Abstract
Background
Coronary microvascular resistance is increased after primary percutaneous coronary intervention (PCI) for ST-elevation myocardial infarction (STEMI), which may be related in part to changed left ventricular (LV) dynamics. Therefore we studied the coronary microcirculation in relation to systolic and diastolic LV function after STEMI.
Methods
The study cohort consisted of 12 consecutive patients, all treated with primary PCI for a first anterior wall STEMI. At 4 months, we assessed pressure-volume loops. Subsequently, we measured intracoronary pressure and flow velocity and calculated coronary microvascular resistance. Infarct size and LV mass were assessed using magnetic resonance imaging.
Results
Patients with an impaired systolic LV function due to a larger myocardial infarction showed a higher baseline average peak flow velocity (APV) than the other patients (26 ± 7 versus 17 ± 5 cm/s, p = 0.003, respectively), and showed an impaired variable microvascular resistance index (2.1 ± 1.0 versus 4.1 ± 1.3 mmHg cm−1∙s−1, p = 0.003, respectively). Impaired diastolic relaxation time was inversely correlated with hyperaemic APV (r = −0.56, p = 0.003) and positively correlated with hyperaemic microvascular resistance (r = 0.48, p = 0.01). LV dilatation was associated with a reduced variable microvascular resistance index (r = 0.78, p = 0.006).
Conclusion
A larger anterior myocardial infarction results in impaired LV performance associated with reduced coronary microvascular resistance variability, in particular due to higher coronary blood flow at baseline in these compromised left ventricles.
Similar content being viewed by others
Introduction
Bax et al. showed that coronary flow velocity reserve (CFVR) and variable microvascular resistance are decreased during the acute phase of ST-elevation myocardial infarction (STEMI), probably due to microembolisation and/or disturbed microvascular autoregulatory function [1, 2]. CFVR has been demonstrated to predict recovery of systolic left ventricular (LV) function after STEMI [1, 3, 4].
CFVR reflects microvascular integrity and may also be influenced by LV dynamics [5]. Clinical reports on this subject are scarce. Recent reports suggest that an increased end-diastolic pressure contributes to coronary microvascular dysfunction in STEMI patients [2, 6]. CFVR has also shown to be decreased in patients with increased LV pressures in dilated ischaemic [7] and non-ischaemic cardiomyopathy [8]. However, the influence of LV dynamics on the coronary microcirculation has not been studied in STEMI patients. We hypothesised that patients with compromised left ventricular dynamics have a disturbed microvascular function.
Therefore, we studied intracoronary haemodynamics in relation to systolic and diastolic LV function as assessed by pressure-conductance catheter [9], in patients at 4 months after their first STEMI.
Methods
Patients
The study population consisted of 12 consecutive patients (10 males, age 57 ± 7 years) who, 4 months previously, had been successfully treated in the proximal left anterior descending coronary artery (LAD) by primary PCI for their first acute anterior STEMI within 6 h after onset of symptoms. Included were patients with an angiographically normal circumflex coronary artery (LCx) to enable comparison of intracoronary measurements in both the infarct-related artery (IRA) and a reference non-IRA. Exclusion criteria were congestive heart failure, previous myocardial infarction, significant valvular disease, and left ventricular thrombus. The study complied with the Declaration of Helsinki and was approved by the institutional research and ethics committee. All patients gave written informed consent.
Study protocol
Patients underwent cardiac catheterisation. Heart rate and 12-lead surface ECGs were monitored and aortic pressure was measured via the guiding catheter. After coronary angiography, the 7F pigtail-equipped combined pressure-conductance catheter (CD Leycom, Zoetermeer, the Netherlands) was placed in the left ventricle through the contralateral femoral artery to assess LV pressure-volume loops, as previously described [9]. A 5 mL blood sample was used to measure blood resistivity rho, and a Swan-Ganz catheter was placed in the pulmonary artery via the femoral vein. Cardiac output was determined by thermodilution and parallel conductance by hypertonic saline injections in order to calibrate the volume signals of the conductance catheter.
