Abstract
NUT midline carcinoma (NMC) is a rare and aggressive disease encountered in the midline of the head and neck or mediastinum. Due to its sparse incidence and subtle pathologic features, we aim to increase knowledge and awareness for this pathologic entity. We present an exemplary case of a young, healthy male presenting with oral cavity pain and cervical lymphadenopathy. This patient was initially diagnosed with an unspecified, highly aggressive sublingual gland malignancy and underwent locoregional resection with free flap reconstruction however suffered a rapid local recurrence and widely extensive metastasis within just 1 month. After rigorous analysis, final pathologic diagnosis revealed a poorly differentiated carcinoma with evidence of squamous differentiation that eventually, post-mortem tested positive for NMC. Only one prior case of sublingual gland NMC has been previously reported as we discuss the literature regarding all sublingual gland malignancies as well as the pathologic features and treatment options for NMC. We recommend consideration of testing for the NUT proto-oncogene at the time of biopsy in the clinical setting of a poorly differentiated midline carcinoma, especially with squamous differentiation, of the head or neck in order to identify patients for clinical trial enrollment and appropriately counsel on the poor clinical prognosis. Improving clinician awareness is critical to increase diagnostic accuracy and need to study prospective treatment outcomes as the first step toward improving management of this difficult disease.



Similar content being viewed by others
References
Carvalho AL, Nishimoto IN, Califano JA, Kowalski LP. Trends in incidence and prognosis for head and neck cancer in the United States: a site-specific analysis of the SEER database. Int J Cancer. 2005;114(5):806–816.
Spiro RH, Armstrong J, Harrison L, Geller NL, Lin S-Y, Strong EW. Carcinoma of major salivary glands. Recent trends. Arch Otolaryngol Head Neck Surg. 1989;115:316–332.
Lee RJ, Tong EL, Patel R, Satyadev N, Christensen RE. Malignant sublingual gland tumors: demographics, prognostic factors, and treatment outcomes. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121(2):180–187.
Rutt AL, Hawkshaw MJ, Lurie D, Sataloff RT. Salivary gland cancer in patients younger than 30 years. Ear Nose Throat J. 2011;90(4):174–184.
Andersen LJ, Therkildsen MH, Ockelmann HH, Bentzen JD, Schiødt T, Hansen HS. Malignant epithelial tumors in the minor salivary glands, the submandibular gland, and the sublingual gland. Prognostic factors and treatment results. Cancer. 1991;68(11):2431–2437.
Ellis GL, Auclair PL. Tumors of the salivary glands (series 4).Washington, DC: Armed Forces Institute of Pathology; 2008.
Jegadeesh NN. Outcomes and prognostic factors in modern era management of major salivary gland cancer. Oral Oncol. 2015;51(8):770–777.
French CA. The Importance of diagnosing NUT midline carcinoma. Head Neck Pathol. 2013;7(1):11–16.
French CA, Miyoshi I, Kubonishi I, et al. BRD4-NUT fusion oncogene: a novel mechanism in aggressive carcinoma. Cancer Res. 2003;63:304–307.
Andreasen S, French CA, Josiassen M, Hahn CH, Kiss K. NUT carcinoma of the sublingual gland. Head and Neck Pathol. 2016;10(3):362–366.
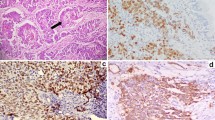
Haack H, Johnson LA, Fry CJ, et al. Diagnosis of NUT midline carcinoma using a NUT-specific monoclonal antibody. Am J Surg Pathol. 2009;33:984–991.
Bauer D, Mitchell C, Strait K, et al. Clinicopathologic features and long-term outcomes of NUT midline carcinoma. Clin Cancer Res. 2012;18:5773–5779.
den Bakker MA, Beverloo BH, van den Heuvel-Eibrink MM, et al. NUT midline carcinoma of the parotid gland with mesenchymal differentiation. Am J Surg Pathol. 2009;33:1253–1258.
Ziai J, French CA, Zambrano E. NUT gene rearrangement in a poorly-differentiated carcinoma of the submandibular gland. Head Neck Pathol. 2010;4:163–168.
