning and didactic teaching offer similar benefits.
Résumé
Objectif
La réanimation réussie d’une femme enceinte victime d’un arrêt cardiaque et la survie du fœtus nécessitent une réanimation cardiopulmonaire rapide et de grande qualité. L’objectif de cette étude observationnelle était d’évaluer la prise en charge d’un arrêt cardiaque maternel par des résidents en anesthésie utilisant une simulation à haute fidélité et de comparer leurs performances après un enseignement didactique ou un apprentissage électronique (formation en ligne).
Méthodes
Vingt résidents en anesthésie ont été répartis de façon aléatoire dans deux groupes : le premier a suivi un enseignement didactique (Groupe didactique, n = 10) et le second, une formation en ligne (Groupe électronique, n = 10) sur l’arrêt cardiaque maternel. Les compétences initiales de prise en charge ont été testées à l’aide d’une simulation à haute fidélité et le test de simulation a été répété un mois après l’intervention d’enseignement. Le délai écoulé entre l’arrêt cardiaque et l’accouchement par césarienne perimortem (PMCD) a été chronométré et les scores de compétences techniques entre les deux groupes d’enseignement ont été comparés.
Résultats
Le délai médian [écart interquartile] jusqu’au PMCD a diminué après l’enseignement de 4,5 min [3,4 à 5,1] à 3,5 min [2,5 à 4], P = 0,03), bien que la variation à l’intérieur de chaque groupe n’ait pas été significative (groupe didactique: 4,9 à 3,8 min, P = 0,2; groupe électronique: 3,9 à 2,5 min, P = 0,07; groupe didactique contre groupe électronique, P = 1,0). Même après l’enseignement, seulement 65 % des participants ont commencé le PMCD dans un délai de quatre minutes. Les scores techniques et non techniques ont été améliorés après enseignement dans les deux groupes, et aucune différence n’a été trouvée entre les groupes.
Conclusion
Il existe des lacunes chez nos résidents quant aux connaissances et à la mise en œuvre des protocoles de réanimation, ainsi que dans les modifications recommandées dans le cadre de la grossesse. L’enseignement peut améliorer la performance pour la prise en charge de l’arrêt cardiaque maternel. La formation en ligne et l’enseignement didactique ont, tous deux, des avantages comparables.
Similar content being viewed by others
Maternal cardiac arrest during pregnancy is rare, with one case for every 20,000–30,000 pregnancies.1,2 Successful resuscitation of a pregnant woman and survival of the fetus require prompt, high-quality cardiopulmonary resuscitation (CPR) with some modifications in basic and advanced cardiovascular life support techniques as they apply to pregnancy.3,4 The term “perimortem Cesarean delivery” (PMCD) refers to a Cesarean delivery concurrent with maternal CPR.5
Katz et al. originally recommended that PMCD be performed within four minutes of maternal cardiac arrest and delivery of the infant by five minutes.5 A subsequent review of published cases from 1985 to 2004 identified 38 cases of PMCD.6 Of the 22 cases where information regarding maternal hemodynamics was provided, 12 women had sudden, often profound improvement following delivery of the fetus. For surviving infants, there was a suggestion that those delivered within five minutes had a lower incidence of neurological and respiratory sequelae. Consequently, the authors concluded that PMCD within four minutes of maternal cardiac arrest improves maternal and neonatal outcomes. However, these times are “an extremely tall order that is made more challenging as maternal cardiac arrest is rare and frequently unexpected.”7 Furthermore, the 2003–2005 Confidential Enquiry into Maternal and Child Health (CEMACH) described deficiencies in knowledge and poor resuscitation skills among obstetrical caregivers and recommended that all clinical staff undergo regular training in basic and advanced CPR.1 The report also emphasised that changes in medical training and work patterns have reduced the exposure of junior medical staff to life-threatening illness and suggested the use of simulator training.1
Various methods, including simulation8 and written surveys,9,10 have been used to assess knowledge of maternal cardiac arrest, although none has assessed the effectiveness of teaching interventions on subsequent performance during simulations or real life. With regard to electronic learning (e-learning), Ruiz et al.11 stated that “several studies outside of health care have revealed that most often e-learning is at least as good as, if not better than, traditional instructor-led methods such as lectures in contributing to demonstrated learning.” Evidence suggests that e-learning is more efficient, and this enhanced efficiency is likely to translate into improved motivation and performance.12 The e-learners demonstrated increased retention rates and better utilization of content, resulting in better achievement of knowledge, skills, and attitudes.12 Some studies, however, used complex e-learning simulator packages that are not routinely available in all institutions.11,13,14 In the medical education field, conflicting opinions remain on the efficacy of e-learning vs traditional instructor-led methods.11,13,14 Our institution currently employs lecture-style and interactive didactic teaching sessions for teaching residents, but it also has a well-established, computer-based continuing medical education program. We were interested to see if there was a difference between the two teaching methods in terms of future development of our teaching program for residents.