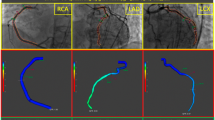
Subsequently, the ComboWire® XT (Volcano Corporation, Rancho Cordova, CA), a 0.014-in. dual-sensor (pressure and Doppler velocity)-equipped guidewire, was used to assess intracoronary pressure and flow velocity signals in the LAD (infarct-related artery) and LCx (nonstenotic and non infarct-related artery) after intracoronary administration of nitroglycerin (0.1 mg), as previously described [10]. The measurements were performed at baseline and during maximal hyperaemia, induced by an intracoronary bolus of adenosine (30–40 μg).
Cardiac magnetic resonance imaging was used to assess LV mass, infarct size (% of LV mass), and the LV remodelling index (LVRi) as calculated by LV mass/EDV [11].
Analysis of LV dynamics
The combined pressure-conductance catheter provides the opportunity to assess continuous information on systolic and diastolic LV function from pressure-volume loops in the catheterisation laboratory. Continuous data from this single catheter enable accurate assessment of the timing and magnitude of therapeutic percutaneous interventions, such as percutaneous coronary intervention or percutaneous aortic valve implantation. Continuously recorded pressure and volume data during a cardiac cycle are displayed as a pressure-volume loop, which represents a working diagram of the left ventricle (Fig. 1), describing LV function during all four phases of the cardiac cycle (i.e. isovolumetric contraction, ejection phase, isovolumetric relaxation, and filling phase). The pressure-volume loop is an extrapolation of the force-length relationships of the cardiac muscle, which are referred to as the Frank Starling law of the heart, and are based on the ventricular function curves of Sarnoff [12] and the force-velocity relations described by Sonnenblick [13]. According to Suga and coworkers, the time-varying elastance model was considered optimal to characterise LV performance [14].
Panel a, illustration of a left ventricular pressure-volume loop of a cardiac cycle. A, isovolumetric contraction; B, ejection phase; C, isovolumetric relaxation; D, filling phase; EDV, end-diastolic volume; EDP, end-diastolic pressure; ESV, end-systolic volume; ESP, end-systolic pressure. Panel b, illustration of a pressure-volume loop of a dilated and failing left ventricle. ESPVR, end-systolic pressure-volume relation; EDPVR, end-diastolic pressure-volume relation, EA, effective arterial elastance. Note the decreased contractility indicated by the decreased slope (EES) and the rightward shift of the ESPVR. The end-diastolic stiffness has increased indicated by the slope of the EDPVR. The left ventricular distensibility has decreased indicated by the upward shift of the EDPVR. Furthermore, left ventricular performance has decreased indicated by decrease in the ventricular-arterial coupling ratio (EES/EA)
In our study, LV dynamics were analysed off-line from the recordings of the pressure-conductance catheter. Per-beat averages of the recorded variables were calculated as the mean of all beats during a steady state of at least 12 s and covering two respiratory cycles. Several indices for overall cardiac performance were obtained as previously described [15, 16], i.e. the ventricular-arterial coupling ratio (EES/EA), which describes the interaction between systolic LV performance and the systemic arterial system [17], as well as specific systolic and diastolic indices, i.e. end-systolic volume and elastance (ESV, EES), ejection fraction (EF), and the relaxation time constant Tau, peak negative derivative of LV pressure (dP/dtmin), peak filling rate (PFR), end-diastolic volume, pressure and elastance (EDV, EDP, EED), respectively.
Analysis of intracoronary haemodynamics
Physiological assessment of intracoronary haemodynamics has become increasingly important for diagnosis and treatment [18] and research applications. After achievement of maximal blood flow in response to hyperaemic stimulation, the fractional flow reserve and/or CFVR may be calculated, respectively. CFVR is a combined measure of the capacity of the major resistance components (the epicardial coronary artery and microvascular bed) to achieve maximal blood flow in response to hyperaemic stimulation. A normal CFVR implies that both the epicardial and minimally achievable microvascular resistances are low and normal. By combining pressure and flow velocity measurements, the status of coronary microvascular function can be determined by calculation of the coronary microvascular resistance index. The advanced single-wire technique allows easier and more accurate (i.e. it measures at exactly the same location) assessment of coronary microvascular function, and its response to treatment [10].
