Abstract
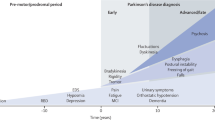
As a multi-factorial degenerative disease, Parkinson’s disease (PD) leads to tremor, gait rigidity, and hypokinesia, thus hampering normal living. As this disease is usually detected in the later stages when neurons have degenerated completely, cure is on hold, ultimately leading to death due to the lack of early diagnostic techniques. Thus, biomarkers are required to detect the disease in the early stages when prevention is possible. Various biomarkers providing early diagnosis of the disease include those of imaging, cerebrospinal fluid, oxidative stress, neuroprotection, and inflammation. Also, biomarkers, alone or in combination, are used in the diagnosis and evolution of PD. This review encompasses various biomarkers available for PD and discusses recent advances in their development.
Similar content being viewed by others
References
Frisardi V, Santamato A, Cheeran B. Parkinson’s disease: new insights into pathophysiology and rehabilitative approaches. Parkinson’s Dis 2016, 2016: 3121727.
Mazzoni P, Shabbott B, Cortés JC. Motor control abnormalities in Parkinson’s disease. Cold Spring Harb Perspect Med 2012, 2: a009282.
Teive HA, Bertucci Filho DC, Munhoz RP. Unusual motor and non-motor symptoms and signs in the early stage of Parkinson’s disease. Arquivos de Neuro-Psiquiatria 2016, 74: 781–784.
Miki Y, Tanji K, Mori F, Kakita A, Takahashi H, Wakabayashi K. PLA2G6 accumulates in Lewy bodies in PARK14 and idiopathic Parkinson’s disease. Neurosci Lett 2017, 645: 40–45.
Gupta R, Kim C, Agarwal N, Lieber B, Monaco EA. Understanding the influence of Parkinson disease on Adolf Hitler’s decision-making during World War II. World Neurosurg 2015, 84: 1447–1452.
Song LK, Ma KL, Yuan YH, Mu Z, Song XY, Niu F, et al. Targeted overexpression of α-synuclein by rAAV2/1 vectors induces progressive nigrostriatal degeneration and increases vulnerability to MPTP in mouse. PLoS One 2015, 10: e0131281.
Cieri D, Brini M, Calì T. Emerging (and converging) pathways in Parkinson’s disease: keeping mitochondrial wellness. Biochem Biophys Res Commun 2017, 483: 1020–1030.
Wu Y, Le W, Jankovic J. Preclinical biomarkers of Parkinson disease. Arch Neurol 2011, 68: 22–30.
Mahlknecht P, Seppi K, Poewe W. The concept of prodromal Parkinson’s disease. J Parkinson’s Dis 2015, 5: 681–697.
Solari N, Bonito-Oliva A, Fisone G, Brambilla R. Understanding cognitive deficits in Parkinson’s disease: lessons from preclinical animal models. Learn Mem 2013, 20: 592–600.
Prakash KG, Bannur BM, Chavan MD, Saniya K, Sailesh KS, Rajagopalan A. Neuroanatomical changes in Parkinson’s disease in relation to cognition: An update. J Adv Pharm Technol Res 2016, 7: 123
Blandini F, Nappi G, Tassorelli C, Martignoni E. Functional changes of the basal ganglia circuitry in Parkinson’s disease. Prog Neurobiol 2000, 62: 63–88.
Brown LL, Schneider JS, Lidsky TI. Sensory and cognitive functions of the basal ganglia. Curr Opin Neurobiol 1997, 7: 157–63
Obeso JA, Rodríguez-Oroz MC, Benitez-Temino B, Blesa FJ, Guridi J, Marin C, et al. Functional organization of the basal ganglia: Therapeutic implications for Parkinson’s disease. Mov Disord 2008, 23(Suppl 3): S548–559
Jankovic J, McDermott M, Carter J, Gauthier S, Goetz C, Golbe L, et al. Variable expression of Parkinson’s disease: A base-line analysis of the DATATOP cohort. The Parkinson Study Group. Neurology 1990, 40: 1529–1534.
Nagae LM, Honce JM, Tanabe J, Shelton E, Sillau SH, Berman BD. Microstructural changes within the basal ganglia differ between Parkinson disease subtypes. Front Neuroanat 2016, 10: 17.
