Abstract
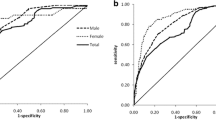
Neck circumference is a new anthropometric index for estimating obesity. We aimed to determine the relationship between neck circumference and body fat content and distribution as well as the efficacy of neck circumference for identifying visceral adiposity and metabolic disorders. A total of 1943 subjects (783 men, 1160 women) with a mean age of 58 ± 7 years were enrolled in this cross-sectional study. Metabolic syndrome was defined according to the standard in the 2013 China Guideline. Analyses were conducted to determine optimal neck circumference cutoff points for visceral adiposity quantified by magnetic resonance imaging, and to compare the performance of neck circumference with that of waist circumference in identifying abdominal obesity and metabolic disorders. Visceral fat content was independently correlated with neck circumference. Receiver operating characteristic curves showed that the area under the curve for the ability of neck circumference to determine visceral adiposity was 0.781 for men and 0.777 for women. Moreover, in men a neck circumference value of 38.5 cm had a sensitivity of 56.1 % and specificity of 83.5 %, and in women, a neck circumference value of 34.5 cm had a sensitivity of 58.1 % and specificity of 82.5 %. These values were the optimal cutoffs for identifying visceral obesity. There were no statistically significant differences between the proportions of metabolic syndrome and its components identified by an increased neck circumference and waist circumference. Neck circumference has the same power as waist circumference for identifying metabolic disorders in a Chinese population.


Similar content being viewed by others
References
K.A. Britton, J.M. Massaro, J.M. Murabito, B.E. Kreger, U. Hoffmann, C.S. Fox, Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J. Am. Coll. Cardiol. 62(10), 921–925 (2013)
G.R. Hajer, T.W. van Haeften, F.L. Visseren, Adipose tissue dysfunction in obesity, diabetes, and vascular diseases. Eur. Heart. J. 29(24), 2959–2971 (2008)
A. Shuster, M. Patlas, J.H. Pinthus, M. Mourtzakis, The clinical importance of visceral adiposity: a critical review of methods for visceral adipose tissue analysis. Br. J. Radiol. 85(1009), 1–10 (2012)
A. Onat, G.S. Avci, M.M. Barlan, H. Uyarel, B. Uzunlar, V. Sansoy, Measures of abdominal obesity assessed for visceral adiposity and relation to coronary risk. Int. J. Obes. Relat. Metab. Disord. 28(8), 1018–1025 (2004)
J.C. Seidell, A. Oosterlee, P. Deurenberg, J.G. Hautvast, J.H. Ruijs, Abdominal fat depots measured with computed tomography: effects of degree of obesity, sex, and age. Eur. J. Clin. Nutr. 42(9), 805–815 (1988)
K.G. Alberti, R.H. Eckel, S.M. Grundy, P.Z. Zimmet, J.I. Cleeman, K.A. Donato, J.C. Fruchart, W.P. James, C.M. Loria, S.C. Smith Jr; International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity, Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 120(16), 1640–1645 (2009)
P. Zimmet, D. Magliano, Y. Matsuzawa, G. Alberti, J. Shaw, The metabolic syndrome: A global public health problem and a new definition. J. Atheroscler. Thromb. 12(6), 295–300 (2005)
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and Treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation 106(25), 3143–3421 (2002)