The objectives of this study were to test the performance of anesthesia residents in the management of maternal cardiac arrest using a high-fidelity simulation and to compare their subsequent performance following either a didactic teaching session or completion of an e-learning module. We hypothesized that teaching would result in better performance of maternal resuscitation and an earlier start to PMCD. We also hypothesized that performance could be potentially affected by the method of teaching. Time from onset of cardiac arrest to PMCD was considered the outcome measure as it is a critical step in the management of maternal cardiac arrest. Moreover, without early consideration of PMCD, resuscitation efforts are less likely to be successful.
Methods
Institutional Research Ethics Board approval (Reference 10-206-E, September 2010) was obtained for this prospective, assessor-blinded, observational cohort study. Anesthesia residents in postgraduate years 2-4 at the University of Toronto who had completed their dedicated three-month training in obstetrical anesthesia were recruited, and written informed consent was obtained. All residents signed a confidentiality agreement not to disclose study details to anyone other than the study personnel and not to participate in any other research related to obstetrical anesthesia during the study period.
A computer-generated randomization sequence (block sizes of 4; 1:1 allocation ratio) was used to allocate residents to one of two teaching groups: didactic (Didactic group) or e-learning (Electronic group). The allocation was concealed by sequentially numbered, sealed, opaque envelopes containing the assigned study number and training modality. These envelopes were prepared and kept by an independent research assistant, who recruited the participants. Participants were not aware of the nature of the scenario on which they would be assessed, which required them to take the role of leader in a simulated case of maternal cardiac arrest (pulseless electrical activity [PEA] secondary to amniotic fluid embolus). They subsequently either participated in a 30-min, narrated PowerPoint©-based teaching session with the research investigator (A.H.), including time for interactive discussion (Electronic supplementary material 1), or were given a computerized, password-protected link to a Word©-based e-learning session (Electronic supplementary material 2), which they could complete at their own pace and convenience.
Both teaching methods were standardized to cover the same information, which was prepared by consensus among the study investigators after a thorough literature review. This comprised a review of the respiratory, cardiovascular, and gastrointestinal physiological changes of pregnancy, a review of the general adult Advanced Cardiovascular Life Support (ACLS) guidelines (including the visual cardiac arrest algorithm), American Heart Association (AHA) guidelines on the management of cardiac arrest during pregnancy (including explanations for those modifications based on the physiological changes of pregnancy), and a review of when/why/how to perform PMCD.3,4 Participants randomized to the Electronic group were unable to print the e-learning document or access the e-link once the full session had been completed. One month after their teaching intervention, the participants returned to complete a second simulated maternal cardiac arrest scenario (PEA secondary to massive vaginal hemorrhage). There was no additional testing on knowledge acquisition during the study period.
The simulation sessions were conducted at the Program for Resuscitation Education and Patient Safety Laboratory at Mount Sinai Hospital. The simulation process itself was standardized for all participants and used a high-fidelity, life-sized SimMan© mannequin (Laerdal Medical Canada, Toronto, ON, Canada) with programmable monitors. The mannequin had palpable pulses, an airway that could be intubated, and chest movement with appropriate ventilation. To optimize realism, an abdominal flap was fitted over the mannequin’s abdomen that could be lifted for delivery of the fetus.