Dickson DV. Neuropathology of movement disorders. In: Tolosa E, Jankovic JJ (Ed.). Parkinson’s Disease and Movement Disorders. Hagerstown, MD: Lippincott Williams & Wilkins 2007: 271–283.
Reetz K, Gaser C, Klein C, Hagenah J, Büchel C, Gottschalk S, et al. Structural findings in the basal ganglia in genetically determined and idiopathic Parkinson’s disease. Mov Disord 2009, 24: 99–103.
Lee SH, Kim SS, Tae WS, Lee SY, Choi JW, Koh SB, et al. Regional volume analysis of the Parkinson disease brain in early disease stage: Gray matter, white matter, striatum, and thalamus. AJNR Am J Neuroradiol 2011, 32: 682–687.
Stoodley CJ. The cerebellum and cognition: Evidence from functional imaging studies. Cerebellum 2012, 11: 352–365.
Rolland AS, Herrero MT, Garcia-Martinez V, Ruberg M, Hirsch EC, François C. Metabolic activity of cerebellar and basal ganglia-thalamic neurons is reduced in Parkinsonism. Brain 2007, 130(Pt 1): 265–275.
Borghammer P, Østergaard K, Cumming P, Gjedde A, Rodell A, Hall N, et al. A deformation-based morphometry study of patients with early-stage Parkinson’s disease. Eur J Neurol 2010, 17: 314–20.
Wu T, Hallett M. The cerebellum in Parkinson’s disease. Brain 2013, 136(Pt 3): 696–709.
Giompres P, Delis F. Dopamine transporters in the cerebellum of mutant mice. Cerebellum 2005, 4: 105–111
Rushton JP, Ankney CD. Whole brain size and general mental ability: A review. Int J Neurosci 2009, 119: 691–731.
Watts RL, Standaertt DG, Obeso JA. Movement Disorders. 3rd ed. New York: McGraw Hill, 2011.
Cerasa A, Messina D, Pugliese P, Morelli M, Lanza P, Salsone M, et al. Increased prefrontal volume in PD with levodopa-induced dyskinesias: A voxel-based morphometry study. Mov Disord 2011, 26: 807–812.
Aglioti S. The role of the thalamus and basal ganglia in human cognition. J Neurolinguistics 1997, 10: 255–265.
Shirvalkar P, Seth M, Schiff ND, Herrera DG. Cognitive enhancement with central thalamic electrical stimulation. Proc Natl Acad Sci U S A 2006, 103: 17007–17012.
Halliday GM. Thalamic changes in Parkinson’s disease. Parkinsonism Relat Disord 2009, 15(Suppl 3): S152–155.
McKeown MJ, Uthama A, Abugharbieh R, Palmer S, Lewis M, Huang X. Shape (but not volume) changes in the thalami in Parkinson disease. BMC Neurol 2008, 8: 8.
Li W, Liu J, Skidmore F, Liu Y, Tian J, Li K. White matter microstructure changes in the thalamus in Parkinson disease with depression: A diffusion tensor MR imaging study. AJNR Am J Neuroradiol 2010, 31: 1861–1866.
Planetta PJ, Schulze ET, Geary EK, Corcos DM, Goldman JG, Little DM, et al. Thalamic projection fiber integrity in de novo Parkinson disease. AJNR Am J Neuroradiol 2013, 34: 74–79.
Zimmerman D. Thinking with your hypothalamus. Philos Phenomenol Res 2001, 63: 521–541.
Langston JW, Forno LS. The hypothalamus in Parkinson disease. Ann Neurol 1978, 3: 129–33.
Politis M, Piccini P, Pavese N, Koh SB, Brooks DJ. Evidence of dopamine dysfunction in the hypothalamus of patients with Parkinson’s disease: An in vivo 11C-raclopride PET study. Exp Neurol 2008;214: 112–116.
Sandyk R, Iacono RP, Bamford CR. The hypothalamus in Parkinson disease. Ital J Neurol Sci 1987, 8: 227–234.
Breen DP, Nombela C, Vuono R, Jones PS, Fisher K, Burn DJ, et al. Hypothalamic volume loss is associated with reduced melatonin output in Parkinson’s disease. Mov Disord 2016, 31: 1062–1066.
Xia J, Miu J, Ding H, Wang X, Chen H, Wang J, et al. Changes of brain gray matter structure in Parkinson’s disease patients with dementia. Neural Regen Res 2013, 8: 1276–1285.