Wartchow EP, Moore TS, French CA, et al. Ultrastructural features of NUT midline carcinoma. Ultrastruct Pathol. 2012;36:280–284.
Chau NG, Hurwitz S, Mitchell CM, et al. Intensive treatment and survival outcomes in NUT midline carcinoma of the head and neck. Cancer. 2016;122(23):3632–3640.
Hirvonen K, Back L, Saarilahti K, Leivo I, Hagstrom J, Makitie AA. Pattern of recurrent disease in major salivary gland adenocystic carcinoma. Virchows Arch. 2015;467:19–25.
Lawal AO, Adisa AO, Kolude B, Adeyemi BF. Malignant salivary gland tumours of the head and neck region: a single institutions review. Pan Afr Med J. 2015;20:121.
Maruse Y, Kawano S, Kiyoshima T, Goto Y, Matsubara R, Chikui T, Yoshiga D, Nakamura S. Case of mucoepidermoid carcinoma of the sublingual gland accompanied with extensive dystrophic calcification and intratumoral bone formation. Head Neck. 2015;37(11):E161–E164.
Roy L, Moubayed S, Ayad T. Lymphoepithelial carcnoma of the sublignual gland: case report and review of literature. J Oral Maxillofac Surg. 2015;(73(9):1878.e1–5.
Ban X, Wu J, Mo Y, et al. Lymphoepithelial carcinoma of the salivary gland: morphologic patterns and imaging features on CT and MRI. AJNR Am J Neuroradiol. 2014;35(9):1813–1819.
Leiser Y, Peled M, Wolff A, El-Naaj IA. Lymphoepithelial carcinoma: review of the treatment modalities and report of a rare case in the sublingual gland. J Oral Maxillofac Surg. 2014;72(4):828–828.
Mohanty S, Pathak H. Epithelial-myoepithelial carcinoma of floor of mouth: A case report with cytological, histological and immunohistochemical correlation. Natl J Maxillofac Surg. 2014;5(2):195–197.
Bradley PJ, McGurk M. Incidence of salivary gland neoplasms in a defined UK population. Br J Oral Maxillofac Surg. 2013;51(5):399–403.
Eichhorn W, Precht C, Wehrmann M, et al. First description of a hybrid tumor of the sublingual gland. Anticancer Res. 2013;33(10):4567–4571.
Fang QG, Shuang S, Li ZN, Zhang X, Liu FY, Sun CF. Epithelial salivary gland tumors in children: a twenty-five-year experience of 122 patients. Int J Pediatr Otorhinolaryngol. 2013;77(8):1252–1254.
Gillenwater AM, Frank SJ, Fatani H, El-Naggar AK. Primary intestinal-like adenocarcinoma of major salivary glands: 2 instances of previously undocumented phenotype. Head Neck. 2013;35(8):234–236.
Kim DW, Park HJ, Cha IH, Yang DH, Kim HS, Nam W. An atypical case of rare salivary malignancy, hyalinizing clear cell carcinoma. J Korean Assoc Oral Maxillofac Surg. 2013;39:283–288.
Lawal AO, Adisa AO, Kolude B, Adeyemi BF, Olajide MA. A review of 413 salivary gland tumours in the head and neck region. J Clin Exp Dent. 2013;5(5):e218–222.
Adirajaiah S, Anehosur V, Sumana, Gopalakrishnan K. Adenocarcinoma of the sublingual salivary gland: a case report. J Oral Biol Craniofac Res. 2012;2(3):206–209.
Ariyoshi Y, Shimahara M, Konda T, Tsuji M. Carcinoma ex pleomorphic adenoma of the sublingual gland: a case report. Int J Oral Sci. 2012;4(1):50–53.
Lukšić I, Virag M, Manojlović S, Macan D. Salivary gland tumours: 25 years of experience from a single institution in Croatia. J Craniomaxillofac Surg. 2012;40(3):e75–e81.
Bombeccari GP, Guzzi GP, Pallotti F, Spadari F. Mucoepidermoid carcinoma of the sublingual gland associated with Sjögren’s syndrome. Indian J Cancer. 2011;48:381–383.