Participants were orientated to the simulation room, mannequin, and available equipment. The debriefing and evaluation processes were explained. Participants were specifically instructed that they should perform all actions as in a real-life case and verbalize their thoughts to enable appropriate evaluation. They were also asked to verbalize the actions that, as per the standard policy of the simulation laboratory, could not be performed on the mannequin (such as placement of a second intravenous line or drug injection), although these actions were “performed” by the actors using the appropriate equipment in real time. Drug vials contained normal saline instead of real medications. Defibrillation equipment was available and functioned for monitoring and shock delivery if and when requested. The simulations were performed with a common team of actors in the roles of obstetrician, nurse, and respiratory therapist. The programmer and actors were provided with guidelines on how often and what specific verbal responses should be provided in real time, either voluntarily or in response to a participant’s question. After the first simulation session, participants received general feedback by the study investigator. However, given the nature of the study, no specific teaching comments or learning points were made at this stage. This deviation from standard simulation debriefing procedures was explained to participants, who were informed that they would learn via the study teaching methods and receive a more focussed debriefing after the second session. Participants were not aware of the outcome measures or assessment criteria. The debriefing after the second session involved interactive oral feedback and a constructive critique, along with the opportunity for participants to provide the study investigators with feedback on their experience. The duration of the debriefing after this session varied depending on the participant but in all cases covered the areas discussed above.
Digital videography was used to record the simulation scenarios, with vital signs superimposed on the image. The recordings were later independently reviewed and scored on both technical and nontechnical skills by two assessors blinded to group allocation, the training level of the participant, and scores given by the other rater. The assessors were experts in obstetrical anesthesia and simulation assessment and received the recordings in random order. The time from onset of cardiac arrest to the start of PMCD was recorded using the automated stopwatch displayed during the video recording. Starting time for PMCD was defined as the time at which participants instructed the obstetrician to make the skin incision. The technical skills were assessed using a checklist (Appendix) developed by consensus among the study investigators and based on recent AHA guidelines.3,4 Participants were expected to verbalize their identification of the arrest rhythm and potential causes as per standard ACLS management. For general ACLS skills, a score of 0 to 2 was assigned, where 0 = not done, 1 = done but with errors, and 2 = performed correctly. For pregnancy modifications, participants scored 1 if the task was done and 0 if it was not. Both scores were added to give a final overall technical score. The Anaesthetists’ Non-Technical Skills15 (ANTS) scoring system was used for nontechnical skills. It is a reliable and previously validated scale that scores participants on a scale of 1-4 (1 = poor, 2 = marginal, 3 = acceptable, 4 = good) for each of four categories (task management, team working, situational awareness, decision-making). Prior to assessing the video recordings, both assessors were provided with the ANTS literature and the user manual.Footnote 1 Before independently rating the study recordings, the assessors viewed recordings unrelated to the study and discussed their ratings to produce a consensus rating.
The primary outcome measure was the difference in time from cardiac arrest to the start of PMCD in the pre-teaching and post-teaching sessions. Secondary outcomes were differences in time to PMCD between the two teaching methods and differences in the technical and nontechnical skills scores between the two teaching groups.
Statistical analysis
Descriptive statistics using medians and interquartile ranges were used to summarize the primary outcome measure because of the skewed distributions and the small sample size. The time from the arrest to the start of PMCD was compared prior to and after teaching using nonparametric Wilcoxon signed-rank tests for paired data, as were the continuous and ordinal secondary outcome measures (differences in technical and nontechnical skills scores). Nonparametric Mann-Whitney U-tests were performed for the secondary analyses (comparison of outcomes between the two teaching groups). Interrater reliability for the consistency of ANTS scores was calculated by intraclass correlation coefficients (ICCs) (1, 2) using average measures similar to the model of Shrout and Fliess.16 All analyses were conducted with SAS version 9.2 software (SAS, Cary, NC, USA). P < 0.05 was considered statistically significant.
