Abstract
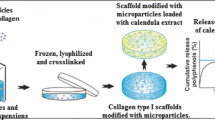
Platelet lysate (PL) was encapsulated in collagen (Coll) millimetric gel beads, on biomimetic superhydrophobic surfaces, under mild conditions, with the aim of obtaining easy-to-handle formulations able to provide sustained release of multiple growth factors for skin ulcers treatment. The gel particles were prepared with various concentrations of PL incorporating or not stem cells, and tested as freshly prepared or after being freeze-dried or cryopreserved. Coll + PL particles were evaluated regarding degradation in collagenase-rich environment (simulating the aggressive environment of the chronic ulcers), sustained release of total protein, PDGF-BB and VEGF, cell proliferation (using particles as the only source of growth factors), scratch wound recovery and angiogenic capability. Compared to Coll solely particles, incorporation of PL notably enhanced cell proliferation (inside and outside gels) and favored scratch wound recovery and angiogenesis. Moreover, cell-laden gel particles containing PL notably improved cell proliferation and even migration of cells from one particle towards a neighbor one, which led to cell-cell contacts and the spontaneous formation of tissue layers in which the spherical gels were interconnected by the stem cells.













Similar content being viewed by others
References
Sen, C. K., Gordillo, G. M., Roy, S., et al. (2010). Human skin wounds: a major and snowballing threat to public health and economy. Wound Repair and Regeneration, 17, 763–771.
Nathan, C. F. (1987). Secretory products of macrophages. Journal of Clinical Investigation, 79, 319–326.
Tonnesen, M. G., Feng, X., & Clark, R. A. F. (2000). Angiogenesis in wound healing. Journal of Investigative Dermatology Symposium Proceedings, 5, 40–46.
Helary, C., Zarka, M., & Giraud-Guille, M. M. (2012). Fibroblasts within concentrated collagen hydrogels favour chronic skin wound healing. Journal of Tissue Engineering and Regenerative Medicine, 6, 225–237.
Bir, S. C., Esaki, J., Marui, A., et al. (2011). Therapeutic treatment with sustained-release platelet-rich plasma restores blood perfusion by augmenting ischemia-induced angiogenesis and arteriogenesis in diabetic mice. Journal of Vascular Research, 48, 195–205.
Brem, H., Balledux, J., Bloom, T., Kerstein, M. D., & Hollier, L. (2000). Healing of diabetic foot ulcers and pressure ulcers with human skin equivalent. Archives of Surgery, 135, 627–634.
Murray, M. M., Spindler, K. P., Abreu, E., et al. (2007). Collagen-platelet rich plasma hydrogel enhances primary repair of the porcine anterior cruciate ligament. Journal of Orthopaedic Research, 25, 81–91.
Hokugo, A., Ozeki, M., Kawakami, O., et al. (2005). Augmented bone regeneration activity of platelet-rich plasma by biodegradable gelatin hydrogel. Tissue Engineering, 11, 1224–1233.
Moreira Teixeira, L. S., Leijten, J. C. H., Wennink, J. W. H., et al. (2012). The effect of platelet lysate supplementation of a dextran-based hydrogel on cartilage formation. Biomaterials, 33, 3651–3661.
Bhang, S. H., Park, J., Yang, H. S., Shin, J., & Kim, B. S. (2013). Platelet-rich plasma enhances the dermal regeneration efficacy of human adipose-derived stromal cells administered to skin wounds. Cell Transplantation, 22, 437–445.
Anitua, E., Muruzabal, F., Alcalde, I., Merayo-Lloves, J., & Orive, G. (2013). Plasma rich in growth factors (PRGF-Endoret) stimulates corneal wound healing and reduces haze formation after PRK surgery. Experimental Eye Research, 115, 153–61.
Albanese, A., Licata, M. E., Polizzi, B., & Campisi, G. (2013). Platelet-rich plasma (PRP) in dental and oral surgery: from the wound healing to bone regeneration. Immunity & Ageing, 10, 23–33.
Sell, S. A., Ericksen, J. J., Reis, T. W., Droste, L. R., Bhuiyan, M. B. A., & Gater, D. R. (2011). A case report on the use of sustained release platelet-rich plasma for the treatment of chronic pressure ulcers. Journal of Spinal Cord Medicine, 34, 122–127.
