Abstract
Objectives
Physical activity is recommended for disability prevention in the older adult population; however, the level of physical activity required for older adults with chronic kidney disease (CKD) remains unknown. This study aimed to examine the associations between daily physical activity and disability incidence in older adults with and without CKD to determine relevant daily physical activity levels.
Design
Prospective observational study.
Setting and Participants
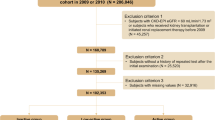
3,786 community-dwelling older adults aged ≥65 years.
Measurements
Mean daily times spent in light- (LPA) and moderate-to-vigorous physical activity (MVPA) were measured using triaxial accelerometers. CKD was defined by a creatinine estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2. Disability incidence was identified as long-term care insurance certification during a 60-month follow-up period. Associations between physical activity and disability incidence were examined using Cox proportional hazard models stratified by the CKD status. Non-linear and linear associations were tested using the restricted cubic spline.
Results
A total of 1,054 individuals were identified to have CKD. Disability incidence was higher in the CKD group than in the non-CKD group. The adjusted cox proportional hazard models indicated that a 10-minute increase in MVPA time was associated with lower disability incidence in the non-CKD group (hazard ratio [HR], 0.838; 95% confidence interval [CI]: 0.764–0.918) and the CKD group (HR, 0.859; 95% CI: 0.766–0.960). Linear associations were observed in MVPA for the non-CKD and CKD groups.
Conclusion
Increasing MVPA was associated with lower disability incidence in older adults with and without CKD. These findings can help devise disability prevention strategies for older CKD patients.


Similar content being viewed by others
References
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204–1222. Doi: https://doi.org/10.1016/S0140-6736(20)30925-9.
Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet 2013;382:339–352. Doi: https://doi.org/10.1016/S0140-6736(13)60595-4.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351:1296–1305. Doi: https://doi.org/10.1056/NEJMoa041031.
Perlman RL, Finkelstein FO, Liu L, et al. Quality of life in chronic kidney disease (CKD): A cross-sectional analysis in the Renal Research Institute-CKD study. Am J Kidney Dis 2005;45:658–666. Doi: https://doi.org/10.1053/j.ajkd.2004.12.021.
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, Hobbs FD. Global prevalence of chronic kidney disease—A systematic review and meta-analysis. PLoS One 2016;11:e0158765. Doi: https://doi.org/10.1371/journal.pone.0158765.
Imai E, Horio M, Watanabe T, et al. Prevalence of chronic kidney disease in the Japanese general population. Clin Exp Nephrol 2009;13:621–630. Doi: https://doi.org/10.1007/s10157-009-0199-x.
Yamada M, Arai H, Nishiguchi S, et al. Chronic kidney disease (CKD) is an independent risk factor for long-term care insurance (LTCI) need certification among older Japanese adults: A two-year prospective cohort study. Arch Gerontol Geriatr 2013;57:328–332. Doi: https://doi.org/10.1016/j.archger.2013.03.009.
Smyth A, Glynn LG, Murphy AW, et al. Mild chronic kidney disease and functional impairment in community-dwelling older adults. Age Ageing. 2013;42(4):488–494. doi:https://doi.org/10.1093/ageing/aft007
Wang XH, Mitch WE. Mechanisms of muscle wasting in chronic kidney disease. Nat Rev Nephrol 2014;10:504–516. Doi: https://doi.org/10.1038/nrneph.2014.112.
Sabatino A, Cuppari L, Stenvinkel P, Lindholm B, Avesani CM. Sarcopenia in chronic kidney disease: “What have we learned so far? J Nephrol 2021;34:1347–1372. Doi: https://doi.org/10.1007/s40620-020-00840-y.
Hiraki K, Yasuda T, Hotta C, et al. Decreased physical function in pre-dialysis patients with chronic kidney disease. Clin Exp Nephrol 2013;17:225–231. Doi: https://doi.org/10.1007/s10157-012-0681-8.