There is currently limited information on the effectiveness of teaching interventions for the improvement of decision-making for PMCD. A previous study reported a successful outcome when PMCD was performed within 15 min of arrest, although no cases were done within 5 min.17 Therefore, we assumed that a mean time of 10 min would be required to start PMCD during the pre-teaching sessions.17 Using sample size calculations for Wilcoxon signed-rank tests, 20 participants were required to detect a significant sum of ranks of 158 (i.e., a reduction in time to PMCD following training in 11 participants) and also to detect a difference in the median change in time to PMCD of ≥ 2.5 min between two randomly assigned education methods, with 80% power and a type I error of 0.05.18,19 Residents were invited to participate on an ongoing basis until the required sample size was achieved.
Results
The study was conducted between November 2010 and May 2011. Of the 60 residents invited to participate, the first 20 who agreed and participated in both sessions were recruited. Ten were randomized to each study group, and they all completed both simulation sessions. The details of their characteristics are shown in Table 1. Each participant had completed at least three months of dedicated obstetrical anesthesia teaching and had previously undergone simulator training using the SimMan© mannequin. Only one participant had seen a real-life maternal cardiac arrest.
Overall, there was a significant improvement in the time to decision for PMCD after teaching from a median (interquartile range [IQR]) of 4.5 [3.4, 5.1] min to 3.5 [2.5, 4.0] min (P = 0.03). However, there was no significant change from baseline either within or between groups (Table 2). At post-teaching sessions, 60% of participants in the Didactic group started PMCD within four minutes of maternal cardiac arrest, compared with 70% in the Electronic group. Overall, technical skills scores improved after the teaching intervention (P < 0.001), and there was no statistically significant difference in the change seen between the two groups (Table 3).
During their baseline assessment, many residents did not perform required life support tasks or the recommended modifications of these tasks for pregnancy (Table 3). The poorly performed skills were drug administration (dose and/or timing), consideration of the cause of the arrest, and rhythm recognition. Except for recognition of cardiac arrest, none of the life support skills had significantly improved at the post-teaching sessions. In terms of modifications for pregnancy, a high percentage of participants called for obstetrical help, applied left uterine displacement (LUD), and intubated early; but only a small proportion adjusted hand position during compressions or applied cricoid pressure during bag-mask ventilation. Although the latter two skills improved significantly after teaching, they were performed in only < 50% of cases. The request for neonatology assistance remained consistently poor throughout the study, and the number of participants requesting senior anesthesiology assistance decreased at the post-teaching simulation.
The scores for the ANTS categories improved significantly after teaching. However, there was no difference in the change from baseline between the two groups (Table 4). The ICCs in pre-teaching and post-teaching ratings were 0.78 and 0.60, respectively, which indicates moderate to substantial consistency of the assessors’ scores.
Discussion
This study demonstrated that teaching improves anesthesia residents’ performance for addressing simulated maternal cardiac arrest but showed no difference between didactic teaching and e-learning. After specific teaching, most participants were able to perform PMCD within the recommended time frame of four minutes from the onset of maternal cardiac arrest.
Our study showed that residents were aware of the need for PMCD, with 85% requesting it before their teaching intervention and 100% afterward. At the baseline session, only 65% considered “bedside” PMCD; this proportion had improved to 95% at the post-teaching session. Following teaching, the median decision time from cardiac arrest to starting PMCD improved to less than four minutes, although no difference was seen between the two teaching groups. Although these results initially seem encouraging, only 60% of participants requested PMCD within four minutes of the arrest.
Previous studies looking at real-life PMCD have shown that it rarely occurs within five minutes of the onset of cardiac carrest.20 For example, a review of cases in The Netherlands between 1993 and 200817 showed that of eight in-hospital arrests no PMCDs were performed in less than 5 min, three occurred within 5-15 min, four in 16-20 min, and one took > 31 min. The debate regarding the realism of commencing an incision within four minutes of arrest is therefore ongoing, and our results further highlight this question. In real life, mobilizing the cardiac arrest team from remote areas of the hospital, securing intravenous access, and moving the operative equipment to the bedside are necessary interventions but were not practical in our simulation. Consequently, we believe that it may be more realistic if teaching and guidelines do not focus on absolute time frames but, rather, on the recognition that PMCD is one of the early interventions to consider if a pregnant patient does not respond to initial resuscitation measures.