Hildner, F., Albrecht, C., Gabriel, C., Redl, H., & van Griensven, M. (2011). State of the art and future perspectives of articular cartilage regeneration: a focus on adipose-derived stem cells and platelet-derived products. Journal of Tissue Engineering and Regenerative Medicine, 5, e36–e51.
Foster, T. E., Puskas, B. L., Mandelbaum, B. R., Gerhardt, M. B., & Rodeo, S. A. (2009). Platelet-rich plasma: from basic science to clinical applications. American Journal of Sports Medicine, 37, 2259–2272.
Lu, H. H., Vo, J. M., Chin, H. S., et al. (2008). Controlled delivery of platelet-rich plasma-derived growth factors for bone formation. Journal of Biomedical Materials Research. Part A, 86, 1128–1136.
Mori, M., Rossi, S., Bonferoni, M. C., et al. (2014). Calcium alginate particles for the combined delivery of platelet lysate and vancomycin hydrochloride in chronic skin ulcers. International Journal of Pharmaceutics, 461, 505–513.
Man, Y., Wang, P., Guo, Y., et al. (2012). Angiogenic and osteogenic potential of platelet-rich plasma and adipose-derived stem cell laden alginate microspheres. Biomaterials, 33, 8802–8811.
Matsui, M., & Tabata, Y. (2012). Enhanced angiogenesis by multiple release of platelet-rich plasma contents and basic fibroblast growth factor from gelatin hydrogels. Acta Biomaterialia, 8, 1792–1801.
Walter, M. N. M., Wright, K. T., Fuller, H. R., MacNeil, S., & Johnson, W. E. B. (2010). Mesenchymal stem cell-conditioned medium accelerates skin wound healing: an in vitro study of fibroblast and keratinocyte scratch assays. Experimental Cell Research, 316, 1271–1281.
Song, W., Lima, A. C., & Mano, J. F. (2010). Bioinspired methodology to fabricate hydrogel spheres for multi-applications using superhydrophobic substrates. Soft Matter, 6, 5868–5871.
Oliveira, N. M., Neto, A. I., Song, W., & Mano, J. F. (2010). Two-dimensional open microfluidic devices by tuning the wettability on patterned superhydrophobic polymeric surface. Applied Physics Express, 3, 085205.
Lima, A. C., Song, W., Blanco-Fernandez, B., Alvarez-Lorenzo, C., & Mano, J. F. (2011). Synthesis of temperature-responsive dextran-MA/PNIPAAm particles for controlled drug delivery using superhydrophobic surfaces. Pharmaceutical Research, 28, 1294–1305.
Lima, A. C., Batista, P., Valente, T. A. M., Silva, A. S., Correia, I. J., & Mano, J. F. (2013). Novel methodology based on biomimetic superhydrophobic substrates to immobilize cells and proteins in hydrogel spheres for applications in bone regeneration. Tissue Engineering Part A, 19, 1175–1187.
Lima, A. C., Custódio, C. A., Alvarez-Lorenzo, C., & Mano, J. F. (2013). Biomimetic methodology to produce polymeric multilayered particles for biotechnological and biomedical applications. Small, 9, 2487–2492.
Lima, A. C., Correia, C. R., Oliveira, M. B., & Mano, J. F. (2013). Sequential ionic and thermogelation of chitosan spherical hydrogels prepared using superhydrophobic surfaces to immobilize cells and drugs. Journal of Bioactive and Compatible Polymers, 29, 50–65.
Liang, C. C., Park, A. Y., & Guan, J. L. (2007). In vitro scratch assay: a convenient and inexpensive method for analysis of cell migration in vitro. Nature Protocols, 2, 329–333.
Ghazi, K., Deng-Pichon, U., Warnet, J. M., & Rat, P. (2012). Hyaluronan fragments improve wound healing on in vitro cutaneous model through P2X7 purinoreceptor basal activation: role of molecular weight. PloS One, 7, e48351.
Chan, B. P., Hui, T. Y., Yeung, C. W., Li, J., Mo, I., & Chan, G. C. F. (2007). Self-assembled collagen-human mesenchymal stem cell microspheres for regenerative medicine. Biomaterials, 28, 4652–4666.
Bao, P., Kodra, A., Tomic-Canic, M., Golinko, M. S., Ehrlich, H. P., & Brem, H. (2009). The role of vasvular endothelial growth factor in wound healing. Journal of Surgical Research, 153, 347–358.