Lee J, Walker ME, Gabriel KP, Vasan RS, Xanthakis V. Associations of accelerometer-measured physical activity and sedentary time with chronic kidney disease: The Framingham Heart Study. PLoS One 2020;15:e0234825. Doi: https://doi.org/10.1371/journal.pone.0234825.
Zha Y, Qian Q. Protein nutrition and malnutrition in CKD and ESRD. Nutrients. 2017;9:208. Doi: https://doi.org/10.3390/nu9030208.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56:M146–M156. Doi: https://doi.org/10.1093/gerona/56.3.M146.
Mijnarends DM, Koster A, Schols JMGA, et al. Physical activity and incidence of sarcopenia: The population-based AGES-Reykjavik Study. Age Ageing 2016;45:614–620. Doi: https://doi.org/10.1093/ageing/afw090.
Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: The LIFE study randomized clinical trial. JAMA 2014;311:2387–2396. Doi: https://doi.org/10.1001/jama.2014.5616.
Hotta C, Hiraki K, Izawa KP, Sakurada T, Shibagaki Y. Physical activity in patients with pre-dialysis chronic kidney disease is related to physical function. Clin Exp Nephrol 2020;24:1189–1190. Doi: https://doi.org/10.1007/s10157-020-01939-z.
Hamada M, Yasuda Y, Kato S, et al. The effectiveness and safety of modest exercise in Japanese patients with chronic kidney disease: A single-armed interventional study. Clin Exp Nephrol 2016;20:204–211. Doi: https://doi.org/10.1007/s10157-015-1147-6.
Howden EJ, Coombes JS, Strand H, Douglas B, Campbell KL, Isbel NM. Exercise training in CKD: Efficacy, adherence, and safety. Am J Kidney Dis 2015;65:583–591. Doi: https://doi.org/10.1053/j.ajkd.2014.09.017.
Zelle DM, Klaassen G, van Adrichem E, et al. Physical inactivity: a risk factor and target for intervention in renal care. Nat Rev Nephrol. 2017;13(3):152–168. doi:https://doi.org/10.1038/nrneph.2016.187
Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sports Exerc 2011;43:1334–1359. Doi: https://doi.org/10.1249/MSS.0b013e318213fefb.
Mañas A, Del Pozo-Cruz B, Guadalupe-Grau A, et al. Reallocating accelerometer-assessed sedentary time to light or moderate- to vigorous-intensity physical activity reduces frailty levels in older adults: An isotemporal substitution approach in the TSHA study. J Am Med Dir Assoc 2018;19:185.e1-185.e6. Doi: https://doi.org/10.1016/j.jamda.2017.11.003.
Howden EJ, Weston K, Leano R, et al. Cardiorespiratory fitness and cardiovascular burden in chronic kidney disease. J Sci Med Sport 2015;18:492–497. Doi: https://doi.org/10.1016/j.jsams.2014.07.005.
Shimada H, Tsutsumimoto K, Lee S, et al. Driving continuity in cognitively impaired older drivers. Geriatr Gerontol Int 2016;16:508–514. Doi: https://doi.org/10.1111/ggi.12504.
Stevens PE, Levin A; Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825–830. Doi: https://doi.org/10.7326/0003-4819-158-11-201306040-00007.
Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009;53:982–992. Doi: https://doi.org/10.1053/j.ajkd.2008.12.034.
Kumahara H, Schutz Y, Ayabe M, et al. The use of uniaxial accelerometry for the assessment of physical-activity-related energy expenditure: A validation study against whole-body indirect calorimetry. Br J Nutr 2004;91:235–243. Doi: https://doi.org/10.1079/BJN20031033.
Gorman E, Hanson HM, Yang PH, Khan KM, Liu-Ambrose T, Ashe MC. Accelerometry analysis of physical activity and sedentary behavior in older adults: A systematic review and data analysis. Eur Rev Aging Phys Act 2014;11:35–49. Doi: https://doi.org/10.1007/s11556-013-0132-x.