Kulisevsky J, Pagonabarraga J, Martinez-Corral M. Changes in artistic style and behaviour in Parkinson’s disease: Dopamine and creativity. J Neurol 2009, 256: 816–819.
Braak H, Braak E, Yilmazer D, de Vos RA, Jansen EN, Bohl J, et al. Amygdala pathology in Parkinson’s disease. Acta Neuropathol 1994, 88: 493–500.
Isaias IU, Marzegan A, Pezzoli G, Marotta G, Canesi M, Biella GE, et al. A role for locus coeruleus in Parkinson tremor. Front Hum Neurosci 2012, 5: 179.
Bertrand E, Lechowicz W, Szpak GM, Dymecki J. Qualitative and quantitative analysis of locus coeruleus neurons in Parkinson’s disease. Folia Neuropathol 1997, 35: 80–86.
Schwartz WJ, Sharp FR, Gunn RH, Evarts EV. Lesions of ascending dopaminergic pathways decrease forebrain glucose uptake. Nature 1976, 261: 155–157.
Theodosis DT, MacVicar B. Neurone-glia interactions in the hypothalamus and pituitary. Trends Neurosci 1996, 19: 363–367.
Theodosis DT, Poulain DA, Oliet SH. Activity-dependent structural and functional plasticity of astrocyte-neuron interactions. Physiol Rev 2008, 88: 983–1008.
Villalba RM, Smith Y. Neuroglial plasticity at striatal glutamatergic synapses in Parkinson’s disease. Front Syst Neurosci 2011, 5: 68.
Voronkov DN, Khudoerkov RM, Dovedova EL. Changes in neuroglial interactions in nigrostriatal brain structures on modeling of dopamine system dysfunction. Neurosci Behav Physiol 2014, 44: 1073–1077.
Alexander GE. Biology of Parkinson’s disease: pathogenesis and pathophysiology of a multisystem neurodegenerative disorder. Dialogues Clin Neurosci 2004, 6: 259–280.
Varanese S, Birnbaum Z, Rossi R, Di Rocco A. Treatment of advanced Parkinson’s disease. Parkinson’s Dis 2011, 2010.
Werner FM, Covenas R. Classical neurotransmitters and neuropeptides involved in Parkinson’s disease: focus on anti-Parkinsonian drugs. Curr Drug Ther 2015, 10: 66-81
Aosaki T, Miura M, Suzuki T, Nishimura K, Masuda M. Acetylcholine–dopamine balance hypothesis in the striatum: An update. Geriatr Gerontol Int 2010, 10(s1): S148–157.
Huang LZ, Grady SR, Quik M. Nicotine reduces L-DOPA-induced dyskinesias by acting at β2* nicotinic receptors. J Pharmacol Exp Ther 2011, 338: 932–941.
Bédard C, Wallman MJ, Pourcher E, Gould PV, Parent A, Parent M. Serotonin and dopamine striatal innervation in Parkinson’s disease and Huntington’s chorea. Parkinsonism Relat Disord 2011, 17: 593–598.
Jaeger D, Kita H. Functional connectivity and integrative properties of globus pallidus neurons. Neuroscience 2011, 198: 44–53.
Werner FM, Coveñas R. Classical neurotransmitters and neuropeptides involved in generalized epilepsy: a focus on antiepileptic drugs. Curr Med Chem2011, 18: 4933–4948.
Delenclos M, Jones DR, McLean PJ, Uitti RJ. Biomarkers in Parkinson’s disease: Advances and strategies. Parkinsonism Relat Disord 2016, 22: S106–110.
Sharma S, Moon CS, Khogali A, Haidous A, Chabenne A, Ojo C, et al. Biomarkers in Parkinson’s disease (recent update). Neurochem Int 2013, 63: 201–229.
Politis M. Neuroimaging in Parkinson disease: from research setting to clinical practice. Nat Rev Neurol 2014, 10: 708–722.
Oravivattanakul S, Benchaya L, Wu G, Ahmed A, Itin I, Cooper S, et al. Dopamine transporter (DaT) scan utilization in a movement disorder center. Mov Disord Clin Pract, 3: 31–35.
Seifert KD, Wiener JI. The impact of DaTscan on the diagnosis and management of movement disorders: A retrospective study. Am J Neurodegener Dis 2013, 2: 29–34.