C. Stabe, A.C. Vasques, M.M. Lima, M.A. Tambascia, J.C. Pareja, A. Yamanaka, B. Geloneze, Neck circumference as a simple tool for identifying the metabolic syndrome and insulin resistance: results from the Brazilian metabolic syndrome study(BRAMS). Clin. Endocrinol. (Oxf). 78(6), 874–881 (2013)
M.R. Hingorjo, M.A. Qureshi, A. Mehdi, Neck circumference as a useful marker of obesity: a comparison with body mass index and waist. J. Pak. Med. Assoc. 62(1), 36–40 (2012)
K.V. Fitch, T.L. Stanley, S.E. Looby, A.M. Rope, S.K. Grinspoon, Relationship between neck circumference and cardiometabolic parameters in HIV-infected and non-HIV-infected adults. Diabetes Care. 34(4), 1026–1031 (2011)
G.R. Yang, S.Y. Yuan, H.J. Fu, G. Wan, L.X. Zhu, X.L. Bu, J.D. Zhang, X.P. Du, Y.L. Li, Y. Ji, X.N. Gu, Y. Li, Beijing community diabetes study group, neck circumference positively related with central obesity, overweight, and metabolic syndrome in Chinese subjects with type 2 diabetes: Beijing community diabetes study 4. Diabetes Care. 33(11), 2465–2467 (2010)
Y. Dai, X. Wan, X. Li, E. Jin, X. Li, Neck circumference and future cardiovascular events in a high-risk population—a prospective cohort study. Lipids. Health. Dis. 15, 46 (2016)
S.R. Preis, J.M. Massaro, U. Hoffmann, R.B. D’Agostino Sr, D. Levy, S.J. Robins, J.B. Meigs, R.S. Vasan, C.J. O’Donnell, C.S. Fox, Neck circumference as a novel measure of cardiometabolic risk: the framingham heart study. J. Clin. Endocrinol. Metab. 95(8), 3701–3710 (2010)
A. Onat, G. Hergenç, H. Yüksel, G. Can, E. Ayhan, Z. Kaya, D. Dursunoğlu, Neck circumference as a measure of central obesity: associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin. Nutr. 28(1), 46–51 (2009)
H.X. Li, F. Zhang, D. Zhao, Z. Xin, S.Q. Guo, S.M. Wang, J.J. Zhang, J. Wang, Y. Li, G.R. Yang, J.K. Yang, Neck circumference as a measure of neck fat and abdominal visceral fat in Chinese adults. BMC Public Health 14, 311 (2014)
Y. Wang, X. Ma, M. Zhou, W. Zong, L. Zhang, Y. Hao, J. Zhu, Y. Xiao, D. Li, Y. Bao, W. Jia, Contribution of visceral fat accumulation to carotid intima-media thickness in a Chinese population. Int. J. Obes. (Lond). 36(9), 1203–1208 (2012)
J. Weng, L. Ji, W. Jia, J. Lu, Z. Zhou, D. Zou, D. Zhu, L. Chen, L. Chen, L. Guo, X. Guo, Q. Ji, Q. Li, X. Li, J. Liu, X. Ran, Z. Shan, L. Shi, G. Song, L. Yang, Y. Yang, W. Yang, Chinese diabetes society, standards of care for type 2 diabetes in China. Diabetes Metab. Res. Rev. 32(5), 442–458 (2016)
National Health and Family Planning Commission of the People’s Republic of China. Criteria of Weight for Adults. (Standards Press of China, Beijing, 2013), pp. 1–8
Y. Bao, J. Lu, C. Wang, M. Yang, H. Li, X. Zhang, J. Zhu, H. Lu, W. Jia, K. Xiang, Optimal waist circumference cutoffs for abdominal obesity in Chinese. Atherosclerosis. 201(2), 378–384 (2008)
N.G. Vallianou, A.A. Evangelopoulos, V. Bountziouka, E.D. Vogiatzakis, M.S. Bonou, J. Barbetseas, P.C. Avgerinos, D.B. Panagiotakos, Neck circumference is correlated with triglycerides and inversely related with HDL cholesterol beyond BMI and waist circumference. Diabetes Metab. Res. Rev. 29(1), 90–97 (2013)
K. Joshipura, F. Muñoz-Torres, J. Vergara, C. Palacios, C.M. Pérez, Neck circumference may be a better alternative to standard anthropometric measures. J. Diabetes Res. 2016, 6058916 (2016)
G. Cizza, L. de Jonge, P. Piaggi, M. Mattingly, X. Zhao, E. Lucassen, K.I. Rother, A.E. Sumner, G. Csako, NIDDK sleep extension study, neck circumference is a predictor of metabolic syndrome and obstructive sleep apnea in short-sleeping obese men and women. Metab. Syndr. Relat. Disord. 12(4), 231–241 (2014)
