Abstract
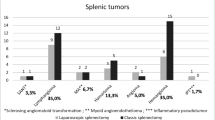
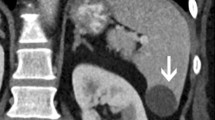
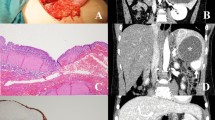
The aim of this study is to consider the management of incidentally diagnosed splenic masses. Patients who underwent splenectomy between September 2005 and February 2015 were analyzed retrospectively. Patients with the history of lymphoproliferative disease were excluded. Radiologic evaluation was done in all patients. Preoperative tru-cut biopsies were performed on three patients. The patients were grouped according to the nature of the splenic mass such as cystic, benign, and malign lesions. The groups were compared according to age, gender, tumor size, and the number of lesions. There were 13 male and 12 female patients with the median age of 52 years (range 15–84 years). The final pathology revealed cyst in 7 patients (28.0%), benign lesion in 7 patients (28.0%), and malign lesion in 11 patients (44%). The results of tru-cut biopsies were similar with postoperative pathologies. Solitary lesions were detected in 15 patients, and there were multiple lesions in 10 cases. There was not a significant difference between the tumor sizes of malign vs. benign lesions (p = 0.42). Malignancy was a higher trend in multiple lesions (p = 0.06). Advanced radiologic imaging studies and more frequent and reliable use of percutaneous diagnostic procedures may limit the number of unnecessary splenectomies especially for benign lesions.
Similar content being viewed by others
References
Gaetke-Udager K, Wasnik AP, Kaza RK et al (2014) Multimodality imaging of splenic lesions and the role of non-vascular, image-guided intervention. Abdom Imaging 39:570–587
Friedlander MA, Wei XJ, Iyengar P et al (2008) Diagnostic pitfalls in fine needle aspiration biopsy of the spleen. Diagn Cytopathol 36:69–75
Falk S, Krishnan J, Meis JM (1993) Primary angiosarcoma of the spleen. A clinicopathologic study of 40 cases. Am J Surg Pathol 17:959–970
Kaza RK, Azar S, Al-Hawary MM et al (2010) Primary and secondary neoplasms of the spleen. Cancer Imaging 10:173–182
Lam KY, Tang V (2000) Metastatic tumors to the spleen: a 25-year clinicopathologic study. Arch Pathol Lab Med 124:526–530
Schon CA, Gorg C, Ramaswamy A et al (2006) Splenic metastases in a large unselected autopsy series. Pathol Res Pract 202:351–356
Fowler RH (1953) Cystic tumours of the spleen. Int Abstr Surg 96:209–227
Morgenstern L (2002) Nonparasitic splenic cysts: pathogenesis, classification, and treatment. J Am Coll Surg 194:306–314
Gianom D, Wildisen A, Hotz T et al (2003) Open and laparoscopic treatment of nonparasitic splenic cysts. Dig Surg 20:74–78
Thipphavong S, Duigenan S, Schindera ST et al (2014) Nonneoplastic, benign, and malignant splenic diseases: cross-sectional imaging findings and rare disease entities. AJR Am J Roentgenol 203:315–322
Gómez-Rubio M, López-Cano A, Rendón P et al (2009) Safety and diagnostic accuracy of percutaneous ultrasound-guided biopsy of the spleen: a multicenter study. J Clin Ultrasound 37:445–450
Handa U, Tiwari A, Singhal N et al (2013) Utility of ultrasound-guided fine-needle aspiration in splenic lesions. Diagn Cytopathol 41:1038–1042
Cuervo JL, Buela E (2007) Splenic epidermoid cyst: laparoscopic partial decapsulation. Circ Pediatr 20:63–67
Szczepanik AB, Meissner AJ (2009) Partial splenectomy in the management of nonparasitic splenic cysts. World J Surg 33:852–856
Gochhait D, Dey P, Rajwanshi A et al (2015) Role of fine needle aspiration cytology of spleen. APMIS 123:190–193
Adas G, Karatepe O, Altiok M et al (2009) Diagnostic problems with parasitic and non-parasitic splenic cysts. BMC Surg 9:9
Ruiz-Fernandez M, Guerra-Vales MJ, Enguita-Valls A et al (2008) Splenic hydatid cyst, a rare location of extrahepatic echinococcosis: report of six cases. European Journal of Internal Medicine 19:51–53
Moir C, Guttman F, Jequier S et al (1989) Splenic cysts: aspiration, sclerosis, or resection. J Pediatr Surg 24:646–648
Goktay AY, Secil M, Ozcan MA et al (2006) Percutaneous treatment of congenital splenic cysts: drainage and sclerotherapy with polidocanol. Cardiovasc Intervent Radiol 29:469–472
Kamaya A, Weinstein S, Desser TS (2006) Multiple lesions of the spleen: differential diagnosis of cystic and solid lesions. Semin Ultrasound CT MR 27:389–403
Abbott RM, Levy AD, Aguilera NS et al (2004) From the archives of the AFIP: primary vascular neoplasms of the spleen: radiologic-pathologic correlation. Radiographics 24:1137–1163
Sim J, Ahn HI, Han H et al (2013) Splenic hamartoma: a case report and review of the literature. World J Clin Cases 1:217–219
Kakisaka T, Kamiyama T, Yokoo H et al (2014) Hand-assisted laparoscopic splenectomy for sclerosing angiomatoid nodular transformation of the spleen complicated by chronic disseminated intravascular coagulation: a case report. Asian J Endosc Surg 7:275–278
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the ethics committee.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yuksel, U.M., Turanli, S., Berberoglu, A.U. et al. Management of Incidentally Diagnosed Splenic Masses. Indian J Surg 80, 318–321 (2018). https://doi.org/10.1007/s12262-016-1582-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12262-016-1582-y