Niccolini F, Politis M. A systematic review of lessons learned from PET molecular imaging research in atypical parkinsonism. Eur J Nucl Med Mol Imaging 2016, 43: 2244–2254.
Calabria FF, Calabria E, Gangemi V, Cascini GL. Current status and future challenges of brain 18 imaging with F-DOPA PET for movement disorders. Hell J Nucl Med 2016, 19: 33–41.
Pikstra AR, van der Hoorn A, Leenders KL, de Jong BM. Relation of 18-F-Dopa PET with hypokinesia-rigidity, tremor and freezing in Parkinson’s disease. NeuroImage 2016, 11: 68–72.
Brown WD, Taylor MD, Roberts AD, Oakes TR, Schueller MJ, Holden JE, et al. FluoroDOPA PET shows the nondopaminergic as well as dopaminergic destinations of levodopa. Neurology 1999, 53: 1212.
Školoudík D, Jelínková M, Blahuta J, Čermák P, Soukup T, Bártová P, et al. Transcranial sonography of the substantia nigra: digital image analysis. Am J Neuroradiol 2014, 35: 2273–2278.
Bouwmans AE, Vlaar AM, Mess WH, Kessels A, Weber WE. Specificity and sensitivity of transcranial sonography of the substantia nigra in the diagnosis of Parkinson’s disease: prospective cohort study in 196 patients. BMJ Open 2013, 3: e002613.
Sian‐Hülsmann J, Mandel S, Youdim MB, Riederer P. The relevance of iron in the pathogenesis of Parkinson’s disease. J Neurochem 2011, 118: 939–957.
Ayton S, Lei P. Nigral iron elevation is an invariable feature of Parkinson’s disease and is a sufficient cause of neurodegeneration. Biomed Res Int 2014, 2014.
Badea L, Onu M, Wu T, Roceanu A, Bajenaru O. Nonreproducible connectome changes hint at functional heterogeneity of Parkinson’s Disease. arXiv preprint arXiv: 1611.04794 2016.
Pyatigorskaya N, Gallea C, Garcia-Lorenzo D, Vidailhet M, Lehericy S. A review of the use of magnetic resonance imaging in Parkinson’s disease. Ther Adv Neurol Disord 2014, 7: 206–20.
Berg D, Steinberger JD, Warren Olanow C, Naidich TP, Yousry TA. Milestones in magnetic resonance imaging and transcranial sonography of movement disorders. Mov Disord 2011, 26: 979–992.
Satue M, Obis J, Rodrigo MJ, Otin S, Fuertes MI, Vilades E, et al. Optical coherence tomography as a biomarker for diagnosis, progression, and prognosis of neurodegenerative diseases. J Ophthalmol 2016, 2016: 8503859.
Normando EM, Davis BM, De Groef L, Nizari S, Turner LA, Ravindran N, et al. The retina as an early biomarker of neurodegeneration in a rotenone-induced model of Parkinson’s disease: evidence for a neuroprotective effect of rosiglitazone in the eye and brain. Acta Neuropathol Commun 2016, 4: 86.
Parnetti L, Castrioto A, Chiasserini D, Persichetti E, Tambasco N, El-Agnaf O, et al. Cerebrospinal fluid biomarkers in Parkinson disease. Nat Rev Neurol 2013, 9: 131–140.
Jiménez-Jiménez FJ, Alonso-Navarro H, García-Martín E, Agundez JA. Cerebrospinal fluid biochemical studies in patients with Parkinson’s disease: toward a potential search for biomarkers for this disease. Front Cell Neurosci 2014, 11: 8.
Hall S, Surova Y, Öhrfelt A, Zetterberg H, Lindqvist D, Hansson O. CSF biomarkers and clinical progression of Parkinson disease. Neurology 2015, 84: 57–63.
Cabezas R, Avila MF, Torrente D, El-Bachá RS, Morales L, Gonzalez J, et al. Astrocytes role in Parkinson: a double-edged sword. Neurodegener Dis 2013, 10(5772): 54305.
Maragakis NJ, Rothstein JD. Mechanisms of disease: astrocytes in neurodegenerative disease. Nat Clin Pract Neurol 2006, 2: 679–689.
Magdalinou N, Lees AJ, Zetterberg H. Cerebrospinal fluid biomarkers in parkinsonian conditions: an update and future directions. J Neurol Neurosurg Psychiatry 2014, 85: 1065–1075.