Yamada M, Arai H. Long-term care system in Japan. Ann Geriatr Med Res 2020;24:174–180. Doi: https://doi.org/10.4235/agmr.20.0037.
Tsutsumimoto K, Doi T, Shimada H, et al. Combined effect of slow gait speed and depressive symptoms on incident disability in older adults. J Am Med Dir Assoc 2016;17:123–127. Doi: https://doi.org/10.1016/j.jamda.2015.08.012.
Satake S, Arai H. The revised Japanese version of the Cardiovascular Health Study criteria (revised J-CHS criteria). Geriatr Gerontol Int 2020;20:992–993. Doi: https://doi.org/10.1111/ggi.14005.
Ministry of Health. LaW, Japan. Active Guide. Japanese Official Physical Activity Guidelines for Health Promotion. https://www.mhlw.go.jp/stf/houdou/2r9852000002xple.html. Accessed 2 June 2021; 2013.
Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 2010;29:1037–1057. Doi: https://doi.org/10.1002/sim.3841.
Saint-Maurice PF, Troiano RP, Matthews CE, Kraus WE. Moderate-to-vigorous physical activity and all-cause mortality: Do bouts matter? J Am Heart Assoc 2018;7. Doi: https://doi.org/10.1161/JAHA.117.007678.
Shah RC, Buchman AS, Leurgans S, Boyle PA, Bennett DA. Association of total daily physical activity with disability in community-dwelling older persons: A prospective cohort study. BMC Geriatr 2012;12:63. Doi: https://doi.org/10.1186/1471-2318-12-63.
Makino K, Lee S, Lee S, et al. Daily physical activity and functional disability incidence in community-dwelling older adults with chronic pain: A prospective cohort study. Pain Med 2019;20:1702–1710. Doi: https://doi.org/10.1093/pm/pny263.
Cooper AJM, Lamb MJE, Sharp SJ, Simmons RK, Griffin SJ. Bidirectional association between physical activity and muscular strength in older adults: Results from the UK Biobank study. Int J Epidemiol 2017;46:141–148. Doi: https://doi.org/10.1093/ije/dyw054.
Chen T, Honda T, Chen S, Narazaki K, Kumagai S. Dose-response association between accelerometer-assessed physical activity and incidence of functional disability in older Japanese adults: A 6-year prospective study. J Gerontol A Biol Sci Med Sci 2020;75:1763–1770. Doi: https://doi.org/10.1093/gerona/glaa046.
Loprinzi PD, Sheffield J, Tyo BM, Fittipaldi-Wert J. Accelerometer-determined physical activity, mobility disability, and health. Disabil Health J 2014;7:419–425. Doi: https://doi.org/10.1016/j.dhjo.2014.05.005.
Heiwe S, Jacobson SH. Exercise training in adults with CKD: A systematic review and meta-analysis. Am J Kidney Dis 2014;64:383–393. Doi: https://doi.org/10.1053/j.ajkd.2014.03.020.
de Oliveira Brito LV, Maranhao Neto GA, Moraes H, Emerick RF, Deslandes AC. Relationship between level of independence in activities of daily living and estimated cardiovascular capacity in elderly women. Arch Gerontol Geriatr 2014;59:367–371. Doi: https://doi.org/10.1016/j.archger.2014.05.010.
Kirkman DL, Muth BJ, Stock JM, Townsend RR, Edwards DG. Cardiopulmonary exercise testing reveals subclinical abnormalities in chronic kidney disease. Eur J Prev Cardiol 2018;25:1717–1724. Doi: https://doi.org/10.1177/2047487318777777.
Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–1462. Doi:https://doi.org/10.1136/bjsports-2020-102955
Amagasa S, Machida M, Fukushima N, et al. Is objectively measured light-intensity physical activity associated with health outcomes after adjustment for moderate-to-vigorous physical activity in adults? A systematic review. Int J Behav Nutr Phys Act 2018;15:65. Doi: https://doi.org/10.1186/s12966-018-0695-z.
