Abstract
Background
Survival after cardiopulmonary resuscitation (CPR) using standard vasopressor therapy is disappointing. Vasopressin is a potent vasopressor that could become a useful therapeutic alternative in the treatment of cardiac arrest.
Aims
The aim of this prehospital prospective cohort study was to assess the influence of treatment with vasopressin and hydroxyethyl starch solution (HHS) on outcome in resuscitated blunt trauma patients with pulseless electrical activity (PEA) cardiac arrest.
Methods
Two treatment groups of resuscitated trauma patients in cardiac arrest were compared: in the epinephrine group patients received epinephrine 1 mg IV every 3 min only; in the vasopressin group patients first received hypertonic HHS and arginine vasopressin 40 units IV only or followed by epinephrine 1 mg every 3 min until cessation of CPR. Medical trauma care was provided according to advanced trauma life support (ATLS) guidelines.
Results
The study included 31 patients and there were no significant demographic or clinical differences between the treatment groups. Significantly more circulatory restorations [11/13 (85%) vs 3/18 (17%); P < 0.01] and better 24-h survival rates [8/13 (62%) vs 2/18 (11%); P = 0.001] were observed in the vasopressin group. Average mean arterial pressure (100.4 ± 11.4 mmHg vs 80.3 ± 12.4 mmHg) and final end-tidal partial pressure of carbon dioxide (PETCO2) at admission (4.5 ± 0.9 kPa vs 2.8 ± 0.4 kPa) were also higher in the vasopressin group.
Conclusion
Our results suggest that victims of severe blunt trauma with PEA should be initially treated with vasopressin in combination with HHS volume resuscitation followed by standard resuscitation therapy and other procedures when appropriate. Vasopressin might be potentially lifesaving in blunt trauma cardiac arrest compared to standard treatment with epinephrine.
Similar content being viewed by others
Introduction
Survival after cardiopulmonary resuscitation (CPR) using standard vasopressor therapy is disappointing. Side effects of epinephrine such as increased myocardial oxygen demand and consumption, decreased myocardial ATP with proarrhythmic effects, or increased intrapulmonary shunting and myocardial dysfunction during the post-resuscitation period are well known [1, 2]. Vasopressin is a potent vasopressor that could become a useful therapeutic alternative in the treatment of cardiac arrest, because it significantly improves total cerebral and left myocardial blood flow, and it causes a sustained increase in mean arterial blood pressure as compared with maximal doses of epinephrine. Recent studies have shown that during CPR vasopressin is especially beneficial when combined with epinephrine [3–6]. Survival after traumatic cardiac arrest is very poor, and some consider resuscitation of such patients futile, especially in patients with hypovolemia as the primary cause of arrest [7–12]. In spite of that some studies were performed [13–15] in which successful hemodynamic stabilization occurred using vasopressin in uncontrolled hemorrhagic shock and during traumatic CPR.
We conducted a clinical investigation to assess the effect of vasopressin and hydroxyethyl starch solution (HHS) on outcome of out-of-hospital CPR in blunt trauma patients, who had pulseless electrical activity (PEA) cardiac arrest.
Our hypothesis was that vasopressin improves outcome in PEA cardiac arrest caused by blunt trauma.
Patients and methods
We undertook a prospective observational cohort study, with a retrospective control group, in a prehospital setting, after approval had been granted by the Ethics Review Board of the Ministry of Health of Slovenia. The study design of a prospective cohort with retrospective historical controls is useful as forming the basis for recommending prospective multicenter trials on an important issue. The study community, in the region surrounding the city of Maribor in Slovenia, includes a population of 190,000, and approximately 90 resuscitations are attempted per year. Initial basic and advanced cardiac life support is provided by emergency doctors before the patient’s arrival at the hospital (prehospital emergency unit), applying a regional protocol that incorporates European Resuscitation Council standards, guidelines, and clinical algorithms for CPR.
This study included trauma patients in cardiac arrest with registered initial PEA < 40 waves/min only. Two groups of resuscitated patients were compared. Patients in group 1 received epinephrine 1 mg every 3 min only (data were collected from January 1998 to November 2002). Patients in group 2 first received 40 IU of arginine vasopressin from 250 ml Pitressin™ formulation (Goldshield Pharmaceuticals, Croydon, UK) in combination with HHS 4 ml/kg, followed by epinephrine 1 mg every 3 min if circulation was not restored before (data were collected from December 2002 to December 2006). All drugs were injected as an intravenous bolus followed by 20 ml of normal saline. Exclusion criteria were age under 18 years, documented terminal illness, nontraumatic cardiac arrest, and severe hypothermia (< 30°C). Diagnoses were confirmed in the intensive care unit, or, for those patients who died at the scene, at autopsy. The data regarding CPR in the prehospital setting were collected in accordance with directions presented by the International Liaison Committee on Resuscitation (ILCOR) Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes.