Mayer CA, Brunkhorst R, Niessner M, Pfeilschifter W, Steinmetz H, Foerch C. Blood levels of glial fibrillary acidic protein (GFAP) in patients with neurological diseases. PLoS One 2013, 8: e62101.
Jiménez-Jiménez FJ, Alonso-Navarro H, García-Martín E, Agundez JA. Cerebrospinal fluid biochemical studies in patients with Parkinson’s disease: toward a potential search for biomarkers for this disease. Front Cell Neurosci 2014, 11: 8.
Yang Z, Wang KK. Glial fibrillary acidic protein: from intermediate filament assembly and gliosis to neurobiomarker. Trends Neurosci 2015, 38: 364–374.
Plog BA, Dashnaw ML, Hitomi E, Peng W, Liao Y, Lou N, et al. Biomarkers of traumatic injury are transported from brain to blood via the glymphatic system. J Neurosci 2015, 35: 518–526.
Saito Y. Oxidized DJ-1 as a possible biomarker of Parkinson’s disease. J Clin Biochem Nutr 2014, 54: 138–144.
Ariga H, Takahashi-Niki K, Kato I, Maita H, Niki T, Iguchi-Ariga SM. Neuroprotective function of DJ-1 in Parkinson’s disease. Oxid Med Cell Longev 2013, 2013: 683920.
Shen L, Ji HF. Low uric acid levels in patients with Parkinson’s disease: evidence from meta-analysis. BMJ Open 2013, 3: e003620.
Tian Y, Chen K, Xie Z, Fang Y, Wang H, Nie Y, et al. The association between serum uric acid levels, metabolic syndrome and cardiovascular disease in middle aged and elderly Chinese: results from the DYSlipidemia International Study. BMC Cardiovasc Disord 2015, 15: 66
Costa A, Peppe A, Carlesimo GA, Zabberoni S, Scalici F, Caltagirone C, et al. Brain-derived neurotrophic factor serum levels correlate with cognitive performance in Parkinson’s disease patients with mild cognitive impairment. Front Behav Neurosci 2015, 9: 253.
Wennström M, Surova Y, Hall S, Nilsson C, Minthon L, Boström F, et al. Low CSF levels of both α-synuclein and the α-synuclein cleaving enzyme neurosin in patients with synucleinopathy. PLoS One 2013, 8: e53250
Marti G, Saez N, Corominas M, Cuberas G, Lorenzo C, De Fabregues O, et al. Nigrostriatal degeneration and serum Bdnf levels in patients with “de novo” untreated Parkinson’s disease. Mov Disord 2016, 31: S402.
Khalil H, Alomari MA, Khabour OF, Al-Hieshan A, Bajwa JA. Circulatory levels of Bdnf correlate with cognitive deficits in people with Parkinson’s disease. Mov Disord 2016, 31: S458.
Braissant O. Neurofilament proteins in brain diseases. In: Arlen RK (Ed.). New Research on Neurofilament Proteins. Nova Science Publishers 2007: 25–51.
Vågberg M, Norgren N, Dring A, Lindqvist T, Birgander R, Zetterberg H, et al. Levels and age dependency of neurofilament light and glial fibrillary acidic protein in healthy individuals and their relation to the brain parenchymal fraction. PLoS One 2015, 10: e0135886.
Dias V, Junn E, Mouradian MM. The role of oxidative stress in Parkinson’s disease. J Parkinson’s Dis 2013, 3: 461–491.
Mischley LK, Standish LJ, Weiss NS, Padowski JM, Kavanagh TJ, White CC, et al. Glutathione as a biomarker in Parkinson’s disease: associations with aging and disease severity. Oxid Med Cell Longev 2016, 2016: 9409363.
Mischley LK, Allen J, Bradley R. Coenzyme Q10 deficiency in patients with Parkinson’s disease. J Neurol Sci 2012, 318: 72–75.
Fedorow H, Tribl F, Halliday G, Gerlach M, Riederer P, Double KL. Neuromelanin in human dopamine neurons: comparison with peripheral melanins and relevance to Parkinson’s disease. Prog Neurobiol 2005, 75: 109–124.
Greco G. Neuromelanin and Parkinson’s disease. In: Kostrzewa RM (Ed.). Handbook of Neurotoxicity. New York: Springer, 2014: 913–932.