Agren, M. S., Steenfos, H. H., Dabelsteen, S., Hansen, J. B., & Dabelsteen, E. (1999). Proliferation and mitogenic response to PDGF-BB of fibroblasts isolated from chronic venous leg ulcers is ulcer-age dependent. Journal of Investigative Dermatology, 112, 463–469.
Steed, D. L. (1995). Clinical evaluation of recombinant human platelet-derived growth factor for the treatment of lower extremity diabetic ulcers. Journal of Vascular Surgery, 21, 71–80.
Smiell, J. M., Wirman, T. J., Steed, D. L., Perry, B. H., Sampson, A. R., & Schwab, B. H. (1999). Efficacy and safety of becaplermin (recombinant human platelet-derived growth factor-BB) in patients with nonhealing, lower extremity diabetic ulcers: a combined analysis of four randomized studies. Wound Repair and Regeneration, 7, 335–346.
Ito, R., Morimoto, N., Pham, L. H., Taira, T., Kaway, K., & Suzuki, S. (2013). Efficacy of the controlled release of concentrated platelet lysate from a collagen/gelatin scaffold for dermis-like tissue regeneration. Tissue Engineering Part A, 19, 1398–1405.
Pietramaggiori, G., Kaipainen, A., Czeczuga, J. M., Wagner, C. T., & Orgill, D. P. (2006). Freeze-dried platelet-rich plasma shows beneficial healing properties in chronic wounds. Wound Repair and Regeneration, 14, 573–580.
O’Leary, L. E. R., Fallas, J. A., Bakota, E. L., Kang, M. K., & Hartgerink, J. D. (2011). Multi-hierarchical self-assembly of a collagen mimetic peptide from triple helix to nanofibre and hydrogel. Nature Chemistry, 3, 821–828.
Kadler, K. E., Holmes, D. F., Trotter, J. A., & Chapman, J. A. (1996). Collagen fibril formation. Biochemistry Journal, 316, 1–11.
George, A., & Veis, A. (1991). FTIRS in H2O demonstrates that collagen monomers undergo a conformational transition prior to thermal self-assembly in vitro. Biochemistry, 30, 2372–2377.
Li, Y., Asadi, A., Monroe, M. R., & Douglas, E. P. (2009). pH effects on collagen fibrillogenesis in vitro: electrostatic interactions and phosphate binding. Materials Science and Engineering C, 29, 1643–1649.
Abou Neel, E. A., Bozec, L., Knowles, J. C., et al. (2013). Collagen-emerging collagen based therapies hit the patient. Advanced Drug Delivery Reviews, 65, 429–456.
Fufa, D., Shealy, B., Jacobson, M., Kevy, S., & Murray, M. M. (2008). Activation of platelet-rich plasma using soluble type I collagen. Journal of Oral and Maxillofacial Surgery, 66, 684–690.
Alsousou, J., Thompson, M., Hulley, P., Noble, A., & Willett, K. (2009). The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. Journal of Bone and Joint Surgery (British), 91, 987–996.
Puga, A. M., Lima, A. C., Mano, J. F., Concheiro, A., & Alvarez-Lorenzo, C. (2013). Pectin-coated chitosan microgels crosslinked on superhydrophobic surfaces for 5-fluorouracil encapsulation. Carbohydrate Polymers, 98, 331–340.
Costa, A. M. S., Alatorre-Meda, M., Oliveira, N. M., & Mano, J. F. (2014). Biocompatible polymeric microparticles produced by a simple biomimetic approach. Langmuir, 30, 4535–4539.
Crevensten, G., Walsh, A. J. L., Ananthakrishnan, D., et al. (2004). Intervertebral disc cell therapy for regeneration: mesenchymal stem cell implantation in rat intervertebral discs. Annals of Biomedical Engineering, 32, 430–434.
Humes, H. D. (2005). Stem cells: the next therapeutic frontier. Transactions of the American Clinical and Climatological Association, 116, 167–184.
Yu, J., Du, K. T., Fang, Q., et al. (2010). The use of human mesenchymal stem cells encapsulated in RGD modified alginate microspheres in the repair of myocardial infarction in the rat. Biomaterials, 31, 7012–7020.
Ruszczak, Z. (2003). Effect of collagen matrices on dermal wound healing. Advanced Drug Delivery Reviews, 55, 1595–1611.