Data are expressed as mean ± standard deviation or number (%). Comparisons between groups were performed using Fisher’s exact test for categorical data and Wilcoxon’s rank sum test for numerical data. The null hypothesis was considered to be rejected at P values less than 0.05. Multiple logistic regression analysis was done to examine the relationship between survival and application of vasopressin, adjusting for age, sex, time elapsed before CPR, time of resuscitation by the medical team, witnessed arrest, and basic life support by bystanders. The results are expressed as odds ratio with 95% confidence interval. All analyses were conducted using SPSS version 12.0 software (SPSS, Inc., Chicago, IL, USA).
Results
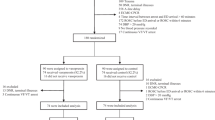
A Utstein reporting template for out-of-hospital cardiac arrest in Maribor obtained in a 9-year period is show in Fig. 1.
The study included 31 patients and there were no significant demographic or clinical differences between the groups regarding gender, age, first monitored rhythm, location of arrest, arrest witnessed, bystander CPR, response time, initial end-tidal partial pressure of carbon dioxide (PETCO2) and Injury Severity Score (ISS) at admission (Table 1). There were 18 patients in the epinephrine group 1 and 13 patients in the vasopressin group 2.
In the vasopressin group significantly more restorations of circulation [11/13 (85%) vs 3/18 (17%); P < 0.01] and better 24-h survival rates [8/13 (62%) vs 2/18 (11%); P = 0.001] were observed.
The discharge rate from hospital was also better, but not statisticallly significant, in the vasopressin group [4/13 (31%) vs 1/18 (6%); P = 0.13] (Table 1).
Average final mean arterial pressure (MAP) at admission to hospital was higher in the vasopressin group (100.4 ± 11.4 mmHg) compared to the epinephrine group (80.3 ± 12.4 mmHg). Final PETCO2 was also higher in the vasopressin group (4.5 ± 0.9 kPa vs 2.8 ± 0.4 kPa; P < 0.01) (Table 1). In the vasopressin group seven patients received only vasopressin 40 IU and nine patients received additional epinephrine therapy.
The variables associated with restoration of spontaneous circulation (ROSC) were: response time, witnessed arrest, bystander CPR, average dose of epinephrine, ISS, initial and average PETCO2, and vasopressin therapy (Table 2). The variables associated with survival and hospital discharge were: response time, witnessed arrest, bystander CPR, average dose of epinephrine, initial and average PETCO2, initial and final MAP, and ISS (Table 3).
Discussion
Our research supports the role of vasopressin as an efficient vasopressor during out-of-hospital CPR in blunt trauma patients, who are in cardiac arrest with initial PEA. In our previous studies about prehospital CPR we established the relationship between PETCO2, MAP, and the prognosis [5, 6]. The average and final PETCO2 in vasopressin-treated patients with ROSC were significantly higher as well as the initial and the final MAP values. Therefore, vasopressin could be more potent than epinephrine in increasing the cardiac output. Results from the study by Bell and colleagues [16] indicate that to secure cerebral perfusion and prevent secondary cerebral injury MAP should be kept at a level higher than commonly accepted. In our study, MAP was kept at a normal level (approximately 100 mmHg), thus securing coronary perfusion and preserving cerebral perfusion in the critical post-resuscitation period of absent cerebral autoregulation.