Lehericy S, Sharman MA, Dos Santos CL, Paquin R, Gallea C. Magnetic resonance imaging of the substantia nigra in Parkinson’s disease. Mov Disord 2012, 27: 822–830.
Nakamura K, Sugaya K. Neuromelanin-sensitive magnetic resonance imaging: a promising technique for depicting tissue characteristics containing neuromelanin. Neural Regen Res 2014, 9: 759.
Rozycka A, Jagodzinski P, Kozubski W, Lianeri M, Dorszewska J. Homocysteine level and mechanisms of injury in Parkinson’s disease as related to MTHFR, MTR, and MTHFD1 genes polymorphisms and L-Dopa treatment. Curr Genomics 2013, 14: 534–542.
Doherty GH. Homocysteine and Parkinson’s disease: a complex relationship. J Neurol Disord 2013, 1: 107.
Desforges NM, Hebron ML, Algarzae NK, Lonskaya I, Moussa CE. Fractalkine mediates communication between pathogenic proteins and microglia: implications of anti-inflammatory treatments in different stages of neurodegenerative diseases. Int J Alzheimers Dis 2012, 2012: 345472.
Wennström M, Surova Y, Hall S, Nilsson C, Minthon L, Boström F, et al. Low CSF levels of both α-synuclein and the α-synuclein cleaving enzyme neurosin in patients with synucleinopathy. PLoS One 2013, 8: e53250
Barone P et al. PRIAMO study group. The PRIAMO study: A multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov Disord 2009, 24: 1641–1649
Sharma S, Moon CS, Khogali A, Haidous A, Chabenne A, Ojo C, Jelebinkov M, Kurdi Y, Ebadi M. Biomarkers in Parkinson’s disease (recent update). Neurochem Int 2013, 63: 201–229.
Fekete R, Jankovic J. Revisiting the relationship between essential tremor and Parkinson’s disease. Mov Disord 2011, 26: 391–398.
Aarsland D, Brønnick K, Alves G, Tysnes OB, Pedersen KF, Ehrt U, et al. The spectrum of neuropsychiatric symptoms in patients with early untreated Parkinson’s disease. J Neurol Neurosurg Psychiatry 2009, 80: 928–930
Monderer R, Thorpy M. Sleep disorders and daytime sleepiness in Parkinson’s disease. Curr Neurol Neurosci Rep 2009, 9: 173–180
Ross GW, Petrovitch H, Abbott RD, Tanner CM, Popper J, Masaki K, et al. Association of olfactory dysfunction with risk for future Parkinson’s disease. Ann Neurol 2008, 63 : 167–173
Goldstein DS, Holmes C, Bentho O, Sato T, Moak J, Sharabi Y, et al. Biomarkers to detect central dopamine deficiency and distinguish Parkinson disease from multiple system atrophy. Parkinsonism Relat Disord 2008, 14: 600–607.
Michell AW, Xu Z, Fritz D, Lewis SJ, Foltynie T, Williams-Gray CH, et al. Saccadic latency distributions in Parkinson’s disease and the effects of L-dopa. Exp Brain Res 2006, 174: 7–18.
Blair HA, Dhillon S. Safinamide: A review in Parkinson’s disease. CNS Drugs 2017, 31: 169–176.
Wang CD, Chan P. Clinicogenetics of Parkinson’s disease: a drawing but not completed picture. Neuroimmunol Neuroinflammation 2014, 1: 115.
Siddiqui IJ, Pervaiz N, Abbasi AA. The Parkinson Disease gene SNCA: Evolutionary and structural insights with pathological implication. Sci Rep 2016, 6.
Oczkowska A, Kozubski W, Lianeri M, Dorszewska J. Mutations in PRKN and SNCA genes important for the progress of Parkinson’s disease. Curr Genomics 2013, 14: 502–517.
Kobo H, Bar-Shira A, Dahary D, Gan-Or Z, Mirelman A, Goldstein O, et al. Down-regulation of B cell-related genes in peripheral blood leukocytes of Parkinson’s disease patients with and without GBA mutations. Mol Genet Metab 2016, 117: 179–185.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lotankar, S., Prabhavalkar, K.S. & Bhatt, L.K. Biomarkers for Parkinson’s Disease: Recent Advancement. Neurosci. Bull. 33, 585–597 (2017). https://doi.org/10.1007/s12264-017-0183-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12264-017-0183-5