In our study, the digital recordings of aortic pressure, intracoronary pressure and flow velocity were analysed off-line, as previously described [19]. Per-beat averages of the recorded variables were calculated as the mean of 8 beats during baseline, and the mean of at least 3 beats during maximal hyperaemia. The following indices were calculated: mean aortic pressure (Pa), mean distal coronary pressure (Pd), average peak flow velocity (APV), and coronary flow velocity reserve (hyperaemic APV/baseline APV). The coronary microvascular resistance index was calculated by Pd/APV. The variable arteriolar resistance index, which represents autoregulatory function, was expressed as baseline microvascular resistance minus hyperaemic microvascular resistance [2, 20].
Statistical analysis
Data are expressed as mean ± SD or n (%). The two-tailed paired and unpaired t-tests were used where appropriate. The one-tailed bivariate Pearson’s correlation was used to determine correlations between intracoronary and LV function parameters. SPSS release 15.0.1 statistical software package for windows (SPSS Inc. 2006, Chicago, Illinois) was used for analyses. A p-value of less than 0.05 was considered statistically significant.
Results
Patient characteristics
The patient characteristics of the 12 patients are shown in Table 1. All patients were treated with similar medication, i.e. statins, ACE inhibitors, β-blockers, aspirin and clopidogrel. There were no significant differences in the coronary haemodynamics of the LAD (i.e. IRA) and the LCx (i.e. non-IRA), as shown in Table 2.
Systolic LV function and the coronary microcirculation
Patients were divided on the basis of their systolic LV performance in relation to the systemic arterial system. It was previously shown that patients with normal LV performance have a mean EES/EA of 1.62, and patients with a severely impaired LV performance an EES/EA ≤1.0 [21]. Our patients were divided into two equal groups of 6 patients: group 1, patients with impaired systolic LV function with an EES/EA <1.15 (0.90 ± 0.25), and group 2, patients with normal systolic LV function with an EES/EA >1.15 (1.88 ± 0.66). We compared LV dynamics and coronary microcirculatory function between the two groups, as shown in Table 3. Patients with normal systolic LV function showed smaller infarct size and larger LV mass. There was an increased baseline APV of 26 ± 7 cm/s (normal reference value is 18 cm/s) [20] in the impaired LV function group, and therefore a lower CFVR of 2.0 ± 0.3 (normal reference value >2). Furthermore, group 1 showed a reduced variable resistance index. Figure 2, panel a, shows the positive correlation of EES/EA with the variable resistance index.
Correlations of left ventricular (LV) function and degree of remodelling with the variable resistance index as measured in the infarct-related artery (IRA) and non-IRA. Panel a, shows the positive correlation of the ventricular-arterial coupling ratio (EES/EA) with the variable microvascular resistance index (variable MR). Panel b, shows the positive correlation of the left ventricular remodelling index (LVRi) with the variable MR. Note that in patients with better performing left ventricles and in patients with a higher LVRi, indicating a more favourable amount of LV mass compared with LV end-diastolic volume, there is a better microvascular autoregulatory function
Diastolic LV function and the coronary microcirculation
Among the 12 patients, there were 3 patients with diastolic LV dysfunction indicated by an EDP >16 mmHg, according to the definitions described by the Heart Failure and Echocardiography Associations of the European Society of Cardiology [22]. Therefore, most of the individual parameters for diastolic LV function tested for correlation with coronary haemodynamics fell within the normal range. The relaxation time constant Tau was inversely correlated with hyperaemic APV (r = −0.56, p = 0.003) and positively correlated with hyperaemic microvascular resistance (r = 0.48, p = 0.01).
The magnetic resonance imaging derived remodelling parameter LVRi (Fig. 2, panel b) and LV mass correlated with the variable resistance index, i.e. better autoregulatory microcirculatory function (r = 0.78, p = 0.006 and r = 0.52, p = 0.01, respectively).
Discussion
This study is the first to demonstrate that a larger anterior myocardial infarction results in impaired LV performance associated with reduced coronary microvascular resistance variability, in particular due to a higher coronary blood flow at baseline in these compromised left ventricles.
Microcirculation and LV dynamics
A previous report by Bax et al. showed the prognostic value of CFVR on left ventricular function during a 6-month follow-up period [1]. Recently, Hirsch et al. showed that flow characteristics (e.g., CFVR and diastolic deceleration rate) correlated to microvascular obstruction as determined by magnetic resonance imaging [23]. These reports suggest that microvascular integrity is related to larger infarct size and worse outcome because it is known that infarct size is a critical determinant of LV function, which in turn is the most important determinant of early and long-term survival [24].