In our study, despite all residents except two holding current ACLS certification, some key skills were performed poorly, both before and after teaching, a finding consistent with those of Lipman et al. 8 Many residents were unsuccessful in identifying the arrest rhythm, considering the cause, and administering the appropriate medications. As these skills are essential for resuscitation, our observations highlight the importance of ongoing teaching and revision of ACLS algorithms. Other studies9 have also found that anesthesia, obstetrical, and emergency medicine specialists have inadequate knowledge of maternal resuscitation measures, including the need for LUD and the potential benefit of early Cesarean delivery. Another study showed that none of the teams in a simulated cardiac arrest scenario provided adequate chest compressions, although 15 of 18 delivered the fetus via operative vaginal delivery within five minutes (median [IQR] 2.51 [2.23, 3.55]).8
Some of the ACLS modifications for pregnancy were performed by a large number of participants in our study (i.e., choosing a smaller-diameter endotracheal tube, intubating early, applying LUD). However, although initially a low percentage applied cricoid pressure for bag-mask ventilation, use of this measure increased significantly at the post-teaching session. Given the increased risk of aspiration in pregnant patients, the importance of cricoid pressure needs to be reinforced in residents’ teaching. Of note, perhaps the one seemingly atypical result in this section was that the number of participants calling for senior anesthesia assistance fell across all groups at the post-teaching sessions. This was noted despite the fact that an early call for senior help is emphasized throughout anesthesia training, and the pre-simulation briefing emphasized the availability of additional assistance if requested. This result may reflect a concerning and inappropriate overconfidence among participants. The CEMACH report also emphasized the need for all clinicians to recognize their limitations and call for assistance.1 We do recognize, however, that this could be an artifact of the simulation process itself, not something that would translate into real-life practice.
There was significant improvement in each of the four categories of the ANTS after teaching, both overall and within groups, although no difference was seen between the two groups. Scores improved in most cases from the “marginal” to the “acceptable” category, which could potentially translate into a clinically significant improvement. Similar improvements in anesthesia residents’ nontechnical skills during anesthesia emergencies and weaning from cardiopulmonary bypass have been shown previously.21,22
Our study does have some limitations. The sample size met our pre-study calculation but nevertheless was small, which may limit the generalizability of our findings. However, it was an observational study designed to provide some initial data and in the absence of previous research can provide a foundation for future investigations in this area. Another concern was that the additional experience of the more senior trainees may have affected results; however, the distribution of trainees was based on randomization, and there was no difference in overall experience between the groups. We did not include a “no teaching” control group as the pretest simulation was used for the sole purpose of baseline comparison of the two groups. As described, limited feedback was offered after this session to minimize bias and to allow reliable testing of the effect of the teaching interventions.
Our checklist for technical skills was developed by the authors and did not undergo validation testing. However, similar to the modified checklist used by Lipman et al.,8 it was derived from current published AHA guidelines and addressed areas critical to the optimal performance of ACLS in the parturient. Future studies are needed to establish the validity of this checklist for formative and summative assessment of participants.
Despite blinding to the teaching groups, based on the simulation scenario the assessors would have been able to discern between the two sessions, although the automated time recordings and the objective checklist minimized this potential bias. We chose two cardiac arrest scenarios with similar basic principles of management, rather than a single scenario, to minimize the influence of the case or content specificity or resident recall to bias performance. Furthermore, we wanted to determine if the knowledge gained would be applicable to other, similar situations.
It might have been more beneficial to investigate our hypothesis by conducting the simulation within a labour and delivery setting to increase the realism of the scenario. In our institution this is not logistically feasible due to patient care requirements. In addition, it is important to remember that maternal cardiac arrest can occur in any setting, both inside and outside a hospital.
In summary, we have shown that anesthesia residents have significant gaps in knowledge and implementation of standard ACLS protocols and the recommended modifications for pregnancy. Although teaching leads to improvements in knowledge and performance, in our study e-learning and didactic learning showed similar benefits in terms of skill acquisition and early knowledge retention. Frequent training and practice in managing maternal cardiac arrest is necessary to improve decision-making regarding the necessity of early Cesarean delivery.