Some studies confirmed that the traumatic cardiac or pulmonary arrest is often associated with a dismal outcome and is considered to be an example of medical futility and inappropriate use of resources [7–11]. On other hand, the use of guidelines regarding the termination or withholding of CPR in traumatic cardiac arrest patients remains controversial because several survivors met criteria for nontreatment according to the proposed clinical guidelines [8, 12]. Vasopressin is a promising agent in the treatment of traumatic cardiac arrest, especially in hemorrhagic shock [17]. Voelckel et al. in two experimental studies [13, 14] concluded that treatment of hypovolemic cardiac arrest with vasopressin, but not epinephrine, resulted in sustained vital organ perfusion with less metabolic acidosis in the post-resuscitation phase, decreased gut perfusion in the post-resuscitation phase without impairing renal function, and subsequently in improved survival. Similarly, Sanui et al. [15, 18] have found that early supplemental arginine vasopressin (AVP) rapidly corrected cerebral perfusion pressure, improved cerebrovascular compliance, and prevented circulatory collapse during fluid resuscitation of hemorrhagic shock after traumatic brain injury. In severe chest trauma early AVP decreased mortality, reduced fluid requirements, improved pulmonary function, and did not increase the risk for bleeding in uncontrolled hemorrhage [19]. In case reports of uncontrolled hemorrhagic shock with subsequent cardiac arrest some authors confirmed these results [20, 21].
The study by Friesenecker and colleagues [22] showed that, under normal physiological conditions, vasopressin exerted significantly stronger vasoconstriction on large arterioles than norepinephrine.
This observation could explain, in part, why vasopressin can be effective in advanced shock unresponsive to therapeutic increases of catecholamines. In a clinical study, Westerman et al. [23] confirmed significantly increased levels of endogenous vasopressin in multiple trauma patients.
That seems to be an integral part of the neuroendocrine response to severe injury; therefore, the natural response to trauma may be enhanced by additional exogenous vasopressin. Some clinical observations suggest that endogenous vasopressin insufficiency may be an underlying mechanism of refractory hypotension after prolonged hemorrhagic shock. Another beneficial effect of vasopressin may be that the blood is shifted away from a subdiaphragmatic region to the heart and brain, thus optimizing vital organ perfusion. This effect of vasopressin may be especially lifesaving in patients with uncontrolled hemorrhage resulting from subdiaphragmatic injury [24–28]. In the historical group, resuscitation efforts lasted longer and a significantly higher quantity of additional epinephrine was needed. Adrenergic stimulation by additional doses of epinephrine is associated with adverse cardiac effects, including post-resuscitation myocardial dysfunction and increased myocardial oxygen consumption. In our trial in the vasopressin group we combined vasopressin with hypertonic HHS. Søreide and Deakin reported [29] that the ideal prehospital fluid regimen may be a combination of an initial hypertonic solution given as a 10- to 20-min infusion, followed by crystalloids, and in some cases, artificial colloids. Meybohm et al. [27, 30] suggested the combination of HHS and vasopressin during the initial 10 min of therapy; cerebral perfusion pressure of the HHS group was significantly higher compared to the fluid group and increased more rapidly in the HHS with vasopressin group. HHS has a positive effect on hemodynamic parameters (systemic vascular resistence index, pulmonary vascular resistence index), microcirculation, and oxygen transport [31]. The interesting study of Giusti-Paiva et al. can explain one additional synergistic effect of HHS and vasopressin [32]. In this study they confirmed the effects of hypertonic saline solution administration on vasopressin secretion and mean arterial pressure in endotoxic shock. The hypertonic saline administration was followed by an immediate recovery of blood pressure and also by an increase in plasma vasopressin levels compared with isotonic saline solution. The vasopressin V1 receptor antagonist blocked the pressor response to hypertonic saline solution. These data suggest that the recovery of blood pressure after hypertonic saline solution administration during endotoxic shock is mediated by vasopressin secretion. Maybe a similar mechanism was responsible for the positive effect of HHS and vasopressin in traumatic cardiac arrest. The higher initial MAP after ROSC and lower average dose of epinephrine and average volume of resuscitation (without HHS) with similar ISS in both groups suggest that vasopressin could be more potent than epinephrine in increasing the cardiac output.
This small study has all the inherent problems associated with observational studies, but despite these limitations suggests a resuscitation strategy involving vasopressin in combination with HHS as a potentially lifesaving treatment in blunt trauma cardiac arrest. Our observations should be confirmed in future by larger multicenter prospective clinical trials.
Conclusion
Survival after traumatic cardiac arrest is in general extremely rare. Our study showed better short-term survival in blunt trauma patients with PEA cardiac arrest, who were resuscitated using vasopressin in combination with HHS. Variables associated with survival and hospital discharge were: response time, witnessed arrest, bystander CPR, initial and average PETCO2, initial and final MAP, and ISS. Vasopressin in combination with HHS might be potentially lifesaving in blunt trauma cardiac arrest compared to standard treatment with epinephrine.