Lima, A. C., Sher, P., & Mano, J. F. (2012). Production methodologies of polymeric and hydrogel particles for drug delivery applications. Expert Opinion on Drug Delivery, 9, 231–248.
Ebrahimian, T. G., Pouzoulet, F., Squiban, C., et al. (2009). Cell therapy based on adipose tissue-derived stromal cells promotes physiological and pathological wound healing. Arteriosclerosis, Thrombosis, and Vascular Biology, 29, 503–510.
Kim, W. S., Park, B. S., Sung, J. H., et al. (2007). Wound healing effect of adipose-derived stem cells: a critical role of secretory factors on human dermal fibroblasts. Journal of Dermatological Science, 2007(48), 15–24.
Sen, C. K. (2009). Wound healing essentials: let there be oxygen. Wound Repair and Regeneration, 17, 1–18.
Bertrand-Duchesne, M. P., Grenier, D., & Gagnon, G. (2010). Epidermal growth factor released from platelet-rich plasma promotes endothelial cell proliferation in vitro. Journal of Periodontal Research, 45, 87–93.
Hsu, C. W., Yuan, K., & Tseng, C. C. (2009). The negative effect of platelet-rich plasma on the growth of human cells is associated with secreted thrombospondin-1. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 107, 185–192.
Backly, R. E., Ulivi, V., Tonachini, L., Cancedda, R., Descalzi, F., & Mastrogiacomo, M. (2011). Platelet lysate induces in vitro wound healing of human keratinocytes associated with a strong proinflammatory response. Tissue Engineering Part A, 17, 1787–1800.
Yannas, I. V., Lee, E., Orgill, D. P., Skrabut, E. M., & Murphy, G. F. (1989). Synthesis and characterization of a model extracellular matrix that induces partial regeneration of adult mammalian skin. Proceedings of the National Academy of Sciences of the United States of America, 86, 933–937.
Soller, E. C., Tzeranis, D. S., Miu, K., So, P. T. C., & Yannas, I. V. (2012). Common features of optimal collagen scaffolds that disrupt wound contraction and enhance regeneration both in peripheral nerves and in skin. Biomaterials, 33, 4783–4791.
Moor, A. N., Vachon, D. J., & Gould, L. J. (2009). Proteolytic activity in wound fluids and tissues derived from chronic venous leg ulcers. Wound Repair and Regeneration, 17, 832–839.
Marx, R. E., Carlson, E. R., Eichstaedt, R. M., Schimmele, S. R., Strauss, J. E., & Georgeff, K.-R. (1998). Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 85, 638–646.
Hokugo, A., Sawada, Y., Hokugo, R., et al. (2007). Controlled release of platelet growth factors enhances bone regeneration at rabbit calvaria. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics, 104, 44–48.
Metcalfe, A. D., & Ferguson, M. W. J. (2007). Tissue engineering of replacement skin: the crossroads of biomaterials, wound healing, embryonic development, stem cells and regeneration. Journal of the Royal Society, Interface, 4, 413–437.
Acknowledgments
A.C. Lima acknowledges to the Portuguese Foundation for Science and Technology (FCT) for the PhD grant SFRH/BD/71395/2010. Work supported by the European Union’s Seventh Framework Programme (FP7/2007-2013) under grant agreement n° REGPOT-CT2012-316331-POLARIS, FEDER through the Competitive Factors Operation Program–COMPETE, Portugal national funds through FCT (PTDC/CTM-BIO/1814/2012), Operational Human Potential Program (POPH) developed under the scope of the National Strategic Reference Framework (QREN) from the European Social Fund (FSE), and Spain MICINN (SAF2011-22771). The authors thank Ibidi for culture inserts samples, Luis Diaz-Gomez and Patricia Días Rodríguez for the help with PL preparation and CAM assay, and Instituto de Ortopedia y Banco de Tejidos Musculoesqueléticos (Universidad de Santiago de Compostela, Spain) for the help with cell cultures.
Notes
The authors declare no potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Lima, A.C., Mano, J.F., Concheiro, A. et al. Fast and Mild Strategy, Using Superhydrophobic Surfaces, to Produce Collagen/Platelet Lysate Gel Beads for Skin Regeneration. Stem Cell Rev and Rep 11, 161–179 (2015). https://doi.org/10.1007/s12015-014-9548-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12015-014-9548-6