However, these studies had a different design than ours. In those patients no LV haemodynamics were assessed, nor were patients divided on the basis of LV function. In other previous clinical reports, an association of coronary haemodynamics with LV function was suggested but not (directly) measured [2, 6, 8, 25, 26].
In our study we combined, for the first time, single-wire intracoronary pressure and flow velocity measurements with LV dynamic measurements. Intracoronary haemodynamic measurements have shown to be a sensitive method for determining microvascular resistance [10]. The reduced CFVR and reduced variable microvascular resistance index is merely due to a higher blood flow velocity at baseline conditions. Patients with a larger infarct are characterised by a lower blood pressure and higher heart rate, as signs of a compromised LV performance. This impaired LV performance is also indicated by the significant difference in end-systolic elastance and ejection fraction, and results in a reduced microvascular resistance at baseline. This reduction in microvascular resistance is more pronounced at baseline than in hyperaemic conditions, resulting in a reduced coronary microvascular resistance variability (Fig. 2, panel a).
In accordance with our observations in systolic LV function, we also observed an association with LV dilatation. The LV remodelling index showed a large correlation with the degree of microcirculatory dysfunction, i.e. the variable resistance index (Fig. 2, panel b). These findings implicate that limiting infarct size does not only preserve LV function, but also coronary microvascular function.
Limitations
Our studied population did not allow a comparison of patients with diastolic LV dysfunction with normal diastolic LV function in association with microcirculatory function, since there were only a few patients with diastolic LV dysfunction. The combination of invasively measured LV function and intracoronary haemodynamics was studied in a small sample size, which was evaluated only at 1 moment in time, i.e. at 4 months after STEMI.
Clinical implications
In patients with a larger myocardial infarction, the left ventricle performs inefficiently against the afterload of the systemic arterial system (reduced ventricular-arterial coupling ratio). The coronary circulation shows their compensation mechanism by increasing coronary flow velocity during baseline conditions (baseline APV), resulting in a decrease in CFVR and variable microvascular resistance
Obviously, the most important therapy remains urgent reperfusion to limit infarct size, in order to preserve LV function and coronary microvascular integrity. Though speculative, in patients with a large anterior STEMI, in addition to pharmacological afterload reduction to reduce LV workload, adjunctive measures such as mechanical LV unloading during the acute phase [27] may be useful to preserve LV performance and increase variability in coronary microvascular resistance [19].
Conclusions
In STEMI patients who were treated with primary PCI, we found that a larger anterior myocardial infarction results in an impaired LV performance associated with reduced coronary microvascular resistance variability, in particular due to a higher coronary blood flow at baseline in these compromised left ventricles.
References
Bax M, de Winter RJ, Schotborgh CE, et al. Short- and long-term recovery of left ventricular function predicted at the time of primary percutaneous coronary intervention in anterior myocardial infarction. J Am Coll Cardiol. 2004;43:534–41.
Bax M, de Winter RJ, Koch KT, et al. Time course of microvascular resistance of the infarct and noninfarct coronary artery following an anterior wall acute myocardial infarction. Am J Cardiol. 2006;97:1131–6.
Feldman LJ, Himbert D, Juliard JM, et al. Reperfusion syndrome: relationship of coronary blood flow reserve to left ventricular function and infarct size. J Am Coll Cardiol. 2000;35:1162–9.
Wakatsuki T, Nakamura M, Tsunoda T, et al. Coronary flow velocity immediately after primary coronary stenting as a predictor of ventricular wall motion recovery in acute myocardial infarction. J Am Coll Cardiol. 2000;35:1835–41.
Westerhof N, Boer C, Lamberts RR, et al. Cross-talk between cardiac muscle and coronary vasculature. Physiol Rev. 2006;86:1263–308.
Van Herck PL, Carlier SG, Claeys MJ, et al. Coronary microvascular dysfunction after myocardial infarction: increased coronary zero flow pressure both in the infarcted and in the remote myocardium is mainly related to left ventricular filling pressure. Heart. 2007;93:1231–7.
Garot P, Pascal O, Simon M, et al. Impact of microvascular integrity and local viability on left ventricular remodelling after reperfused acute myocardial infarction. Heart. 2003;89:393–7.