References
Thrush DN, Downs JB, Smith RA (1997) Is epinephrine contraindicated during cardiopulmonary resuscitation? Circulation 96:2709–2714
Paradis NA, Wenzel V, Southall J (2002) Pressor drugs in the treatment of cardiac arrest. Cardiol Clin 20:61–78
Wenzel V, Lindner KH (2006) Vasopressin combined with epinephrine during cardiac resuscitation: a solution for the future? Crit Care 10:125
Krismer AC, Wenzel V, Stadlbauer KH, Mayr VD, Lienhart HG, Arntz HR, Lindner KH (2004) Vasopressin during cardiopulmonary resuscitation: a progress report. Crit Care Med 32(9 Suppl):S432–S435
Grmec S, Mally S (2006) Vasopressin improves outcome in out-of-hospital cardiopulmonary resuscitation of ventricular fibrillation and pulseless ventricular tachycardia: a observational cohort study. Crit Care 10:R13
Mally S, Jelatancev A, Grmec S (2007) Effects of epinephrine and vasopressin on end-tidal carbon dioxide tension and mean arterial blood pressure in out-of-hospital cardiopulmonary resuscitation: an observational study. Crit Care 11:R39
Lockey D, Crewdson K, Davies G (2006) Traumatic cardiac arrest: who are the survivors? Ann Emerg Med 48(3):240–244
Willis CD, Cameron PA, Bernard SA, Fitzgerald M (2006) Cardiopulmonary resuscitation after traumatic cardiac arrest is not always futile. Injury 37(5):448–454
Alanezi K, Alanzi F, Faidi S, Sprague S, Cadeddu M, Baillie F, Bowser D, McCallum A, Bhandari M (2004) Survival rates for adult trauma patients who require cardiopulmonary resuscitation. CJEM 6(4):263–265
Huber-Wagner S, Lefering R, Qvick M, Kay MV, Paffrath T, Mutschler W, Kanz KG, Working Group on Polytrauma of the German Trauma Society (DGU) (2007) Outcome in 757 severely injured patients with traumatic cardiorespiratory arrest. Resuscitation 75(2):276–285
Pickens JJ, Copass MK, Bulger EM (2005) Trauma patients receiving CPR: predictors of survival. J Trauma 58(5):951–958
Hopson LR, Hirsh E, Delgado J, Domeier RM, McSwain NE, Krohmer J, National Association of EMS Physicians Standards and Clinical Practice Committee, American College of Surgeons Committee on Trauma (2003) Guidelines for withholding or termination of resuscitation in prehospital traumatic cardiopulmonary arrest. J Am Coll Surg 196(3):475–481
Voelckel WG, Lurie KG, Lindner KH, Zielinski T, McKnite S, Krismer AC, Wenzel V (2000) Vasopressin improves survival after cardiac arrest in hypovolemic shock. Anesth Analg 91:627–634
Voelckel WG, Lurie KG, McKnite S, Zielinski T, Lindstrom P, Peterson C, Wenzel V, Lindner KH (2001) Comparison of epinephrine with vasopressin on bone marrow blood flow in an animal model of hypovolemic shock and subsequent cardiac arrest. Crit Care Med 29(8):1587–1592
Sanui M, King DR, Feinstein AJ, Varon AJ, Cohn SM, Proctor KG (2006) Effects of arginine vasopressin during resuscitation from hemorrhagic hypotension after traumatic brain injury. Crit Care Med 34(2):433–438
Bell DD, Brindley PG, Forrest D, Al Muslim O, Zygun D (2005) Management following resuscitation from cardiac arrest: recommendations from the 2003 Rocky Mountain Critical Care Conference. Can J Anaesth 52:309–322
Krismer AC, Dünser MW, Lindner KH, Stadlbauer KH, Mayr VD, Lienhart HG, Arntz RH, Wenzel V (2006) Vasopressin during cardiopulmonary resuscitation and different shock states: a review of the literature. Am J Cardiovasc Drugs 6(1):51–68
Feinstein AJ, Patel MB, Sanui M, Cohn SM, Majetschak M, Proctor KG (2005) Resuscitation with pressors after traumatic brain injury. J Am Coll Surg 201(4):536–545
Feinstein AJ, Cohn SM, King DR, Sanui M, Proctor KG (2005) Early vasopressin improves short-term survival after pulmonary contusion. J Trauma 59(4):876–882
Tsuneyoshi I, Onomoto M, Yonetani A, Kanmura Y (2005) Low-dose vasopressin infusion in patients with severe vasodilatory hypotension after prolonged hemorrhage during general anesthesia. J Anesth 19(2):170–173