M. Khalangot, V. Gurianov, N. Okhrimenko, I. Luzanchuk, V. Kravchenko, Neck circumference as a risk factor of screen-detected diabetes mellitus: community-based study. Diabetol. Metab. Syndr. 8, 12 (2016)
L.L. Ben-Noun, A. Laor, Relationship between changes in neck circumference and cardiovascular risk factors. Exp. Clin. Cardiol. 11(1), 14–20 (2006)
L. Yang, Y.P. Sa marasinghe, P. Kane, S.A. Amiel, S.J. Aylwin, Visceral adiposity is closely correlated with neck circumference and represents a significant indicator of insulin resistance in WHO grade III obesity. Clin. Endocrinol. (Oxf). 73(2), 197–200 (2010)
T.S. Han, N. Sattar, M. Lean, ABC of obesity. Assessment of obesity and its clinical implications. BMJ. 333(7570), 695–698 (2006)
E. Maddaloni, I. Cavallari, M. De Pascalis, H. Keenan, K. Park, S. Manfrini, R. Buzzetti, G. Patti, G. Di Sciascio, P. Pozzilli, Relation of body circumferences to cardiometabolic disease in overweight-obese subjects. Am. J. Cardiol. 118(6), 822–887 (2016)
G. Jamar, L.P. Pisani, L.M. Oyama, C. Belote, D.C. Masquio, V.A. Furuya, J.P. Carvalho-Ferreira, S.G. Andrade-Silva, A.R. Dâmaso, D.A. Caranti, Is the neck circumference an emergent predictor for inflammatory status in obese adults? Int. J. Clin. Pract. 67(3), 217–224 (2013)
S. Hoebel, L. Malan, J.H. de Ridder, Determining cut-off values for neck circumference as a measure of the metabolic syndrome amongst a South African cohort: the SABPA study. Endocrine. 42(2), 335–342 (2012)
S. Hoebel, L. Malan, J. Botha, M. Swanepoel, Optimizing waist circumference cut-points for the metabolic syndrome and its components in a South African cohort at 3 year follow-up: the SABPA prospective cohort. Endocrine. 47(3), 959–961 (2014)
M. Hastedt, M. Büchner, M. Rothe, R. Gapert, S. Herre, F. Krumbiegel, M. Tsokos, T. Kienast, A. Heinz, S. Hartwig, Detecting alcohol abuse: traditional blood alcohol markers compared to ethyl glucuronide (EtG) and fatty acid ethyl esters (FAEEs) measurement in hair. Forensic Sci. Med. Pathol 9(4), 471–477 (2013)
Acknowledgments
We appreciate the efforts of all participants who contributed to sample measurements and data collections.
Funding
This work was funded by the 973 Program of China (2013CB530606), the Grant from Shanghai Health and Family Planning Commission (2013ZYJB1001), and the Translational Medicine Innovation Foundation of School of Medicine Shanghai Jiao Tong University (15ZH2010 and 15ZH4006).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study protocol was reviewed and approved by the Ethics Committee of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, and all procedures were performed in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
The study methods and potential risks were fully explained to all participants, and each participant provided a written informed consent prior to enrollment.
Additional information
Yuqi Luo and Xiaojing Ma contributed equally to this work.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Luo, Y., Ma, X., Shen, Y. et al. Neck circumference as an effective measure for identifying cardio-metabolic syndrome: a comparison with waist circumference. Endocrine 55, 822–830 (2017). https://doi.org/10.1007/s12020-016-1151-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-1151-y