Kumar AN, Nair PP, Thomas S, Raman PS, Bhambal A. Mucoepidermoid carcinoma of sublingual gland: a malignant neoplasm in an uncommon region. BMJ Case Rep. 2011;12:2011.
López-Quiles J, Ferreira E, Jiménez-Heffernan JA, Del Canto M. Clear cell carcinoma of the major salivary glands in an HIV-infected patient. Int J Oral Maxillofac Surg. 2011;40(7):760–763.
Zdanowski RR. Sublingual gland tumors: clinical, pathologic, and therapeutic analysis of 13 patients treated in a single institution. Head Neck. 2011;33(4):476–481.
Gadre S, Ryan MW, Logroño R. MALT lymphoma of the floor of the mouth: a case report. Ear Nose Throat J. 2009;88(8):E1–E3.
Papadogeorgakis N, Kalfarentzos EF, Vourlakou C, Malta F, Exarhos D. Simultaneous pleomorphic adenoma of the left parotid gland and adenoid cystic carcinoma of the contralateral sublingual salivary gland: a case report. Oral Maxillofac Surg. 2009;13(4):221–224.
Weinreb I, Seethala RR, Perez-Ordoñez B, Chetty R, Hoschar AP, Hunt JL. Oncocytic mucoepidermoid carcinoma: clinicopathologic description in a series of 12 cases. Am J Surg Pathol. 2009;33(3):409–416.
Kwon YD, Biesterfeld S, Hansen T, Schwerdtfeger A, Kunkel M. Lymphadenomatous carcinoma of the sublingual gland: report of a first case in an unusual localization. Head Neck. 2008;30(10):1394–1398.
Saito M, Nishiyama H, Maruyama S, Oda Y, Saku T, Hayashi T. Adenoid cystic carcinoma of sublingual gland involving the submandibular duct. Dentomaxillofac Radiol. 2008;37(7):421–424.
Yamada S, Matsuo T, Baba N, Rokutanda S, Kawasaki G, Mizuno A, Fujita S. High-grade papillary cystadenocarcinoma of the sublingual gland: a case report. J Oral Maxillofac Surg. 2007;65(6):1223–1227.
Yu T, Gao QH, Wang XY, Wen YM, Li LJ. Malignant sublingual gland tumors: a retrospective clinicopathologic study of 28 cases. Int Soc Cell. 2007;72(1–2):39–44.
Maruya S, Namba A, Matsubara A, et al. Salivary gland carcinoma treated with concomitant chemoradiation with intraarterial cisplatin and docetaxel. Int J Clin Oncol. 2006;11(5):403–406.
da Cruz Perez DE, Pires FR, Alves FA, Almeida OP, Kowalski LP. Sublingual salivary gland tumors: clinicopathologic study of six cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:449–453.
Gurney TA, Eisele DW, Weinberg V, Shin E, Lee N. Adenoid cystic carcinoma of the major salivary glands treated with surgery and radiation. Laryngoscope. 2005;115(7):1278–1282.
Matsuzaka K, Shibahara T, Murakami S, Lee DH, Shimono M, Inoue T. Acinic cell carcinoma found by recurrence of a mucous cyst in the sublingual gland. Bull Tokyo Dent Coll. 2004;45(2):95–98.
Shigematsu H, Magoshi S, Suzuki S, Kusama K, Sakashita H. An apparent radiation-induced carcinoma of the parotid gland following treatment for adenoid cystic carcinoma of the sublingual gland: a case report. J Oral Maxillofac Surg. 2004;62(9):1169–1174.
Ogawa I, Sato S, Kudo Y, Miyauchi M, Sugiyama M, Suei Y, Takata T. Solitary fibrous tumor with malignant potential arising in sublingual gland. Pathol Int. 2003;53(1):40–45.
Ota Y, Arai I, Aoki T, Yamazaki H, Karakida K, Tsukinoki K. Acinic cell carcinoma of the sublingual gland accompanied by bone formation. Tokai J Exp Clin Med. 2001;26(4–6):127–130.
Ma’aita JK, Al-Kaisi N, Al-Tamimi S, Wraikat A. Salivary gland tumors in Jordan: a retrospective study of 221 patients. Croat Med J. 1999;40(4):539–542.