Krismer AC, Wenzel V, Voelckel WG, Innerhofer P, Stadlbauer KH, Haas T, Pavlic M, Sparr HJ, Lindner KH, Koenigsrainer A (2005) Employing vasopressin as an adjunct vasopressor in uncontrolled traumatic hemorrhagic shock. Three cases and a brief analysis of the literature. Anaesthesist 54(3):220–224
Friesenecker BE, Tsai AG, Martini J, Ulmer H, Wenzel V, Hasibeder WR, Intaglietta M, Dünser MW (2006) Arteriolar vasoconstrictive response: comparing the effects of arginine vasopressin and norepinephrine. Crit Care 10:R75
Westermann I, Dünser MW, Haas T, Jochberger S, Luckner G, Mayr VD, Wenzel V, Stadlbauer KH, Innerhofer P, Morgenthaler N, Hasibeder WR, Voelckel WG (2007) Endogenous vasopressin and copeptin response in multiple trauma patients. Shock 28:644–649
Stadlbauer KH, Wenzel V, Krismer AC, Voelckel WG, Lindner KH (2005) Vasopressin during uncontrolled hemorrhagic shock: less bleeding below the diaphragm, more perfusion above. Anesth Analg 101:830–832
Raedler C, Voelckel WG, Wenzel V, Krismer AC, Schmittinger CA, Herff H, Mayr VD, Stadlbauer KH, Lindner KH, Königsrainer A (2004) Treatment of uncontrolled hemorrhagic shock after liver trauma: fatal effects of fluid resuscitation versus improved outcome after vasopressin. Anesth Analg 98:1759–1766
Voelckel WG, Raedler C, Wenzel V, Lindner KH, Krismer AC, Schmittinger CA, Herff H, Rheinberger K, Königsrainer A (2003) Arginine vasopressin, but not epinephrine, improves survival in uncontrolled hemorrhagic shock after liver trauma in pigs. Crit Care Med 31:1160–1165
Meybohm P, Cavus E, Dörges V, Weber B, Stadlbauer KH, Wenzel V, Scholz J, Steffen M, Bein B (2008) Release of protein S100B in haemorrhagic shock: effects of small volume resuscitation combined with arginine vasopressin. Resuscitation 76:449–456
Stadlbauer KH, Wenzel V, Wagner-Berger HG, Krismer AC, Königsrainer A, Voelckel WG, Raedler C, Schmittinger CA, Lindner KH, Klima G (2007) An observational study of vasopressin infusion during uncontrolled haemorrhagic shock in a porcine trauma model: effects on bowel function. Resuscitation 72:145–148
Søreide E, Deakin CD (2005) Pre-hospital fluid therapy in the critically injured patient – a clinical update. Injury 36:1001–1010
Meybohn P, Cavus E, Bein B, Steinfath M, Weber B, Hamann C, Scholz J, Dörges V (2007) Small volume resuscitation: a randomized controlled trial with either norepinephrine or vasopressin during severe hemorrhage. J Trauma 62(3):640–646
Sirvinskas E, Sneider E, Svagzdiene M, Vaskelyte J, Raliene L, Marchertiene I, Adukauskiene D (2007) Hypertonic hydroxyethyl starch solution for hypovolaemia correction following heart surgery. Perfusion 22(2):121–127
Giusti-Paiva A, Martinez MR, Bispo-da-Silva LB, Salgado MC, Elias LL, Antunes-Rodrigues J (2007) Vasopressin mediates the pressor effect of hypertonic saline solution in endotoxic shock. Shock 27(4):416–421
Conflicts of interest
This article was presented in part as an oral presentation at the 12th International Conference on Emergency Medicine–ICEM 2008 in San Francisco. The abstract will be published in Annals of Emergency Medicine. Otherwise the authors declare that they have no conflict of interest regarding this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The views expressed in this paper are those of the author(s) and not those of the editors, editorial board or publisher.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Grmec, Š., Strnad, M., Čander, D. et al. A treatment protocol including vasopressin and hydroxyethyl starch solution is associated with increased rate of return of spontaneous circulation in blunt trauma patients with pulseless electrical activity. Int J Emerg Med 1, 311–316 (2008). https://doi.org/10.1007/s12245-008-0073-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12245-008-0073-8