Abstract
Background
The Bernese periacetabular osteotomy (PAO) traditionally is performed using the iliofemoral or the ilioinguinal approach with transection of the rectus femoris tendon attachments. Although a rectus-preserving approach has been developed, there is limited direct comparison data regarding the surgical safety, radiographic correction, and improvement in hip pain and function between the rectus-preserving and the classic approaches.
Questions/purposes
The purposes of this study were to determine whether preserving the rectus femoris tendon attachment would (1) reduce intraoperative blood loss and length of surgery; (2) improve Harris hip scores (HHS); (3) decrease the rate of complications; and (4) affect the radiographic correction when compared with the classic approach.
Methods
A retrospective matched cohort study was used to compare the endpoints listed above after PAO using a rectus-preserving approach versus the classic approach. Operative blood loss, preoperative and postoperative hematocrit, duration of surgery, HHS, and postoperative complications were recorded for the two groups. Pelvic radiographs were reviewed for measurement of the lateral center-edge angle, anterior center-edge angle, and Tönnis acetabular inclination angle. A total of 64 patients were included (32 in each group). Followup was at a minimum of 1 year (mean, 20 months; range, 13–44 months).
Results
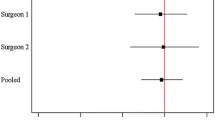
Blood loss (p = 0.2405), hematocrit change (p = 0.3277), and operative time (p = 0.3960) were similar between groups. At latest followup, the HHS improved in the rectus-preserving (mean improvement, 25; 95% CI, 21–29; p < 0.0001) and control groups (mean improvement, 21; 95% CI, 17–25; p < 0.0001) with no difference in HHS improvement between the groups (mean difference, 4.3; 95% CI, −1.6 to 10.1; p = 0.1523). The complication rate was 12.5% (four of 32) in the rectus-preserving group and 25% (eight of 32) in the classic approach groups, respectively (p = 0.2002). The rectus-preserving approach allowed for similar lateral center-edge angle (p = 0.4463), anterior center-edge angle (p = 0.0936), and Tönnis angle (p = 0.7953) improvement when compared with the classic approach.
Conclusions
The rectus-preserving approach for PAO is as safe and effective as the classic approach to achieve radiographic correction and HHS improvement at minimum 1 year. Additional investigation is needed to determine whether the rectus-preserving approach allows for improvement in functional recovery including hip flexion strength.
Level of Evidence
Level III, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.


Similar content being viewed by others
References
Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013;471:1602–1614.
Atwal NS, Bedi G, Lankester BJ, Campbell D, Gargan MF. Management of blood loss in periacetabular osteotomy. Hip Int. 2008;18:95–100.
Centers for Disease Control and Prevention. Defining overweight and obesity. Available at: http://www.cdc.gov/obesity/defining.html. Accessed March 28, 2014.
Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009;467:2041–2052.
Davey JP, Santore RF. Complications of periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:33–37.
Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36.
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755.
Hussell JG, Mast JW, Mayo KA, Howie DW, Ganz R. A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:64–72.
Lee CB, Kalish LA, Millis MB, Kim YJ. Predictors of blood loss and haematocrit after periacetabular osteotomy. Hip Int. 2013;23(suppl 9):S8–13.
Lequesne M, de Sèze S. [False profile of the pelvis: a new radiographic incidence for the study of the hip. Its use in dysplasias and different coxopathies][in French]. Rev Rhum Mal Osteoartic. 1961;28:643–652.
Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009;91:2113–2123.
Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the bernese periacetabular osteotomy and predictors of clinical outcome: surgical technique. J Bone Joint Surg Am. 2010;92(suppl 1 pt 2):115–129.
Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999;364:92–98.
Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99.
Novais EN, Heyworth B, Murray K, Johnson VM, Kim YJ, Millis MB. Physical activity level improves after periacetabular osteotomy for the treatment of symptomatic hip dysplasia. Clin Orthop Relat Res. 2013;471:981–988.
Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239–245.
Siebenrock KA, Steppacher SD, Albers CE, Haefeli PC, Tannast M. Diagnosis and management of developmental dysplasia of the hip from triradiate closure through young adulthood. J Bone Joint Surg Am. 2013;95:748–755.
Sink EL, Leunig M, Zaltz I, Gilbert JC, Clohisy J. Reliability of a complication classification system for orthopaedic surgery. Clin Orthop Relat Res. 2012;470:2220–2226.
Smith-Petersen MN. Approach to and exposure of the hip joint for mold arthroplasty. J Bone Joint Surg Am. 1949;31:40–46.
Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644.
Tannast M, Mistry S, Steppacher SD, Reichenbach S, Langlotz F, Siebenrock KA, Zheng G. Radiographic analysis of femoroacetabular impingement with Hip2Norm-reliable and validated. J Orthop Res. 2008;26:1199–1205.
Tonnis D. General radiograph of the hip joint. In: Tonnis D, ed. Congenital Dysplasia, Dislocation of the Hip. New York, NY:Springer; 1987:100–142.
Troelsen A, Elmengaard B, Soballe K. Comparison of the minimally invasive and ilioinguinal approaches for periacetabular osteotomy: 263 single-surgeon procedures in well-defined study groups. Acta Orthop. 2008;79:777–784.
Troelsen A, Elmengaard B, Soballe K. A new minimally invasive transsartorial approach for periacetabular osteotomy. J Bone Joint Surg Am. 2008;90:493–498.
Troelsen A, Elmengaard B, Soballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009;91:2169–2179.
Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77:73–85.
Trumble SJ, Mayo KA, Mast JW. The periacetabular osteotomy: minimum 2 year followup in more than 100 hips. Clin Orthop Relat Res. 1999;363:54–63.
Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83:28–38.
Acknowledgments
We thank Kerry Murray PA-C (Department of Orthopaedics, Children’s Hospital Boston), and Gloria Boye BA (Department of Orthopaedics, Children’s Hospital Boston) for contributions to data acquisition for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This study was performed at Boston Children’s Hospital, Boston, MA, USA.
About this article
Cite this article
Novais, E.N., Kim, YJ., Carry, P.M. et al. The Bernese Periacetabular Osteotomy: Is Transection of the Rectus Femoris Tendon Essential?. Clin Orthop Relat Res 472, 3142–3149 (2014). https://doi.org/10.1007/s11999-014-3720-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3720-9