Blanchaert RH, Ord RA, Kumar D. Polymorphous low-grade adenocarcinoma of the sublingual gland. Int J Oral Maxillofac Surg. 1998;27(2):115–117.
Foss RD, Ellis GL, Auclair PL. Salivary gland cystadenocarcinomas. A clinicopathologic study of 57 cases. Am J Surg Pathol. 1996;20(12):1440–1447.
Krogdahl AS, Schou C. Mucinous adenocarcinoma of the sublingual gland. J Oral Pathol Med. 1997;26(4):198–200.
McFall MR, Irvine GH, Eveson JW. Adenoid cystic carcinoma of the sublingual salivary gland in a 16-year-old female–report of a case and review of the literature. J Laryngol Otol. 1997;111(5):485–488.
Sakashita H, Miyata M, Miyamoto H, Minato H. Adenocarcinoma originating in the sublingual gland: report of a case. J Oral Maxillofac Surg. 1997;55(7):764–767.
Mima T, Shirasuna K, Kishino M, Matsuya T. Basal cell adenocarcinoma of the sublingual gland: report of a case. J Oral Maxillofac Surg. 1996;54(9):1121–1123.
Whear NM, Addy JM. Adenoid cystic carcinoma of the sublingual gland—an unusual presentation. Br J Oral Maxillofac Surg. 1993;31(2):113–116.
Williams TP, Vincent SD, Connor FA Jr. A mass in the floor of the mouth. J Oral Maxillofac Surg. 1993;51(12):1385–1388.
Danford M, Eveson JW, Flood TR. Papillary cystadenocarcinoma of the sublingual gland presenting as a ranula. Br J Oral Maxillofac Surg. 1992;30(4):270–272.
Uchiyama K, Ikeuchi S, Shiba H, Okada Y, Asanami S. Adenocarcinoma of the sublingual gland. Keio J Med. 1991;40(1):20–24.
Hamper K, Brügmann M, Caselitz J, et al. Prognosis of salivary adenocarcinomas. A retrospective study of 52 cases with special regard to cytochemically assessed nuclear DNA content. Virchows Arch A Pathol Anat Histopathol. 1989;416(1):57–64.
Schwartz-Arad D, Azaz B, Shteyer A. Malignant lymphoma arising in the submandibular and sublingual salivary glands: report of cases. J Oral Maxillofac Surg. 1987;45(9):795–799.
Anonsen C, Dobie RA, Hoekema D, Huang TW, Gown AM. Carcinosarcoma of the floor of mouth. J Otolaryngol. 1985;14(4):215–220.
Nishijima W, Tokita N, Takooda S, Tsuchiya S, Watanabe I. Adenocarcinoma of the sublingual gland: case report and 50 year review of the literature. Laryngoscope. 1984;94(1):96–101.
van den Akker HP, Busemann-Sokole E, Becker AE. Acinic cell carcinoma of the sublingual gland. Scintigraphy in pre-operative evaluation. Int J Oral Surg. 1981;10(5):363–366.
Shidnia H, Hornback NB, Hamaker R, Lingeman R. Carcinoma of major salivary glands. Cancer. 1980;45(4):693–697.
Spiro RH, Huvos AG, Strong EW. Malignant mixed tumor of salivary origin: a clinicopathologic study of 146 cases. Cancer. 1977;39(2):388–396.
Glanzmann C, Aberle HG, Burgener F, Willi F, Horst W. Radiotherapy of salivary gland carcinomas (results from 80 patients). Strahlentherapie. 1976;152(5):395–403.
Main JH, Orr JA, McGurk FM, McComb RJ, Mock D. Salivary gland tumors: review of 643 cases. J Oral Pathol. 1976;5(2):88–102.
Washizu K. Salivary Gland Tumors. In: Takeda C, Nakahara K, editors. Toukeibu Shuyo Zufu. Tokyo: Nakayama-Shoten; 1996. p. 231–233.
Ito T. Adenoid cystic carcinoma of the left sublingual gland. Jpn J Oral Surg. 1974;20:315.
Ramsden D, Sheridan BF, Newton NC, De Wilde FW. Adenoid cystic carcinoma of the head and neck: a report of 30 cases. Aust N Z J Surg. 1973;43(2):102–108.