Notes
http://www.abdn.ac.uk/iprc/ants; accessed October 24, 2010.
References
Lewis G. The Confidential Enquiry into Maternal and Child Health (CEMACH). Saving Mothers’ Lives: Reviewing Maternal Deaths to Make Motherhood Safe 2003- 2005. The Seventh Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. RCOG Press, London: CEMACH, 2007. Available from URL: http://www.publichealth.hscni.net/sites/default/files/Saving%20Mothers%27%20Lives%202003-05%20.pdf (accessed June 2012)
Lewis G. Why mothers die 2000–2002. Confidential Enquiry Into Maternal and Child Health. Improving Care for Mothers, Babies and Children. The Sixth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. RCOG Press; London, UK: Centre for Maternal and Child Enquiries; 2004. Available from URL: http://www.hqip.org.uk/assets/NCAPOP-Library/CMACE-Reports/33.-2004-Why-Mothers-Die-2000-2002-The-Sixth-Report-of-the-Confidential-Enquiries-into-Maternal-Deaths-in-the-UK.pdf (accessed June 2012)
2005American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Part 10.8: Cardiac Arrest Associated With Pregnancy. Circulation 2005; 112: IV150-3
Vanden Hoek TL, Morrison LJ, Shuster M, et al. Part 12: Cardiac Arrest in Special Situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010; 122: S829-61.
Katz VL, Dotters DJ, Droegemueller W. Perimortem cesarean delivery. Obstet Gynecol 1986; 68: 571-6.
Katz VL, Balderston K, DeFreest M. Perimortem cesarean delivery: were our assumptions correct? Am J Obstet Gynecol 2005; 192: 1916-21.
Banks A. Maternal resuscitation: plenty of room for improvement. Int J Obstet Anesth 2008; 17: 289-91.
Lipman SS, Daniels KI, Carvalho B, et al. Deficits in the provision of cardiopulmonary resuscitation during simulated obstetric crises. Am J Obstet Gynecol 2010; 203: 179.e1-5
Cohen SE, Andes LC, Carvalho B. Assessment of knowledge regarding cardiopulmonary resuscitation of pregnant women. Int J Obstet Anesth 2008; 17: 20-5.
Einav S, Matot I, Berkenstadt H, Bromiker R, Weiniger CF. A survey of labour ward clinicians’ knowledge of maternal cardiac arrest and resuscitation. Int J Obstet Anesth 2008; 17: 238-42.
Ruiz JG, Mintzer MJ, Leipzig RM. The impact of E-learning in medical education. Acad Med 2006; 81: 207-12.
Clark D. Psychological myths in e-learning. Med Teach 2002; 24: 598-604.
Schwid HA, Rooke GA, Michalowski P, et al. Screen-based anesthesia simulation with debriefing improves performance in a mannequin-based anesthesia simulator. Teaching and Learning in Medicine 2001; 18: 92-6.
Nyssen AS, Larbuisson R, Janssens M, Pendeville P, Mayne A. A comparison of the training value of two types of anesthesia simulators: computer screen-based and mannequin-based simulators. Anesth Analg 2002; 94: 1560-5.
Fletcher G, Flin R, McGeorge P, Glavin R, Maran N, Patey R. Anaesthetists’ Non-Technical Skills (ANTS): evaluation of a behavioural marker system. Br J Anaesth 2003; 90: 580-8.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979; 86: 420-8.
Dijkman A, Huisman CM, Smit M, et al. Cardiac arrest in pregnancy: increasing use of perimortem caesarean section due to emergency skills training? BJOG 2010; 117: 282-7.
Rosner B. Fundamentals of Biostatistics. 3rd ed. Boston: PWS-Kent; 1990 .
Zhao D, Rahardja D, Qu Y. Sample size calculation for the Wilcoxon-Mann-Whitney test adjusting for ties. Stat Med 2008; 27: 462-8.
Jeejeebhoy FM, Zelop CM, Windrim R, Carvalho JC, Dorian P, Morrison LJ. Management of cardiac arrest in pregnancy: a systematic review. Resuscitation 2011; 82: 801-9.