Qiu S, Cai X, Jia L, et al. Does objectively-measured light-intensity physical activity reduce the risk of cardiovascular mortality? A meta-analysis. Eur Heart J Qual Care Clin Outcomes 2021;7:496–504. Doi: https://doi.org/10.1093/ehjqcco/qcaa051.
Grgic J, Dumuid D, Bengoechea EG, Shrestha N, Bauman A, Olds T, Pedisic Z. Health outcomes associated with reallocations of time between sleep, sedentary behaviour, and physical activity: A systematic scoping review of isotemporal substitution studies. Int J Behav Nutr Phys Act 2018;15:69. Doi: https://doi.org/10.1186/s12966-018-0691-3.
Dunlop DD, Song J, Semanik PA, et al. Relation of physical activity time to incident disability in community dwelling adults with or at risk of knee arthritis: Prospective cohort study. BMJ 2014;348:g2472. Doi: https://doi.org/10.1136/bmj.g2472.
Nicolodi GV, Della Méa Plentz R, Righi NC, Stein C. Effects of aerobic exercise on patients with pre-dialysis chronic kidney disease: a systematic review of randomized controlled trials. Disabil Rehabil 2021:1–10. Doi: https://doi.org/10.1080/09638288.2021.1900929.
MacKinnon HJ, Wilkinson TJ, Clarke AL, et al. The association of physical function and physical activity with all-cause mortality and adverse clinical outcomes in nondialysis chronic kidney disease: A systematic review. Ther Adv Chronic Dis 2018;9:209–226. Doi: https://doi.org/10.1177/2040622318785575.
Weymar F, Braatz J, Guertler D, et al. Characteristics associated with non-participation in 7-day accelerometry. Prev Med Rep 2015;2:413–U8. Doi: https://doi.org/10.1016/j.pmedr.2015.05.003.
Jefferis BJ, Sartini C, Ash S, et al. Trajectories of Objectively Measured Physical Activity in Free-Living Older Men. Med Sci Sport Exerc. 2015;47(2):343–349. Doi: https://doi.org/10.1249/MSS.0000000000000410.
Inker LA, Schmid CH, Tighiouart H, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med 2012;367:20–29. Doi: https://doi.org/10.1056/NEJMoa1114248.
Acknowledgement
We thank the healthcare staff for their valued assistance with the study assessments. We would like to thank Editage (https://www.editage.jp) for English language editing. We would like to thank the JSPS KAKENHI Grant-in-Aid for Young Scientists (grant number: 20K18975) for their support.
Author information
Authors and Affiliations
Contributions
Author contributions: IC was involved in study concept and design, data interpretation, and the manuscript preparation. SL, SB, KM and KH involved in the acquisition of subjects and data. OK, KT, MM, YY and NT critically revised the report, commented on the drafts of manuscript. HS approved the final report.
Corresponding author
Ethics declarations
Ethical Standards: Ethical standards for epidemiological study were adhered to according to guidelines from the Ministry of Health, Labour and Welfare, Japan.
Conflicts of interest: The work in Takahama city was supported by a Research Funding for Longevity Sciences (27–22) from the NCGG, Grant-in-Aid for Scientific Research (A) (26242059), joint research with Kao Corporation, and expenses for R&D were commissioned by Takahama city. This work in Nagoya city was supported by the Strategic Basic Research Programs Redesigning Communities for Aged Society (RISTEX) of the Japan Science and Technology Agency (JST), Health and Labor Sciences Research Grants, and joint research with Kao Corporation.
Additional information
Sponsors role: Kao corporation provided the accelerometers. Other funders played no role in the design, methods, subject recruitment, data collections, analysis and preparation or paper.
Rights and permissions
About this article
Cite this article
Chiba, I., Lee, S., Bae, S. et al. Association of Daily Physical Activity with Disability in Community-Dwelling Older Adults With/Without Chronic Kidney Disease. J Nutr Health Aging 26, 521–528 (2022). https://doi.org/10.1007/s12603-022-1790-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-022-1790-z