Canetti M, Akhter MW, Lerman A, et al. Evaluation of myocardial blood flow reserve in patients with chronic congestive heart failure due to idiopathic dilated cardiomyopathy. Am J Cardiol. 2003;92:1246–9.
Baan J, van der Velde ET, de Bruin HG, et al. Continuous measurement of left ventricular volume in animals and humans by conductance catheter. Circulation. 1984;70:812–23.
Siebes M, Verhoeff BJ, Meuwissen M, et al. Single-wire pressure and flow velocity measurement to quantify coronary stenosis hemodynamics and effects of percutaneous interventions. Circulation. 2004;109:756–62.
De Castro S, Caselli S, Maron M, et al. Left ventricular remodelling index (LVRI) in various pathophysiological conditions: a real-time three-dimensional echocardiographic study. Heart. 2007;93:205–9.
Sarnoff SJ, Berglund E. Ventricular function. I. Starling’s law of the heart studied by means of simultaneous right and left ventricular function curves in the dog. Circulation. 1954;9:706–18.
Sonnenblick EH. Force-velocity relations in mammalian heart muscle. Am J Physiol. 1962;202:931–9.
Suga H. Ventricular energetics. Physiol Rev. 1990;70:247–77.
Remmelink M, Sjauw KD, Henriques JP, et al. Acute left ventricular dynamic effects of primary percutaneous coronary intervention: from occlusion to reperfusion. J Am Coll Cardiol. 2009;53:1498–502.
Steendijk P, Tulner SA, Bax JJ, et al. Hemodynamic effects of long-term cardiac resynchronization therapy: analysis by pressure-volume loops. Circulation. 2006;113:1295–304.
Sunagawa K, Maughan WL, Burkhoff D, et al. Left ventricular interaction with arterial load studied in isolated canine ventricle. Am J Physiol. 1983;245:H773–80.
Tonino PA, de Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213–24.
Remmelink M, Sjauw KD, Henriques JP, et al. Effects of left ventricular unloading by Impella recover LP2.5 on coronary hemodynamics. Catheter Cardiovasc Interv. 2007;70:532–7.
Chamuleau SA, Siebes M, Meuwissen M, et al. Association between coronary lesion severity and distal microvascular resistance in patients with coronary artery disease. Am J Physiol Heart Circ Physiol. 2003;285:H2194–200.
Starling MR. Left ventricular-arterial coupling relations in the normal human heart. Am Heart J. 1993;125:1659–66.
Paulus WJ, Tschope C, Sanderson JE, et al. How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28:2539–50.
Hirsch A, Nijveldt R, Haeck JD, et al. Relation between the assessment of microvascular injury by cardiovascular magnetic resonance and coronary Doppler flow velocity measurements in patients with acute anterior wall myocardial infarction. J Am Coll Cardiol. 2008;51:2230–8.
Braunwald E. Myocardial reperfusion, limitation of infarct size, reduction of left ventricular dysfunction, and improved survival. Should the paradigm be expanded? Circulation. 1989;79:441–4.
Daher E, Dione DP, Heller EN, et al. Acute ischemic dysfunction alters coronary flow reserve in remote nonischemic regions: potential mechanical etiology identified in an acute canine model. J Nucl Cardiol. 2000;7:112–22.
Shimada Y, Yoshiyama M, Tanaka H, et al. Convalescent stage coronary flow reserve and late myocardial morphologic outcomes in patients with first anterior acute myocardial infarction. Circ J. 2004;68:208–13.
Sjauw KD, Remmelink M, Baan Jr J, et al. Left ventricular unloading in acute ST-segment elevation myocardial infarction patients is safe and feasible and provides acute and sustained left ventricular recovery. J Am Coll Cardiol. 2008;51:1044–6.
Acknowledgments
The authors acknowledge our nursing staff of the cardiac catheterisation laboratory for their skilled assistance, especially W.J. Rohling, RN, T. Wagenaar, RN, W.R. Rozendaal, RN, and S. van Gilst, RN.
Disclosures
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Remmelink, M., Sjauw, K.D., Yong, Z.Y. et al. Coronary microcirculatory dysfunction is associated with left ventricular dysfunction during follow-up after STEMI. Neth Heart J 21, 238–244 (2013). https://doi.org/10.1007/s12471-013-0382-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12471-013-0382-2