Yee B, Naik VN, Joo HS, et al. Nontechnical skills in anesthesia crisis management with repeated exposure to simulation-based education. Anesthesiology 2005; 103: 241-8.
Bruppacher HR, Alam SK, LeBlanc VR, et al. Simulation based training improves physicians’ performance in patient care in high stakes clinical setting of cardiac surgery. Anesthesiology 2010; 112: 985-92.
Acknowledgements
We acknowledge the Department of Anesthesia, University of Toronto, for Merit awards and the Ontario Ministry of Health & Long-term Care, Ontario, Canada, for their financial support in providing Innovation funds for this study. We wish to thank J. Charles Victor, MSc, Epidemiologist, Chronic Disease and Pharmacotherapy Program, Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada, for his help with statistical analysis, and Susan Dunington, MA, Professor in Respiratory Therapy, Michener Institute for Applied Health Sciences, Toronto, Ontario, Canada for her assistance with simulator programming. We are grateful to Dr. David Mazer, Vice Chair, Research, Department of Anesthesia, University of Toronto, for his guidance in this research. We also wish to thank all the actors for their commitment to the study and the Program for Resuscitation Education and Patient Safety (PREPS) laboratory staff at Mount Sinai Hospital for providing facilities for running simulations. Last but not least, we are very grateful to our residents for participating in this research.
Funding
This work was supported by Innovation funds, Ontario Ministry of Health & Long-term Care, Ontario, Canada; Merit awards, Department of Anesthesia, University of Toronto, Ontario, Canada.
Declaration of interests
The study was presented in part at the annual meeting of the Society for Obstetric Anesthesia and Perinatology, Henderson, NV, April 13-17, 2011; the Canadian Anesthesiology Society annual meeting, Toronto, ON, Jun 24-28, 2011; and the Faculty Development Day, University of Toronto. Nov 11, 2010.
Competing interests
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Andrea Hards contributed to the study conception and design, acquisition of data, analysis, and interpretation of data. She drafted and revised the article and approved the final version. Sharon Davies contributed to study conception and design, reviewed the analysis of the data, and revised and approved the final manuscript. Aliya Salman contributed to acquisition of data and approved the final manuscript. Magda Erik-Soussi contributed to acquisition of data, reviewed the data, and revised and approved the final version. Mrinalini Balki contributed to the study conception and design, acquisition of data, analysis and interpretation of data. She also drafted and revised the article and approved the final version.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix: Technical skills checklist
Appendix: Technical skills checklist
Life support skills | |||
|---|---|---|---|
Action | Not done | Done but with errors | Done correctly |
Recognizes the clinical change and reassesses | 0 | 1 | 2 |
Starts basic life support | 0 | 1 | 2 |
Identifies arrest rhythm | 0 | 1 | 2 |
Calls “code blue” | 0 | 1 | 2 |
Calls for crash cart | 0 | 1 | 2 |
Considers appropriate cause | 0 | 1 | 2 |
Gives drugs as per algorithm | 0 | 1 | 2 |
Postintubation asynchronous compressions | 0 | 1 | 2 |
Modifications for pregnancy | |||
Calls for obstetrician | Y / N | ||
Calls for senior anesthesiologist | Y / N | ||
Calls for neonatologist | Y / N | ||
Bag-mask ventilation with cricoid pressure | Y / N | ||
Rapid intubation | Y / N | ||
Uses smaller-diameter endotracheal tube | Y / N | ||
Applies left uterine displacement | Y / N | ||
Adjusts hand position for compressions | Y / N | ||
Requests bedside perimortem CD | Y / N | ||
Performs concurrent CPR | Y / N | ||
Treats the pregnancy and case-specific cause | Y / N | ||
Rights and permissions
About this article
Cite this article
Hards, A., Davies, S., Salman, A. et al. Management of simulated maternal cardiac arrest by residents: didactic teaching versus electronic learning. Can J Anesth/J Can Anesth 59, 852–860 (2012). https://doi.org/10.1007/s12630-012-9752-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-012-9752-2