Furuichi N, et al. A malignant mixed tumor of the sublingual gland. Otolaryngology. 1972;44:41–45.
Rankow RM, Mignogna F. Cancer of the sublingual salivary gland. Am J Surg. 1969;118(5):790–795.
Suzuki H, Henderson R. Acinic cell carcinoma of the sublingual gland. Arch Otolaryngol. 1968;87(2):146–149.
Rosenfeld L, Sessions DG, McSwain B, Graves H Jr. Malignant tumors of salivary gland origin: 37-year review of 184 cases. Ann Surg. 1966;163(5):726–735.
Smith LC, Lane N, Rankow RM. Cylindroma (adenoid cystic carcinoma). A report of fifty-eight cases. Am J Surg. 1965;110(4):519–526.
Luccioli GM, Clement H, Palmer JD. An analysis of 50 carcinomas of the salivary glands. Can J Surg. 1965;8(4):389–399.
Gore DO, Annamunthodo H, Harland A. Tumors of salivary gland origin. Surg Gynecol Obstet. 1964;119:1290–1296.
Bandini A, La Maccia E. Cylindroma of the sublingual gland. Riforma Med. 1962;76:889–892.
Grage TB, Lober PH. Malignant tumors of the major salivary glands. Surgery. 1962;52:284–294.
Wang CP, Chang YL, Ko JY, et al. Lymphoepithelial carcinoma versus large cell undifferentiated carcinoma of the major salivary glands. Cancer. 2004;101:2020–2027.
Manganaris A, Patakiouta F, Xirou P, Manganaris T. Lymphoepithelial carcinoma of the parotid gland: is an association with Epstein-Barr virus possible in non-endemic areas? Int J Oral Maxillofac Surg. 2007;36:556–559.
Hamilton-Dutoit SJ, Therkildsen MH, Nielsen NG, et al. Undifferentiated carcinoma of the salivary gland in Greenlandic Eskimos: demonstration of Epstein-Barr virus DNA in situ hybridization. Hum Pathol. 1991;22:811–815.
Singhi AD, Stelow EB, Mills SE, Westra WH. Lymphoepithelial-like carcinoma of the oropharynx, a morphologic variant of HPV-related head and neck carcinoma. Am J Surg Pathol. 2010;34:800–805.
Barnes L, Eveson JW, Reichart P, Sidransky D, editors. World Health Organization Classification of Tumours. Pathology and Genetics of Head and Neck Tumours. Lyon, France: IARC Press; 2005. p. 200–249.
French CA, Ramirez CL, Kolmakova J, et al. BRD-NUT oncoproteins: a family of closely related nuclear proteins that block epithelial differentiation and maintain the growth of carcinoma cells. Oncogene. 2008;27:2237–2242.
Filippakopoulos P, Qi J, Picaud S, et al. Selective inhibition of BET bromodomains. Nature. 2010;468:1067–1073.
Reynoird N, Schwartz BE, Delvecchio M, et al. Oncogenesis by sequestration of CBP/p300 in transcriptionally inactive hyperacetylated chromatin domains. EMBO J. 2010;29:2943–2952.
Schwartz BE, Hofer MD, Lemieux ME, et al. Differentiation of NUT midline carcinoma by epigenomic reprogramming. Cancer Res. 2011;71:2686–2696.
Funding
There was no external funding for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Nolan Seim declares that he has no conflict of interest. Ramez Phillips declares he has no conflict of interest. Lynn Schoenfield declares that she has no conflict of interest. Theodoros Teknos declares that he has no conflict of interest. James Rocco declares that he has no conflict of interest. Amit Agrawal declares that he has no conflict of interest. Enver Ozer declares that he has no conflict of interest. Ricardo Carrau declares that he has no conflict of interest. Stephen Kang declares that he has no conflict of interest. Matthew Old declares that he has no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Not indicated for this study.
Rights and permissions
About this article
Cite this article
Seim, N.B., Philips, R.H.W., Schoenfield, L. et al. NUT Midline Carcinoma of the Sublingual Gland: Clinical Presentation and Review. Head and Neck Pathol 11, 460–468 (2017). https://doi.org/10.1007/s12105-017-0809-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12105-017-0809-y